Translate this page into:
Fine-needle aspiration cytology of a thyroid nodule: Challenging morphologic considerations
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 32-year-old female presented to the emergency department with fever, sore throat, and swelling of the right neck. A computed tomography scan showed a thyroid nodule measuring 2 cm localized to the right lobe. Ultrasound showed a dominant, complex, partially cystic and solid nodule measuring 2.3 cm × 2.1 cm × 2.0 cm with scattered internal microcalcifications. An ultrasound-guided FNA was performed, and the Papanicolaou and Diff-Quik-stained smears are shown in Figure 1.
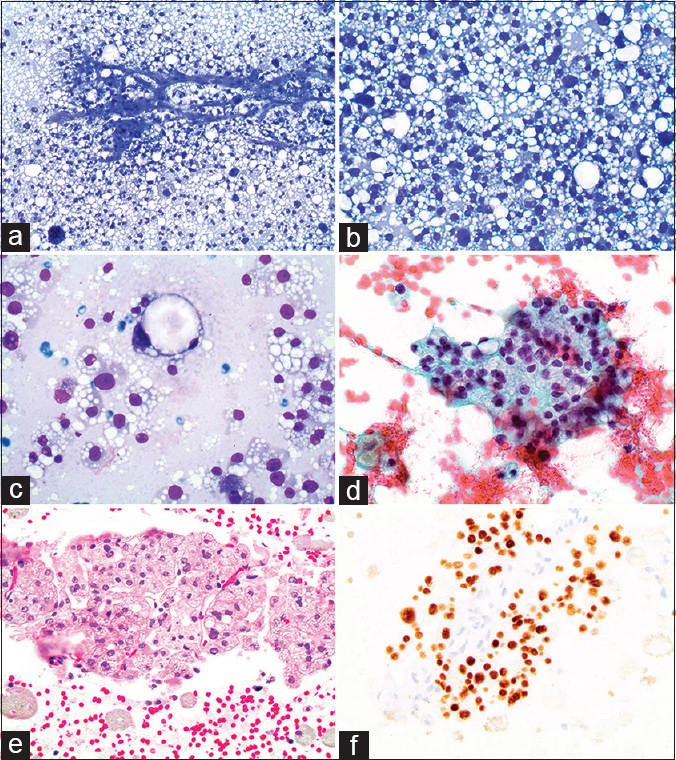
- (a) Cellular smears with numerous epithelioid cells showing clear cytoplasmic vacuoles, and rich vascularity (Diff-Quik, ×200); (b) Rare focus with cellular atypia, nuclear pleomorphism and hyperchromasia (Diff-Quik, ×400). (c) Higher power of a lesional cell with a signet ring appearance (Diff-Quik, ×600); (d) Papanicolaou-stained smear showing a cohesive cluster of cells, two with a signet ring appearance (×400); (e) The cell block was paucicellular but did contain two small groups of lesional cells with interspersed macrophages (H and E, ×200); (f) Immunohistochemical staining for thyroid transcription factor-1 showing positive nuclear staining in the lesional cells (×200). CD68 and CD10 immunohistochemical stains were negative (not shown)
QUESTION
Q1: What is your interpretation of the above findings?
-
Negative for malignancy
-
Suspicious for follicular neoplasm
-
Positive for malignancy, favor metastasis
-
Papillary thyroid carcinoma.
ANSWER
The best answer is “suspicious for follicular neoplasm.” Given the imaging findings of a dominant thyroid nodule along with a cellular aspirate of cohesive clusters of monotonous-appearing cells with atypical cytologic features including hyperchromasia, intracytoplasmic vacuoles, and signet ring cells, a neoplasm is likely.
The finding of signet ring cells in a follicular neoplasm of the thyroid is a rare event.[1] Interpreting these signet ring cells in thyroid cytology specimens is a difficult task, with various metastatic entities, primary thyroid neoplasms, and even benign nonneoplastic lesions, all entering the differential diagnosis. In this case, the pronounced intracytoplasmic vacuoles and prominent vascular network on the FNA smears closely mimicked metastatic clear cell renal cell carcinoma.[2] However, positive immunohistochemical (IHC) staining for TTF-1 and negative staining of CD10 on the cell block section rendered this diagnosis unlikely.
