Translate this page into:
Diagnostic agreement between bronchoalveolar lavage and transbronchial lung biopsy in patients with suspected pulmonary diseases: A single-center study
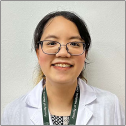
*Corresponding author: Sayanan Chowsilpa, Department of Pathology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand. sayanan.c@cmu.ac.th
-
Received: ,
Accepted: ,
How to cite this article: Wannasai K, Kongkarnka S, Lertprasertsuke N, Phinyo P, Namwong C, Yaowarat T, et al. Diagnostic agreement between bronchoalveolar lavage and transbronchial lung biopsy in patients with suspected pulmonary diseases: A single-center study. CytoJournal. 2025;22:43. doi: 10.25259/Cytojournal_205_2024
Abstract
Objective
This study investigates the diagnostic concordance between bronchoalveolar lavage (BAL) cytology and the histologic analysis of transbronchial lung biopsy (TBLB) specimens in patients with suspected pulmonary diseases to highlight the strengths and limitations of these complementary diagnostic tools.
Material and Methods
We conducted a comprehensive retrospective cross-sectional analysis on patients suspected of pulmonary diseases who underwent both BAL and TBLB from 2018 to 2022. We assessed diagnostic agreement using kappa statistics and calculated the overall concordance rates. The analysis was stratified based on malignant versus infectious etiologies to elucidate performance differences between the two methods.
Results
Our study included a cohort of 189 patients, comprising 104 individuals with suspected malignancy and 85 with suspected infections. Among the malignancy group, BAL yielded positive results for cancer in 49 patients, whereas TBLB confirmed malignancy in 64 patients, demonstrating an overall agreement of 70.19% (kappa = 0.52, 95% confidence interval [CI]: 0.38–0.66). Conversely, within the infectious cohort, BAL identified micro-organisms in only five patients, while TBLB diagnosed infection in 22 patients, achieving an overall agreement of 77.65% (kappa = 0.29, 95% CI: 0.17–0.41).
Conclusion
Our findings underscore the critical role of BAL cytology in the diagnosis of pulmonary carcinoma and infectious processes while also revealing its limitations in detecting interstitial lung diseases. The TBLB procedure emerges as an indispensable technique for accurate histopathological evaluation in lung cancer diagnostics. The integration of BAL and TBLB not only enhances diagnostic yield but also provides a more comprehensive understanding of pulmonary pathologies. Notably, we found moderate agreement between BAL and TBLB in neoplastic cases and fair agreement in non-neoplastic conditions, suggesting a nuanced interplay between these methodologies that could inform clinical practice and improve patient outcomes. This study advocates a combined approach in diagnostic frameworks to optimize the management of patients with suspected pulmonary diseases, paving the way for more precise and effective diagnoses in the field of cytology.
Keywords
Biopsy
Bronchoalveolar lavage
Cytology
Histopathology
Pulmonary diseases
INTRODUCTION
Respiratory diseases represent a notable global health challenge, significantly contributing to morbidity and mortality rates worldwide. Traditional histopathology is considered the gold standard for diagnosing these conditions. However, cytology, specifically involving techniques such as bronchoalveolar lavage (BAL), brush cytology, and fine needle aspiration (FNA), serves as a valuable complementary diagnostic tool. Current diagnostic practices often involve obtaining patient specimens to enable accurate pathological examination, with concurrent BAL frequently performed alongside transbronchial lung biopsy (TBLB) to enhance diagnostic accuracy.[1-4]
Evidence suggests that combining BAL with TBLB improves diagnostic precision, particularly for infiltrative peripheral lung cancers and metastatic lesions. For instance, a study by Tang et al. reported a diagnostic accuracy of 73% for infiltrative cancers when combining these techniques, rising to 100% for metastatic lung cancer.[5] This highlights the advantages of using a dual approach to enhance diagnostic outcomes for suspected malignancies. However, limitations exist concerning non-neoplastic lesions, where the agreement between cytological findings from BAL and TBLB is often minimal. Jois et al. indicated that such limitations could potentially be addressed through the application of cytology in conjunction with lung biopsies.[2]
While BAL is advantageous due to its minimal complication risk compared to lung biopsies, its reliability in diagnosing specific lung disorders, such as interstitial lung disease, is inconsistent and varies when compared to TBLB outcomes.[6-9] The results of previous studies have shown that the agreement between BAL and TBLB remains notably high in cancer detection. However, there is a pressing need to better understand how these techniques can be optimized for broader lung disease pathologies. Nevertheless, under socioeconomic limitations, BAL is a quick and useful diagnostic procedure for ruling out malignancy.[8,10] Sareen and Pandey suggested using the BAL cytology for malignancy screening before administering treatment for tuberculosis under the high prevalence of tuberculous infection region.[8] Chang et al. even suggested that BAL could diagnose interstitial lung disease in patients with suspicious radiography and should be done early in admitted patients with malignancy, connective tissue diseases, or transplantation who had poor response to initial medications for additional treatment.[11] These studies supported the usefulness, quickness, and cost-effectiveness of BAL diagnoses in the treatment of pulmonary diseases.
