Translate this page into:
Diagnostic value of ultrasound-guided fine-needle aspiration cytology in the pathological natures of thyroid nodules: A retrospective study

*Corresponding author: Wenting Tan, Department of Ultrasound Medicine, The Fifth Affiliated Hospital of Southern Medical University, Guangzhou, Guangdong, China. 15112158715@163.com
-
Received: ,
Accepted: ,
How to cite this article: Xing G, Tan W. Diagnostic value of ultrasound-guided fine-needle aspiration cytology in the pathological natures of thyroid nodules: A retrospective study. CytoJournal. 2024;21:21. doi: 10.25259/Cytojournal_34_2024
Abstract
Objective:
Thyroid nodules, a clinical disease with high incidence, include benign and malignant types. This study aims to evaluate the diagnostic value of ultrasound-guided fine-needle aspiration cytology (US-FNAC) in determining the pathological nature of thyroid nodules and to conduct an in-depth analysis of its diagnostic efficacy across nodules of varying sizes.
Material and Methods:
This retrospective study identified 116 patients undergoing thyroidectomy in Zibo Central hospital from January 2022 to March 2023, with 98 meeting the study’s inclusion criteria. All patients received ultrasound and US-FNAC examinations before surgery to analyze the ultrasonic features of thyroid nodules. The diagnosis results of pathological natures obtained by US-FNAC were analyzed with the result of post-operative pathological examination as the gold standard. The patients were divided into four groups according to the median and quartile of nodular diameters to explore the diagnostic efficacy of US-FNAC for the pathological natures of thyroid nodules with various diameters and comprehensively evaluate its application value. The evaluation tool of diagnostic efficacy was the receiver operator characteristic (ROC) curve.
Results:
A total of 98 puncture nodules were evaluated, with a diameter of 0.8–5.2 cm. Post-operative pathological examination showed 10 (10.20%) benign and 88 (89.80%) malignant lesions. The ultrasound examination showed 14 (14.29%) benign and 84 (85.71%) suspected malignant lesions. The US-FNAC results showed 2 cases (2.04%) of type I, 9 cases (9.18%) of type II, 3 cases (3.06%) of type III, 29 cases (29.59%) of type IV, 39 cases (39.80%) of type V, and 16 cases (16.33%) of type VI, including 9 (9.18%) benign and 84 (85.72%) malignant lesions and 5 (5.10%) uncertain pathological natures. According to the median and quartile of nodular diameters, specifically, 1.90 (1.60, 2.30) cm, 93 nodules with decided pathological natures were divided into groups Q1 (n = 24, ≤1.6 cm), Q2 (n = 26, 1.7–1.9 cm), Q3 (n = 24, 2.0–2.3 cm), and Q4 (n = 19, >2.3 cm). The results of ROC analysis showed that the area under the curve (AUC), sensitivity, and specificity of US-FNAC diagnosis were 0.894, 98.80%, and 80.00%, respectively. The AUCs of US-FNAC in groups Q1, Q2, Q3, and Q4 were 0.978, 1.000, 0.977, and 0.971. The AUCs of Q1 group, Q2 group, Q3 group and Q4 group were all > 0.9, and US-FNAC had high diagnostic efficiency for the pathological properties of thyroid nodules with different diameters.
Conclusion:
US-FNAC has a high diagnostic efficiency for the pathological properties of thyroid nodules. Whether the nodule diameter has an effect on the accuracy of this method requires more clinical evidence.
Keywords
Ultrasound
Fine-needle aspiration cytology
Thyroid nodule
Pathological nature
INTRODUCTION
Thyroid nodules are a commonly observed condition in clinical practice with a complex etiology and can be classified as benign or malignant.[1] Related research results show that the incidence of malignant nodules in patients with thyroid nodules is approximately 5.6–79.8%.[2] Compared with patients with benign nodules, patients with malignant thyroid nodules have more serious conditions, and their physical and mental health and quality of life are affected,[3-6] so timely identification of the pathological natures of thyroid nodules is vital.