PATIENT FOLLOW-UP
The patient subsequently underwent a total thyroidectomy with limited cervical lymph node dissection without complication. Gross pathologic examination of the thyroid specimen revealed a well-circumscribed tan-yellow nodule within the mid-inferior right lobe measuring 2.7 cm × 2.3 cm × 1.7 cm. Histologically, the nodule was encapsulated and demonstrated a predominantly nested pattern of growth with occasional microfollicular structures and scattered fine vasculature [Figure 2a]. The lesional cells showed numerous fine vacuoles as well as large, clear intracytoplasmic vacuoles imparting a signet ring cell appearance. Mitotic figures were not conspicuous. In addition, an area with marked cellular atypia and nuclear pleomorphism was identified [Figure 2b], similar to the aspirate smears. Mucicarmine [Figure 2e] and Alcian blue stains were negative for mucin. Thyroglobulin was positive in the neoplastic cells [Figure 2f]. The nodule was entirely submitted for microscopic examination. Two foci of vascular invasion within the capsule were identified [Figure 2c], which were confirmed by IHC staining with ERG transcription factor [Figure 2d]. A diagnosis of “follicular thyroid carcinoma with signet ring cells, minimally invasive with vascular invasion” was made. No evidence of lymph node metastasis was identified.
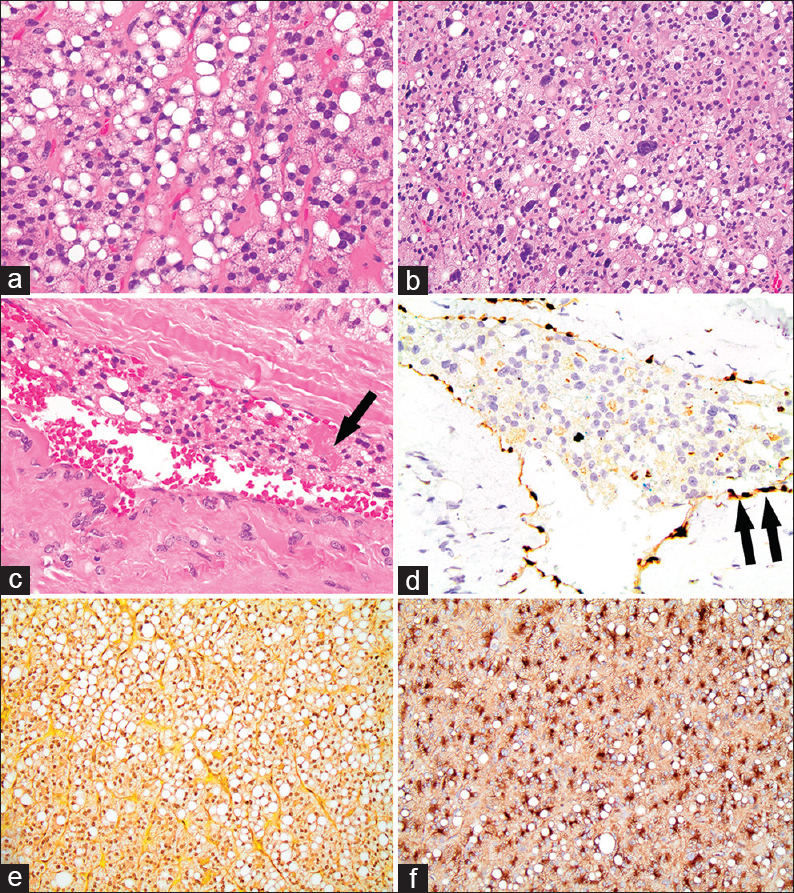
- Histologic features of thyroid follicular carcinoma with signet ring cells. (a) Nested pattern of follicular cells, some with intracytoplasmic vacuoles imparting a signet ring cell appearance, and surrounding fine vasculature (H and E, ×400); (b) An area with marked cellular atypia (H and E, ×200). (c) Vascular invasion within the capsule, with fibrin thrombus formation associated with neoplastic follicular cells (arrow) (H and E, ×400). (d) ERG transcription factor immunohistochemistry, highlighting the endothelial cells (double arrows) lining the vascular space with neoplastic follicular cells within the lumen (×400). (e) Neoplastic cells negative for mucin (Mucicarmine, ×400). (f) Neoplastic cells positive for thyroglobulin (Thyroglobulin, ×200)
Clinical follow-up with nuclear scans revealed no definitive evidence of local or distant metastasis, and the patient received 30 mCi of I-131. At 6-month postthyroidectomy, the patient had no evidence of recurrence.
ADDITIONAL QUIZ QUESTIONS
Q1. Which of the following statements regarding prognosis when signet ring cell morphology is seen in a thyroid neoplasm has been reported in the literature?
-
Signet ring cell morphology in thyroid neoplasms is associated with a poor prognosis, much like carcinomas of the gastrointestinal tract showing similar morphology
-
Signet ring cell morphology indicates a metastatic tumor and is associated with a poor prognosis
-
Signet ring cell morphology in thyroid neoplasms does not appear to be associated with a poor prognosis, unlike carcinoma of the gastrointestinal tract showing similar morphology
-
Signet ring cell morphology in thyroid neoplasms has not been reported to be associatedS with prognosis.