This investigation aims to assess the diagnostic agreement between BAL and TBLB in patients with suspected malignant and infectious pulmonary diseases within a single-center setting. By elucidating the relationship between these diagnostic modalities, this study aims to identify whether combining BAL with TBLB can enhance detection rates and provide a more accurate framework for diagnosing complex pulmonary conditions. Resolving this dilemma will contribute valuable insights into clinical practices and potentially improve patient management strategies in respiratory medicine.
MATERIAL AND METHODS
Study design
This study involved a retrospective cross-sectional review of bronchoscopic procedures conducted between 2018 and 2022. The study protocol was approved by the Research Ethics Committee Panel 5, Faculty of Medicine, Chiang Mai University, and all ethical principles were adhered to according to the Helsinki Declaration.[12]
Study population
The study included all patients exhibiting clinical and radiologic features indicative of lung diseases, encompassing neoplasms, interstitial lung diseases, and infections. Eligible participants were those who underwent both BAL and TBLB during the defined study period. The exclusion criteria were patients with only BAL or only TBLB, which could not be calculated using the cytology and histology correlation.
Procedures
Both BAL and TBLB procedures were performed by qualified pulmonologists in the Pulmonology Unit. Before the procedure, informed consent for investigation and treatment was obtained from all patients. Procedures followed the standard protocols for asepsis, premedication, sedation, and anesthesia. A transnasal standard flexible fiberoptic bronchoscope (Olympus, BF-1T150 Adult, Tokyo, Japan) was utilized for the procedures.
Topical lidocaine was administered before the bronchoscopy. The bronchoscope was then advanced to obtain cytologic and histologic specimens, carefully adhering to aseptic techniques. BAL samples were collected through the instillation of sterile saline and subsequently sent to the Pathology Laboratory for processing. The BAL samples were preserved and analyzed through liquid-based cytology, stained using the Papanicolaou method according to manufacturer recommendation (YD Diagnostics CORP, Gyeonggi-do, Republic of Korea), and thoroughly examined by experienced pulmonary pathologists and cytopathologists. The identification of malignant cells was confirmed by observing distinctive malignant features within the BAL samples, while additional findings, such as micro-organisms or other abnormal cells, were documented.
For TBLB, tissue biopsies were collected from the bronchial trees by carefully inserting biopsy forceps (Erbe Cryoprobe, flexible, diameter 1.9 mm, length 900 mm, Germany) through the bronchoscope. This technique enabled the strategic positioning of the bronchoscope in the segmental bronchi, allowing for the procurement of several biopsies, with a target of obtaining three to eight specimens.