The puncture technique was first used in the pathological examination of tumors in 1930 and was adopted in the cutting biopsy of thyroid diseases in the 1950s and 1960s. However, traditional coarse needle biopsy can lead to complications or metastasis of tumor cells along the needle tract, limiting its clinical application.[7-9] Fine-needle aspiration biopsy (FNAB) is a newer technique that offers minimal injury, reduced pain, and ease of operation. FNAB effectively mitigates the complications and metastasis risks associated with coarse needle biopsy, thus reducing the need for unnecessary surgeries. Consequently, it has gradually become the biopsy technique recommended by clinical guidelines.[10-12] Hence, higher requirements are placed on the puncture path and site accuracy because of the limited tissue dose obtained by fine-needle aspiration.
With the continuous improvement of modern medical technology and ultrasound equipment, ultrasound technology has also been used in thyroid nodule examination, which shows an increasing trend in the detection rate of nodules.[13-15] Ultrasound-guided fine-needle aspiration cytology (USFNAC) is a minimally invasive technique that effectively diagnoses the nature of thyroid nodules. Unfortunately, clinical reports on the diagnostic value of US-FNAC in determining the nature of thyroid nodules are scarce, and the relationship between the diagnostic efficacy of US-FNAC and nodular diameter has not been established. In this study, the result of post-operative pathological examination was the gold standard for analyzing the value of US-FNAC in diagnosing benign and malignant thyroid nodules and exploring its application effect in nodules of different sizes. This study aims to provide an effective reference for improving the accuracy of clinical diagnosis of nodular natures, determining treatment options, and evaluating prognosis.
MATERIAL AND METHODS
Inclusion and exclusion criteria
Inclusion criteria
Adult patients with thyroid nodules diagnosed by ultrasound, those undergoing resection surgery of thyroid nodules for the first time, those with basic listening, speaking, reading, and writing abilities, and those with complete clinical data were included.
Exclusion criteria
Patients with infection or skin injury at the puncture site after US-FNAC, puncture failure, cognition or communication disorders, incomplete clinical data, treatments such as sclerosing agent injection, drugs, radiofrequency ablation before enrollment, the history of radiotherapy and tumor surgery, distant metastasis of malignant tumors, severe diseases in heart, liver and kidney or other tumor types, and those in lactation period or gestation period were excluded.
Study methods
This retrospective study was approved by the medical ethics committee of Zibo Central Hospital (approval no.: 2024052). Considering the anonymity of data, patients informed consent was waived. The study was conducted in accordance with the Declaration of Helsinki.
A total of 116 patients underwent thyroidectomy in Zibo Central Hospital from January 2022 to March 2023, whose eligibility was evaluated according to the inclusion and exclusion criteria to determine the study subjects. Clinical data and information related to ultrasound imaging, diagnosis and treatment of cytopathology, and post-operative pathological examination were collected for each subject. The ultrasound features of patients with benign and malignant nodules were compared. Taking the result of post-operative histopathologic examination as the gold standard, the area under the curve (AUC) value was calculated via receiver operator characteristic (ROC) curve to determine the diagnostic value of US-FNAC for the pathological natures of thyroid nodules.
Finally, the patients were divided into groups Q1, Q2, Q3, and Q4 according to the median and quartile of nodular diameters to further evaluate US-FNAC’s diagnostic efficacy for the pathological natures of thyroid nodules with different diameters.
Examination and evaluation methods
Surgical pathological examination and evaluation
During the resection of thyroid nodules, all patients underwent resection of lesion nodules under general anesthesia, and a rapid pathological examination of diseased thyroid tissues was carried out. The collected specimens were transferred to the pathology department for assessment by two experienced pathologists at the level of attending physician or above. Consultation was necessary to obtain a unified diagnostic result if different opinions existed.
Typical cancer cells in the specimens were assessed as malignant, and non-typical cancer cells were assessed as benign.