Q2. Which of the following results on the immunohistochemical analysis of a cell block from a fine-needle aspiration of a thyroid nodule showing signet ring cell morphology is most consistent with a primary thyroid neoplasm?
-
Lesional cells positive for CAIX and CD10; negative for TTF-1 and thyroglobulin
-
Lesional cells positive for TTF-1 and napsin A; negative for CAIX and CD10
-
Lesional cells positive for ER and GATA3; negative for SOX10 and S100
-
Lesional cells positive for TTF-1 and thyroglobulin; negative for CAIX and CD10.
Q3. Which of the following statements is best, given the finding of signet ring cell morphology in an aspirate smear of a thyroid nodule?
-
A metastatic tumor to the thyroid is a possibility, but a thyroid primary should be ruled out
-
Signet ring cell morphology is not seen in primary thyroid neoplasms, so it is likely a metastasis
-
Signet ring cells indicate a malignant neoplasm, as this morphology is not associated with benign processes of the thyroid
-
A benign thyroid process is likely, and further workup is not necessary.
ANSWERS TO ADDITIONAL QUIZ QUESTIONS
Q1: C; Q2: D; Q3: A
BRIEF REVIEW OF THE TOPIC
“Signet-ring” is a commonly used descriptor for cells showing crescent-shaped nuclei compressed to the periphery of the cell secondary to cytoplasmic accumulation of vacuoles, inclusions, and various substances including mucin and lipids.[1] The finding of signet ring cells on a fine-needle aspiration (FNA) smear of a thyroid nodule can present a diagnostic challenge for the cytopathologist due to its rarity, broad differential diagnosis, and the potential for misdiagnosis as a metastatic lesion. Although the finding of signet ring cells in a neoplasm is often associated with gastrointestinal, breast, and lung carcinomas, there are limited reports in the literature of primary thyroid follicular adenomas and carcinomas with signet ring cells.[134567891011] Furthermore, the literature is even sparser with regard to the cytomorphology of these signet ring cell follicular neoplasms on FNA smears.[157891011]
Although metastasis to the thyroid is a rare event, it must be considered and ruled out when signet ring cells are encountered on an aspirate smear. The common primary sites of metastatic carcinomas to the thyroid reported in the literature include kidney, lung, and breast, among others.[112] In addition, signet ring cells can be seen in melanoma, along with carcinomas of varying sites.[12] Even cases of oncocytic thyroid neoplasms and adenomatous hyperplasia with signet ring cells have been exceptionally seen.[313] Combined evaluation of cytomorphology and appropriate use of IHC with an adequate cell block preparation are ideal in these situations to clarify the nature of the lesion. Immunohistochemical stains to consider using to differentiate primary from metastatic lesions would include thyroglobulin and TTF-1 (thyroid), CAIX and PAX8 (clear cell renal cell carcinoma), GATA3, mammaglobin and ER (breast), and Melan-A, HMB45, and SOX10 (melanoma). Caution should be employed when considering the use of PAX8 and TTF-1, as positive staining can be seen in primary thyroid lesions as well as metastatic renal cell carcinoma (PAX8+) and metastatic adenocarcinoma of the lung (TTF-1+).
The vacuoles imparting the signet ring cell morphology in follicular thyroid neoplasms are thought to be intracytoplasmic follicular lumina lined by microvilli based on ultrastructural studies, which may be due to an arrest in folliculogenesis.[3413] Accumulation of thyroglobulin and less frequently mucin has been shown within these vacuoles.[18] The clear cell variant of follicular neoplasms, in comparison to the signet ring cell variant, shows centrally located nuclei with cytoplasmic clearing due to the accumulation of similar material.[5] Medullary thyroid carcinoma is also considered in the differential due to the fine cytoplasmic vacuoles, which can be seen in various neuroendocrine neoplasms.[1415] It can be ruled out by immunohistochemical staining or measuring serum calcitonin levels. Although the finding of signet ring cells has been classically associated with a poor prognosis in malignancies from other sites, and especially in gastrointestinal tumors, this has not been the case in thyroid follicular neoplasms, as signet ring morphology has been identified more often in benign rather than malignant tumors.[16]
The general molecular genetics of thyroid neoplasms have been well studied. While BRAF and RET/PTC alterations are most commonly found in classic papillary thyroid carcinomas, genetic alterations, when found in follicular adenomas and carcinomas, typically involve RAS or PAX8/PPARγ.[1617] The molecular characterization of follicular neoplasms with signet ring cells, however, is lacking in the literature. This is probably due to the scarcity of cases reported and also due to the fact that many of them were reported decades ago. Two reported cases of follicular adenoma with signet ring cells were found negative for BRAF V600E mutations, but analysis for PAX8/PPARγ was not performed due to technical limitations.[11] Another series showed a PTEN variant through amplified multiplex PCR analysis of follicular adenoma with signet ring cells.[18]
CONCLUSION
The finding of signet ring cells in a thyroid aspirate presents a diagnostic challenge to the cytopathologist, with a variety of not only primary and metastatic neoplasms but also nonneoplastic conditions to consider. Although neoplasms showing signet ring cells typically are associated with a poor prognosis, this cytologic feature has been reported more often in benign rather than malignant thyroid processes.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
All authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author.