Tissue samples were preserved in a 10% buffered formalin solution and subsequently embedded in paraffin. A trained technician utilized a microtome (Leica, RM2235, Leica Biosystems, Germany) to create five-micron sections, which were then stained with hematoxylin-eosin (H&E) according to the manufacturer’s recommendation (Merck KGaA, Darmstadt, Germany) before evaluation by pulmonary pathologists. The definitive diagnosis of lung cancer was established through the identification of malignant cells within the histological samples, while the detection of micro-organisms was based on their presence observed through H&E staining or special stains, including acid-fast staining (BenchMark Special Stains – acid-fast bacilli [AFB] III procedure, Roche Diagnostics, Mannheim, Germany) and Gomori-methenamine silver (GMS) staining (GMS II Staining Kit, Roche Diagnostics, Mannheim, Germany) according to the manufacturer’s recommendation.
Data collection
Pathology reports and demographic data were extracted from the hospital’s secure electronic record system.
Statistical analysis
Descriptive statistics were employed to summarize the categorical data, reported as frequency and percentage. The analysis focused on assessing the diagnostic concordance between cytological and histopathological findings in patients with pulmonary diseases. Overall agreement and kappa statistics were calculated to evaluate the level of agreement. In addition, the sensitivity and diagnostic accuracy of BAL cytological findings for pulmonary diseases were evaluated. A case was classified as a true positive when both cytological and histopathological examinations indicated malignancy. A true negative was a case showing negative for malignancy on both cytological and histopathological assessments. Conversely, a false positive referred to a case where cytology suggested malignancy, but histopathology did not confirm this. A case with negative cytology but positive histopathology for malignancy was regarded as a false negative. Statistical analyses were conducted using Stata 16 (StataCorp, College Station, TX, USA). Confidence intervals were reported for the relevant statistical measures, and all P-values were deemed significant at <0.05.
RESULTS
Demographic data
A total of 189 patients underwent BAL and TBLB for pulmonary diseases through clinical and radiological assessments. The average age was 61.97 years, ranging from 17 to 89. The group consisted of 110 males (58.2%) and 79 females (41.8%). Upon completion, the patients were categorized into individuals with pulmonary neoplasms and those with other non-neoplastic conditions.
Agreement of pulmonary neoplastic diseases
Within the cohort of 104 patients suspected of having pulmonary neoplastic diseases, 56 (53.84%) were male and 48 (46.15%) female, with a mean age of 65.11 years, ranging from 39 to 87. The BAL analysis yielded positive results in 49 patients, including 34 adenocarcinomas, one squamous cell carcinoma, two non-small cell carcinomas without a specific cell type, and 12 cases that showed the presence of atypical cells (tumor type could not be specified). The TBLB led to the final diagnosis of lung cancer in 64 cases comprising 54 adenocarcinomas, six squamous cell carcinomas, three metastatic cancers (metastatic osteosarcoma, metastatic colonic adenocarcinoma, and metastatic nasopharyngeal squamous cell carcinoma), and one Kaposi sarcoma as indicated in Table 1 and Figure 1 evidencing malignancy in both BAL and TBLB. Figures 1a and b reveal pulmonary adenocarcinoma, and Figures 1c and d reveal pulmonary squamous cell carcinoma.