Ultrasound examination and evaluation
The color ultrasound diagnosis equipment (model: Philips EPQ5) with L12–5 probe was selected for ultrasound examination, and the probe frequency was 5–12 MHz. The patient was guided to adopt a supine position, and the pillow was placed behind the patient’s neck to tilt the head backward. After fully exposing the neck skin, ultrasound detected the bilateral thyroid lobes and isthmus and observed nodular location, size, number, morphological characteristics, blood flow, internal echo, and calcification situations.
According to the American Thyroid Association (ATA) guidelines, the ultrasound examination results could be divided into five types.[16]
Benign
Simple cystic nodules (no solid component).
Super-low suspected malignancy
Spongiform or partially cystic nodules without any of the ultrasound features described in low, moderate, or high suspected pattern.
Low suspected malignancy
Solid nodules with equal or high echo or partially cystic nodules with eccentric solidity. Moderate suspected malignancy
Solid nodules with low echo and smooth margins.
High suspected malignancy
Solid nodules (components) with a low echo of a partially cystic nodule with one or more of the characteristics including irregular edges (infiltrative, microlobulated), microcalcification, longer than wide shape, edge calcification combined with small prominent soft tissue component, and the evidence of extrathyroid extension.
US-FNAC examination and evaluation
According to the results of clinical and ultrasound examinations, the most suspected thyroid nodule was examined through US-FNAC. After disinfection and towel treatment, 2% lidocaine (NMPA approval no.: H37022114; specification: 5 mL: 0.1 g, manufacturer: Shandong Hualu Pharmaceutical Co., Ltd.; origin: Liaocheng, China) at a dose of 50–300 mg was used for local infiltration anesthesia. A 22 G fine needle was selected to puncture the corresponding suspected nodules under ultrasound guidance [Figure 1]. The multi-directional puncture should reach the nodular internals to obtain contents as much as possible. Negative pressure suction was reasonably adopted if the tissue was difficult to extract. If the aspirate contained more blood, the remaining blood was aspirated completely from various