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article. CEF performed the literature review, organized the data, selected images, and drafted the manuscript. LS provided histological analysis and critically reviewed the manuscript. RN provided cytological analysis and critically reviewed the manuscript. FN provided clinical analysis and critically reviewed the manuscript. MJ conceived the study, participated in the design, performed cytological and histological analysis, selected final images, critically reviewed the manuscript draft, and is the corresponding author. All authors read and approved the final manuscript.
ETHICS STATEMENT BY ALL AUTHORS
As this is a case report without identifiers, our institution does not require approval from the Institutional Review Board (IRB)
LIST OF ABBREVIATIONS (In alphabetic order)
FNA - Fine-needle aspiration
IHC - Immunohistochemistry.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (the authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Follicular thyroid carcinoma with signet ring cell morphology: Fine-needle aspiration cytology, histopathology, and immunohistochemistry. Endocr Pathol. 2013;24:239-45.
- [Google Scholar]
- Cytology diagnosis of metastatic clear cell renal cell carcinoma, synchronous to pancreas, and metachronous to thyroid and contralateral adrenal: Report of a case and literature review. Diagn Cytopathol. 2017;45:161-7.
- [Google Scholar]
- Clear cell change in primary thyroid tumors. A study of 38 cases. Am J Surg Pathol. 1985;9:705-22.
- [Google Scholar]
- Signet-ring-cell thyroid tumors. Follicle cell tumors with arrest of folliculogenesis. Am J Surg Pathol. 1985;9:619-29.
- [Google Scholar]
- Cytopathology of follicular tumours of the thyroid with clear cell change. Cytopathology. 1991;2:125-35.
- [Google Scholar]
- Axillary node metastasis from differentiated thyroid carcinoma with hürthle and signet ring cell differentiation. A case of disseminated thyroid cancer with peculiar histologic findings. BMC Cancer. 2012;12:55.
- [Google Scholar]
- Signet-ring follicular adenoma of the thyroid diagnosed by fine needle aspiration. Report of a case with cytologic description. Acta Cytol. 2004;48:87-90.
- [Google Scholar]
- Fine-needle aspiration of mucin-producing thyroid tumors. Acta Cytol. 2011;55:549-55.
- [Google Scholar]
- Mucinous carcinoma of thyroid gland. Report of a primary and a metastatic mucinous tumour from ovarian adenocarcinoma with immunohistochemical study and review of literature. Virchows Arch. 2007;451:847-51.
- [Google Scholar]
- Signet-ring cell differentiation in FNA cytology of a primitive thyroid carcinoma. Cytopathology. 2013;24:274-5.
- [Google Scholar]
- The unique liquid-based cytologic findings of thyroid signet-ring follicular adenoma: A report of two cases with fine needle aspiration cytology. Acta Cytol. 2013;57:100-6.
- [Google Scholar]
- Metastatic signet ring cell carcinoma presenting as a thyroid nodule: Report of a case with fine-needle aspiration cytology. Diagn Cytopathol. 2010;38:597-602.
- [Google Scholar]
- Signet ring cells in a poorly differentiated hurthle cell carcinoma of the thyroid combined with two papillary microcarcinomas. Int J Surg Pathol. 2007;15:388-90.
- [Google Scholar]
- Cytoplasmic vacuolization: An under-recognized cytomorphologic feature in endocrine tumors of the pancreas. Diagn Cytopathol. 2013;41:623-8.
- [Google Scholar]
- Cytologic diagnosis of medullary carcinoma of the thyroid gland. Diagn Cytopathol. 2000;22:351-8.
- [Google Scholar]
- Molecular genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol. 2011;7:569-80.
- [Google Scholar]
- Primary benign and malignant thyroid neoplasms with signet ring cells: Cytologic, histologic, and molecular features. Am J Clin Pathol. 2017;148:251-8.
- [Google Scholar]