| Neoplastic pulmonary diseases | ||
| Diagnosis | BAL n, (%) | TBLB n, (%) |
| Negative for malignancy | 55 (52.88%) | 40 (38.46%) |
| Adenocarcinoma | 34 (32.69%) | 54 (51.92%) |
| Squamous cell carcinoma | 1 (0.96%) | 6 (5.77%) |
| Atypical cells | 12 (11.54%) | Metastatic tumor 3 (2.88%) |
| Positive for NSCLC | 2 (1.92%) | Kaposi sarcoma 1 (0.96%) |
| Total | 104 (100.00%) | 104 (100.00%) |
| Non-neoplastic pulmonary diseases | ||
| Diagnosis | BAL n, (%) | TBLB n, (%) |
| Negative for malignancy or micro-organism | 79 (92.94%) | 62 (72.94%) |
| Positive for fungus | 4 (4.71%) | 9 (10.59%) |
| Positive for eosinophils | 1 (1.18%) | Chronic eosinophilic pneumonia 1 (1.18%) |
| Positive for CMV-infected cells | 1 (1.18%) | CMV pneumonitis 1 (1.18%) |
| - | Granuloma 12 (14.12%) | |
| Total | 85 (100.00%) | 85 (100.00%) |
BAL: Bronchoalveolar lavage, TBLB: Transbronchial lung biopsy, CMV: Cytomegalovirus, NSCLC: Non-small cell lung cancer
![Malignancy. (a and b) Positive for adenocarcinoma. (a) The bronchoalveolar lavage (BAL) revealed clusters of malignant cells with vacuolated cytoplasm (Liquid-based preparation, Papanicolaou stain, ×40 objective) Scale bar, 50 µm. (b) The transbronchial lung biopsy (TBLB) from the same case revealed tissue fragments of malignant cells with glandular formations (Hematoxylin-Eosin [H&E] stain, ×10 objective). Scale bar, 200 μm. (c and d) Positive for squamous cell carcinoma. (c) BAL revealed a group of malignant cells with coarse chromatin and a moderate amount of dense cytoplasm (Liquid-based preparation, Papanicolaou stain, ×40 objective). Scale bar, 50 μm. (d) TBLB in the same case revealed tissue fragments of malignant squamous epithelium among desmoplastic stroma (H&E stain, ×10 objective). Scale bar, 200 µm.](/content/105/2025/22/1/img/Cytojournal-22-43-g001.png)
- Malignancy. (a and b) Positive for adenocarcinoma. (a) The bronchoalveolar lavage (BAL) revealed clusters of malignant cells with vacuolated cytoplasm (Liquid-based preparation, Papanicolaou stain, ×40 objective) Scale bar, 50 µm. (b) The transbronchial lung biopsy (TBLB) from the same case revealed tissue fragments of malignant cells with glandular formations (Hematoxylin-Eosin [H&E] stain, ×10 objective). Scale bar, 200 μm. (c and d) Positive for squamous cell carcinoma. (c) BAL revealed a group of malignant cells with coarse chromatin and a moderate amount of dense cytoplasm (Liquid-based preparation, Papanicolaou stain, ×40 objective). Scale bar, 50 μm. (d) TBLB in the same case revealed tissue fragments of malignant squamous epithelium among desmoplastic stroma (H&E stain, ×10 objective). Scale bar, 200 µm.
Out of 104 patients suspected of having pulmonary neoplastic diseases, 55 were determined to be cytologically negative for malignancy by BAL, with 40 accurately identified as histologically negative for malignancy through TBLB. The overall agreement between BAL cytology and TBLB histopathological diagnosis was 70.19% with a 95% confidence interval (95% confidence interval [CI]) of 60.43– 78.76 and kappa’s statistics of 0.52 (95% CI: 0.38–0.66), indicating moderate agreement. The diagnostic accuracy of the BAL cytological examination was 79.81%. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of BAL cytology are presented in Tables 2 and 3.