directions using a syringe after slightly shaking the glass slide, and then, the suction operations were performed three times, subsequently obtaining specimens. The syringe was withdrawn, the needlepoint was pressed with gauze, and the specimens were placed in the slide, and the slide method was used for examination. Two experienced pathologists (attending physician or above) evaluated the results. When there were different opinions, consultation was needed, and the final diagnosis results were obtained after the unification of opinions.
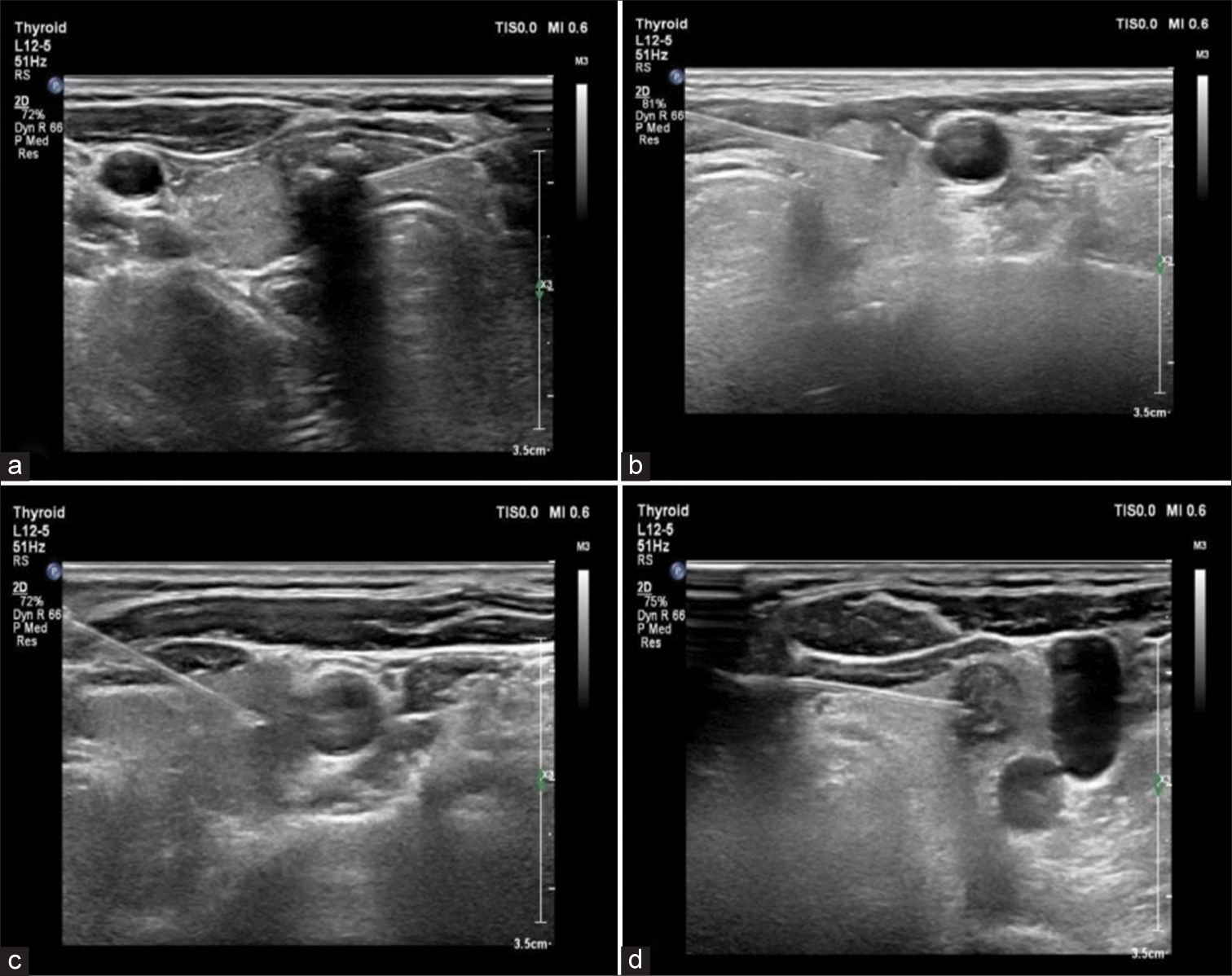
- Ultrasound-guided puncture images in ultrasound-guided fine-needle aspiration cytology. (a) A low-echo nodule puncture was observed in the right lobe of the thyroid, and (b-d) was displayed in the left lobe of the thyroid.
According to US-FNAC results, patients could be divided into the following six types.[17]
Patients with non-diagnostic or unsatisfactory specimen results were classified as type I
Patients with benign lesions were classified as type II
Patients showing atypical cellular lesions with unclear diagnostic significance were classified as type III
Patients with suspected or existing follicular tumors belonged to type IV
Patients with suspected malignant tumors were classified as type V
Patients with definitely diagnosed malignant tumors were classified as type VI.
Statistical analysis
The pre-operative US-FNAC and post-operative paraffin pathology results of all patients with thyroid nodules were entered into the SPSS database (version: 26.0, developer: IBM Corporation; Armonk, State of New York, USA). The categorical variables were expressed as (n [%]) and tested by Fisher’s exact probability or the correction formula of the chi-square test, and continuous variables were tested by the Shapiro–Wilk test and the data meeting non-normal distribution were expressed as M (P25, P75). ROC curves were used to evaluate the diagnostic efficacy of US-FNAC. When AUC > 0.5, the AUC closer to 1 indicates a better diagnostic effect (i.e., AUC = 0.5–0.7 indicates low accuracy, AUC=0.7–0.9 indicates a certain accuracy, and AUC > 0.9 indicates high accuracy). Microsoft Office Word 2006 (Microsoft Corporation; Redmond, WA, USA) and SPSS software were used to create figures.