| Bronchoalveolar lavage | Transbronchial lung biopsy | |||||||
|---|---|---|---|---|---|---|---|---|
| Negative for malignancy | Adeno carcinoma | Squamous cell carcinoma | Metastatic tumor | Kaposi sarcoma | Total | Overall agreement (95% CI) | Kappa (95% CI ) | |
| Negative for malignancy | 37 | 11 | 4 | 2 | 1 | 55 | 70.19% (60.43–78.76) | 0.52 (0.38–0.66) |
| Adenocarcinoma | 0 | 34 | 0 | 0 | 0 | 34 | ||
| Squamous cell carcinoma | 0 | 0 | 1 | 0 | 0 | 1 | ||
| Atypical cells | 3 | 7 | 1 | 1 | 0 | 12 | ||
| Positive for NSCLC | 0 | 2 | 0 | 0 | 0 | 2 | ||
| Total | 40 | 54 | 6 | 3 | 1 | 104 | ||
BAL: Bronchoalveolar lavage, TBLB: Transbronchial lung biopsy, NSCLC: Non-small cell lung cancer, CI: Confidence interval
| Parameter | Finding |
|---|---|
| Sensitivity | 93.90% (95% CI: 83.10–98.70) |
| Specificity | 67.30% (95% CI: 53.30–79.30) |
| ROC area | 0.82 (95% CI: 0.73–0.88) |
| Positive predictive value | 71.90% (95% CI: 59.20–82.40) |
| Negative predictive value | 92.50% (95% CI: 79.60–98.40) |
| Diagnostic accuracy | 79.81% |
CI: Confidence interval, ROC: Receiver operating characteristics, BAL: Bronchoalveolar lavage
Agreement on pulmonary non-neoplastic diseases
In another subset of 85 patients suspected of having nonneoplastic pulmonary diseases, 54 (63.52%) were males and 31 (36.47%) females, with a mean age of 58.14 years ranging from 17 to 89. The BAL revealed evidence of pulmonary infection in five cases (four for fungal infection and one for cytomegalovirus infection) and one case of eosinophil-rich fluid. TBLB contributed to the final diagnosis of pulmonary infection in 22 cases, including nine cases of fungal infection, one case of cytomegalovirus infection, and 12 cases of caseating granulomatous inflammation. In addition, one case was diagnosed with chronic eosinophilic pneumonia by TBLB. Table 1 and Figure 2 show details of infections in both BAL and TBLB. Figure 2a-c reveals yeasts in macrophages. Figure 2d-f reveals inflammatory cells in both Papanicolaou and H&E stains, while the acid-fast stain reveals AFB positive.
![Infection (a-c) Histoplasmosis. (a) The bronchoalveolar lavage (BAL) revealed a macrophage containing round-shaped microorganisms (Liquid-based preparation, Papanicolaou stain, ×40 objective). (b) The transbronchial lung biopsy (TBLB) from the same case revealed granulomas (Hematoxylin-Eosin [H&E] stain, ×40 objective). (c) GMS stain revealed small narrow-based budding yeasts in macrophages (GMS stain, ×40 objective). (d, e, and f) Tuberculosis. (d) The BAL revealed inflammatory cells among fibrinous backgrounds (Liquid-based preparation, Papanicolaou stain, ×40 objective). (e) TBLB from the same case revealed numerous macrophages and epithelioid histiocytes (H&E stain, ×40 objective). (f) Numerous acid–fast bacilli (Acid–fast bacilli stain, ×40 objective). Scale bar, 50 µm.](/content/105/2025/22/1/img/Cytojournal-22-43-g002.png)
- Infection (a-c) Histoplasmosis. (a) The bronchoalveolar lavage (BAL) revealed a macrophage containing round-shaped microorganisms (Liquid-based preparation, Papanicolaou stain, ×40 objective). (b) The transbronchial lung biopsy (TBLB) from the same case revealed granulomas (Hematoxylin-Eosin [H&E] stain, ×40 objective). (c) GMS stain revealed small narrow-based budding yeasts in macrophages (GMS stain, ×40 objective). (d, e, and f) Tuberculosis. (d) The BAL revealed inflammatory cells among fibrinous backgrounds (Liquid-based preparation, Papanicolaou stain, ×40 objective). (e) TBLB from the same case revealed numerous macrophages and epithelioid histiocytes (H&E stain, ×40 objective). (f) Numerous acid–fast bacilli (Acid–fast bacilli stain, ×40 objective). Scale bar, 50 µm.
On the other hand, in 79 out of 85 cases, no evidence of infection or malignancy was diagnosed by BAL, while 62 out of 85 cases showed no evidence of infection or malignancy through histological examination. The agreement between BAL cytology and TBLB histopathology in negative results reached 77.65% (95% CI: 67.31–85.97), with a kappa coefficient of 0.29 (95% CI: 0.17–0.41), indicating fair agreement, as illustrated in Table 4.
| Bronchoalveolar lavage | Transbronchial lung biopsy | |||||||
|---|---|---|---|---|---|---|---|---|
| Negative for malignancy | Positive for fungus | Pulmonary eosinophilia | Positive for CMV | Granuloma | Total | Overall agreement (95% CI) | Kappa (95% CI ) | |
| Negative for malignancy or micro-organism | 61 | 6 | 0 | 0 | 12 | 79 | 77.65% (67.31–85.97) | 0.29 (0.17–0.41) |
| Positive for fungus | 1 | 3 | 0 | 0 | 0 | 4 | ||
| Positive for eosinophils | 0 | 0 | 1 | 0 | 0 | 1 | ||
| Positive for CMV | 0 | 0 | 0 | 1 | 0 | 1 | ||
| Total | 62 | 9 | 1 | 1 | 12 | 85 | ||
BAL: Bronchoalveolar lavage, TBLB: Transbronchial lung biopsy, CMV: Cytomegalovirus, CI: Confidence interval
DISCUSSION
The incidence of pulmonary lesions has steadily increased in recent years. Clinicians and pathologists have many patients with pulmonary lesions. Patients prefer straightforward and economical examinations that result in shorter hospital stays. Preliminary screening may involve bronchial cytology (brush and wash). Pathologists and clinicians must engage in interactions and cooperation to facilitate additional treatment in pulmonary cytopathology fields.[13] This study aims to evaluate the diagnostic agreement between BAL cytology and TBLB histopathologic analysis in patients with suspected pulmonary conditions. The results demonstrate a substantial level of agreement (70.19%) with a kappa statistic of 0.52 for neoplastic diseases. These findings indicate that combining BAL and TBLB can effectively diagnose lung malignancies and support their use as complementary diagnostic tools in clinical practice.
Several factors contribute to the agreement between BAL cytology and TBLB histology for pulmonary neoplastic diseases. Dionísio reveals that the sensitivity of TBLB for diagnosing peripheral pulmonary neoplastic lesions fluctuates based on the number of biopsy samples extracted and the size of the lesion.[14] Moreover, the distribution of the lesion, whether focal or diffuse, combined with the small size of the acquired samples, the potential for confounding factors arising from crush artifacts, and the challenge of penetrating beyond the peribronchial sheath are all significant considerations.[15]
In comparing our findings with previous studies, it is noteworthy that the sensitivity and PPV of BAL in our cohort were higher than those reported by Salama et al., who found a sensitivity of only 40.3% and a specificity of 51.7%.[16] While our study shows improved sensitivity and PPV, it also reflects lower specificity and NPV. Moreover, a study by Ahmed and Ahmed reported higher sensitivity of BAL cytology (93.44%), specificity (100%), and NPV (75%), with 94.5% diagnostic efficacy compared with transbronchial needle aspiration.[10]
This highlights the diverse nature of existing research and suggests a need for careful interpretation of diagnostic metrics in different clinical contexts.
The moderate agreement (77.65%) observed for nonneoplastic diseases, with a kappa statistic of 0.29, underscores the complexities involved in diagnosing pulmonary conditions that are not malignancies. While this suggests some consistency between BAL and TBLB, the relatively low kappa value indicates fair to poor agreement, suggesting that these methods should be interpreted cautiously in nonneoplastic scenarios. Factors influencing low agreement levels could include the distribution, size, and complexity of the non-neoplastic pulmonary diseases evaluated, as well as the inherent limitations of both diagnostic techniques.