RESULTS
Baseline data
This study selected a cohort of 116 patients, of which 98 met the inclusion criteria [Figure 2]. Of these, 53 were female (54.08%) and 45 were male (45.92%), with an average age of 53.46 ± 6.62 years (ranging from 32–76 years).
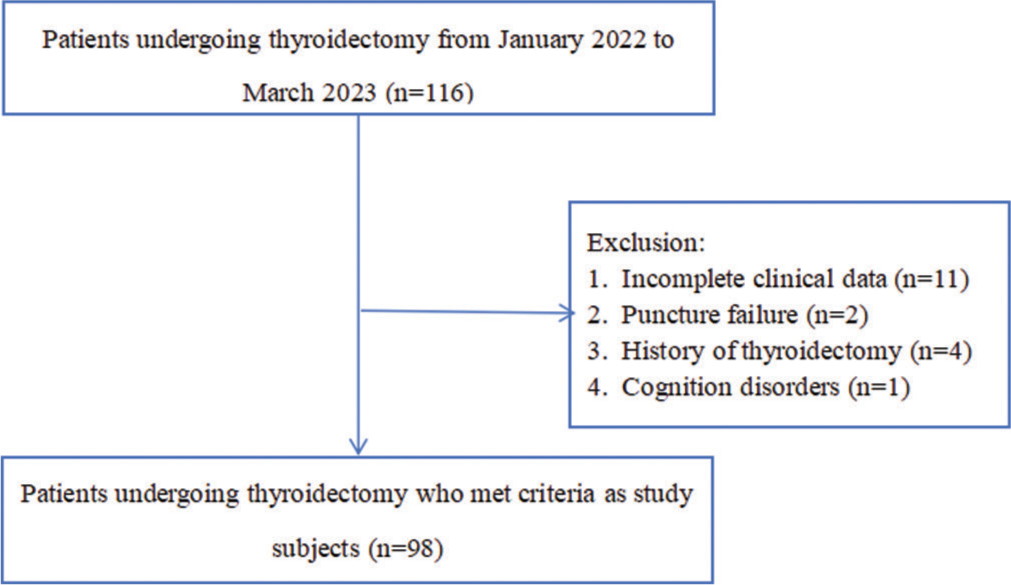
- Inclusion process of patients.
Results of surgical pathological examination
In this study, 98 nodules were punctured, with a diameter of 0.8–5.2 cm and a median and quartile of (1.98 ± 0.70) cm, including 10 (10.20%) benign nodules and 88 (89.80%) malignant nodules, as shown in Table 1.
| Surgical results | Pathological types | Number (n[%]) |
|---|---|---|
| Benign | 10 (10.20) | |
| Subacute thyroiditis | 4 (4.08) | |
| Hashimoto’s thyroiditis | 3 (3.06) | |
| Oncocytoma | 2 (2.04) | |
| Atypical follicular adenoma | 1 (1.02) | |
| Malignant | 88 (89.80) | |
| Papillary carcinoma | 77 (78.57) | |
| Medullary carcinoma | 7 (7.15) | |
| Undifferentiated carcinoma | 4 (4.08) |
Ultrasonic classification and features
According to ATA guidelines, 98 thyroid nodules were classified, including 14 (14.29%) benign nodules and 84 (85.71%) suspected malignant nodules. The specific ultrasound classification results are shown in Table 2. The composition, echo, calcification, edge, and shape of benign thyroid nodules were significantly different from those of malignant thyroid nodules (P < 0.05), and the specific ultrasonic features are shown in Table 3.