Various factors, such as the distribution of lesions, the size and type of non-neoplastic pulmonary diseases being assessed, and the specific methodologies used in BAL and TBLB, may influence the level of agreement observed. Jois’s study examined the correlation between TBLB and lung cytology in respiratory specimens. The highest level of concordance for malignancy was observed with imprint cytology, achieving a rate of 77.78%, followed by BAL at 40.91% and brush cytology at 40.00%. Overall, the degree of agreement between cytological evaluations and biopsy results was significantly low for non-neoplastic lesions. Notably, when BAL and imprint smears were utilized in tandem, the concordance rate improved to 42.50% compared to other methodological combinations. The authors advocate the application of a multimodal approach incorporating various cytological techniques in cases where malignancy is suspected, as this strategy is more efficacious than relying on a single diagnostic modality. They recommend the systematic inclusion of imprint smears across all cases; however, it remains clear that biopsy continues to be the gold standard for the diagnosis of non-neoplastic lung diseases.[2] In addition, studies from Davidson et al. and Tomassetti et al. concluded that BAL with cellular analysis was found to be a useful diagnostic adjunct in interstitial lung diseases.[1,4]
The moderate agreement between BAL cytology and TBLB histopathology has important implications for clinical decision-making. While BAL demonstrates a high diagnostic accuracy, its limitations in sensitivity suggest that it should not be solely relied upon for malignancy detection, especially in patients with high suspicion. This necessitates a multifaceted diagnostic approach, incorporating both BAL and TBLB for enhanced diagnostic precision. In addition, understanding the potential for false negatives in BAL emphasizes the importance of histological confirmation through TBLB as the gold standard.
One of the primary strengths of our study lies in its design, involving a comprehensive retrospective analysis of bronchoscopic procedures conducted at a single institution. The rigorous methodology adopted, including well-defined inclusion criteria and thorough data collection, contributes to the reliability of our findings. In addition, the technical proficiency of the pulmonologists performing the procedures likely enhances the accuracy of the results, thereby improving the interpretation of diagnostic outcomes.
Despite these strengths, certain limitations must be acknowledged. The specificity of BAL for neoplastic diseases was found to be relatively low (67.3%), potentially influenced by factors such as the location of peripheral tumors, which might yield fewer detectable malignant cells, and the presence of degenerative cells that could confound results. Such limitations are consistent with existing literature, highlighting the variability in diagnostic performance due to sampling techniques, the experience of the bronchoscopist, and the distribution and histological characteristics of the lesions involved.[10,14,16] In addition, the higher adverse event rate noted in this study may reflect the severity of the pulmonary conditions in the patient cohort under investigation. While our agreement percentage of 70.19% indicates moderate concordance, it is critical to acknowledge that kappa statistics also account for chance agreements, which can obfuscate true diagnostic reliability. Moreover, the single-center design may restrict the generalizability of the results, as data derived from one institution may not accurately represent the diversity of patient demographics, disease prevalence, or treatment practices observed in multicenter studies. The sample size of 189 patients, although adequate for initial analyses, may limit the robustness of conclusions, particularly concerning specific pulmonary disease subgroups, as a larger and more diverse cohort would yield a more accurate representation of diagnostic outcomes.
Future research should address these limitations through multicenter trials with larger sample sizes and standardized methodologies while also exploring the potential impact of technological advancements in cytology and histopathology, such as the implementation of artificial intelligence in image analysis and enhanced imaging techniques, which could improve diagnostic accuracy and agreement between BAL and TBLB. Integrating these innovations may lead to more reliable diagnoses and improved patient outcomes.
SUMMARY
This research highlights the value of BAL cytology in diagnosing pulmonary carcinoma and pulmonary infections. In the context of diagnosing lung cancer, a TBLB procedure is essential for accurate tissue examination. Despite BAL’s potentially low yield, its inclusion in the procedure can be beneficial, potentially saving time. Furthermore, the examination of BAL fluid may enable the diagnosis of pulmonary diseases in patients with inaccessible peripheral pulmonary lesions. Combining TBLB with BAL has the potential to further enhance the positive diagnostic rate.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
ABBREVIATIONS
AFB: Acid–fast bacilli
BAL: Bronchoalveolar lavage
FN: False negative
FNA: Fine needle aspiration
FP: False positive
GMS: Gomori-methenamine silver
H&E: Hematoxylin-eosin
NPV: Negative predictive value
PPV: Positive predictive value
TBLB: Transbronchial lung biopsy
TBNA: Transbronchial needle aspiration
TN: True negative
TP: True positive
AUTHOR CONTRIBUTIONS
KW: Concept, design, literature search, clinical studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, manuscript review, and funding; SK and NL: Clinical studies and data acquisition; PP: design, data analysis, and statistical analysis; CN, TY, PS, PV, and SC: Literature search, data acquisition, data analysis; WD: Literature search, clinical studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review; SCH: Concept, design, literature search, clinical studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, and manuscript review. All authors have provided their final approval for the version intended for publication. Each has participated adequately in the work to assume public responsibility for relevant parts of the content and has agreed to be accountable for all aspects of the work, ensuring that any issues regarding its accuracy or integrity are addressed. All authors meet the authorship status of ICMJE.
ACKNOWLEDGMENT
Not applicable.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research was approved by the Research Ethics Committee Panel 5 of Faculty of Medicine, Chiang Mai University (STUDY CODE: PAT-2565-09319). The authors certify that they have obtained all appropriate patient consent.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
EDITORIAL/PEER REVIEW
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through an automatic online system.
FUNDING: This work was supported by the Faculty of Medicine, Chiang Mai University Endowment Fund [grant number 067/2566].
References
- Bronchoalveolar lavage as a diagnostic procedure: A review of known cellular and molecular findings in various lung diseases. J Thorac Dis. 2020;12:4991-5019.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation between transbronchial lung biopsy and lung cytology. Rev Esp Patol. 2020;53:75-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnoses from lung specimen collected through flexible bronchoscopy from patients in a tertiary hospital in dar es Salaam Tanzania: A retrospective cross-sectional study. BMC Pulm Med. 2019;19:214.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchoalveolar lavage and lung biopsy in connective tissue diseases, to do or not to do? Ther Adv Musculoskelet Dis. 2021;13:1759720x211059605.
- [CrossRef] [PubMed] [Google Scholar]
- Value of bronchoalveolar lavage combined with transbronchial lung biopsy in the diagnosis of peripheral lung cancer. Chang Gung Med J. 2000;23:695-700.
- [Google Scholar]
- Transbronchial biopsy vs. Bronchoalveolar lavage in interstitial lung disease. Curr Opin Pulm Med. 2022;28:3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Interstitial lung disease: The diagnostic role of bronchoscopy. J Thorac Dis. 2017;9:S996-1010.
- [CrossRef] [PubMed] [Google Scholar]
- Lung malignancy: Diagnostic accuracies of bronchoalveolar lavage, bronchial brushing, and fine needle aspiration cytology. Lung India. 2016;33:635-41.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchoalveolar lavage In: Ernst A, Herth FJ, eds. Principles and practice of interventional pulmonology. New York: Springer; 2013. p. :165-76.
- [CrossRef] [Google Scholar]
- Comparison of bronchoalveolar lavage cytology and transbronchial biopsy in the diagnosis of carcinoma of lung. J Ayub Med Coll Abbottabad. 2004;16:29-33.
- [Google Scholar]
- Clinical usefulness of bronchoalveolar lavage in patients with interstitial lung diseases: A pilot study. J Thorac Dis. 2020;12:3125-34.
- [CrossRef] [PubMed] [Google Scholar]
- The 2024 revision to the declaration of helsinki: Modern ethics for medical research. JAMA. 2025;333:30-1.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of bronchial cytological diagnosis in lung lesions in comparison with histopathology. J Cytol. 2022;39:163-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic flexible bronchoscopy and accessory techniques. Rev Port Pneumol. 2012;18:99-106.
- [CrossRef] [PubMed] [Google Scholar]
- The role of transbronchial biopsy in the diagnosis of diffuse parenchymal lung diseases: Con. Rev Port Pneumol. 2012;18:61-3.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchoalveolar lavage in lung cancer: Does it increase the positive yield of bronchoscopy? Egypt J Chest Dis Tuberc. 2023;72:326-33.
- [CrossRef] [Google Scholar]