| Ultrasound classification | Number (n[%]) |
|---|---|
| Benign | 14 (14.29) |
| Super-low suspected malignancy | 16 (16.33) |
| Low suspected malignancy | 28 (28.57) |
| Moderate suspected malignancy | 11 (11.22) |
| High suspected malignancy | 29 (29.59) |
US-FNAC RESULTS
| Ultrasonic features | Number (n=98) | Surgical pathological results | χ2/Fisher | P-value | |
|---|---|---|---|---|---|
| Benign (n=10) | Malignant (n=88) | ||||
| Composition | |||||
| Solid-cystic | 20 (20.41) | 5 (50.00) | 15 (17.05) | 4.146 | 0.042 |
| Solid | 78 (79.59) | 5 (50.00) | 73 (82.95) | ||
| Echo | |||||
| Low/super-low echo | 70 (71.43) | 4 (40.00) | 66 (75.00) | 4.830 | 0.028 |
| Equal/high echo | 28 (28.57) | 6 (60.00) | 22 (25.00) | ||
| Calcification | |||||
| Micro calcification | 44 (44.90) | 1 (10.00) | 43 (48.86) | Fisher | 0.034 |
| Coarse calcification | 15 (15.31) | 3 (30.00) | 12 (13.64) | ||
| No calcification | 39 (39.80) | 6 (60.00) | 33 (37.50) | ||
| Edge | |||||
| Irregular edge | 76 (77.55) | 5 (50.00) | 71 (80.68) | 4.132 | 0.042 |
| Smooth/regular edge | 22 (22.45) | 5 (50.00) | 17 (19.32) | ||
| Shape | |||||
| Aspect ratio<1* | 25 (25.51) | 8 (80.00) | 17 (19.32) | 14.354 | <0.001 |
| Aspect ratio>1# | 73 (74.49) | 2 (20.00) | 71 (80.68) | ||
The US-FNAC results of 98 thyroid nodules showed 9 (9.18%) benign nodules, 84 (85.72%) malignant nodules, and 5 (5.10%) uncertain pathological natures, as shown in Table 4 and Figure 3.
| Classifications | Pathological natures | Total |
|---|---|---|
| Type I | Uncertain | 2 (2.04) |
| Type II | Benign | 9 (9.18) |
| Type III | Uncertain | 3 (3.06) |
| Type IV | Malignant | 29 (29.59) |
| Type V | Malignant | 39 (39.80) |
| Type VI | Malignant | 16 (16.33) |
US-FNAC: Ultrasound-guided fine-needle aspiration cytology, Type I-VI:
Patients with non-diagnostic or unsatisfactory specimen results were classified as type I.
Patients with benign lesions were classified as type II.
Patients showing atypical cellular lesions with unclear diagnostic significance were classified as typeIII.
Patients with suspected or existing follicular tumors belonged to type IV.
Patients with suspected malignant tumors were classified as type V.
Patients with definitely diagnosed malignant tumors were classified as type VI.
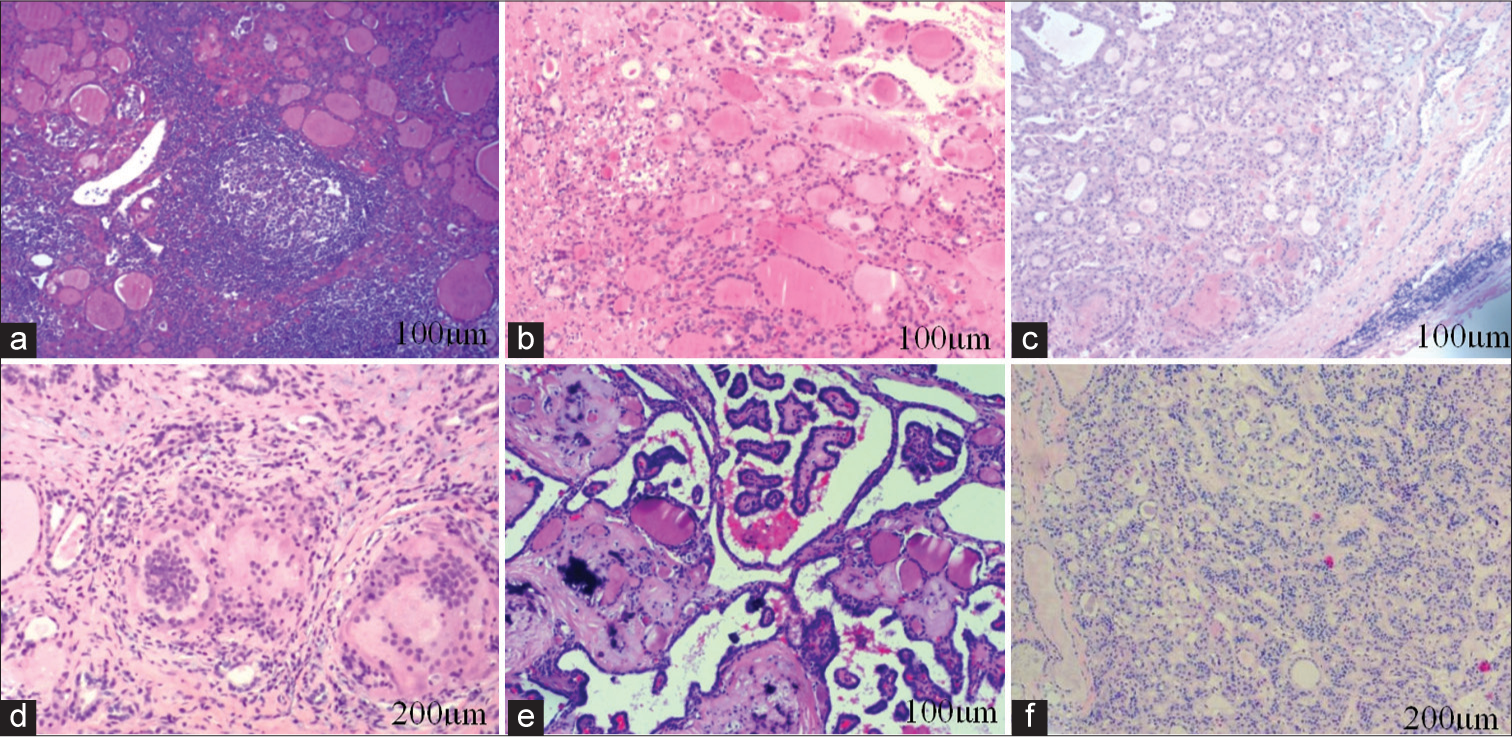
- Cytopathology in patients with thyroid nodules by ultrasound-guided fine-needle aspiration cytology. (a) Hashimoto’s thyroiditis. Lymphadenia, formation of lymphoid follicles, and acidophilic degeneration of follicular epithelium among thyroid follicles were observed (100 µm). (b) Atypical fo llicular adenoma. Rich neoplastic cells, inconspicuous follicular structure in some areas, and mild heterogenic cells were observed (100 µm). (c) Onco1cytoma. The eosinophilic infiltration of thyroid cells, consistent nuclear size, obscure heteromorphism, and complete fibrous capsule around thyroid follicles were observed, and no capsule and vascular invasion were observed (100 µm). (d) Subacute thyroiditis. Destroyed thyroid follicles and overflowed colloids, the infiltration of fibroblast hyperplasia, lymphocytes, plasma cells, neutrophils, and eosinophils, and the reaction of histiocytes and multinucleated giant cells were observed (200 µm). (e) Papillary thyroid carcinoma. Papillary structure and gravel-like calcification could be found (100 µm). (f) Medullary thyroid carcinoma. The cells were arranged in follicular, nested, and trabecular ways. The cytoplasm was bicolorophilic, the nucleus was round or oval, and the chromatin was coarse (200 µm). (3a-f: Hematoxylin and eosin)
Diagnostic efficacy of US-FNAC for the pathological natures of thyroid nodules
Because the benign and malignant natures of nodules in type I and type III could not be determined, 93 cases were included after excluding nodules in type I and III. The result of the post-operative pathological examination was used as the gold standard for ROC analysis, showing that the AUC, sensitivity, specificity, and 95% confidence interval of US-FNAC were 0.894, 98.80%, 80.00%, and 0.745–1.000, respectively, as shown in Table 5 and Figure 4.
| Benign | Malignant | AUC | Sensitivity (%) | Specificity (%) | 95% CI | |
|---|---|---|---|---|---|---|
| US-FNAC (n=93) | ||||||
| Benign | 8 | 1 | 0.894 | 98.80 | 80.00 | 0.745~1.000 |
| Malignant | 2 | 82 |
US-FNAC: Ultrasound-guided fine-needle aspiration cytology, CI: Confidence interval, AUC: Area under the curve
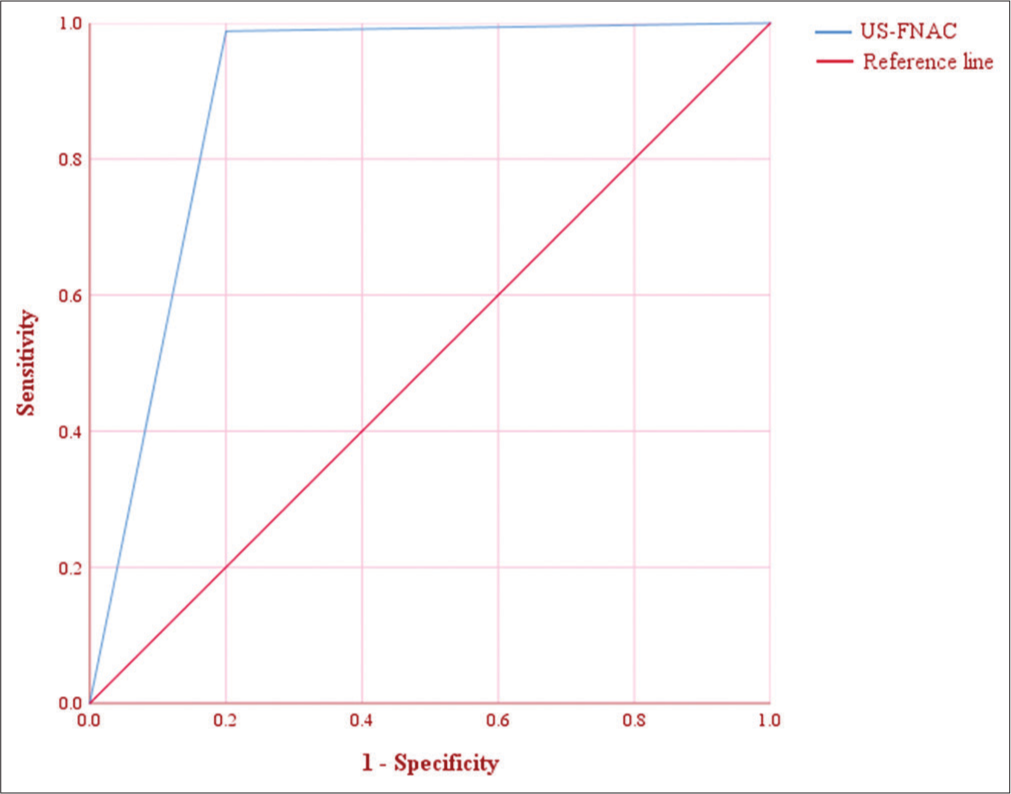
- Receiver operator characteristic curve of ultrasound-guided fine-needle aspiration cytology diagnosis. (US-FNAC: Ultrasound-guided fine-needle aspiration cytology)
Diagnostic efficacy of US-FNAC for pathological natures of thyroid nodules with different diameters
According to the median and quartile of nodular diameters, i.e., 1.90 (1.60, 2.30) cm, 93 patients were divided into groups Q1 (≤1.6 cm), Q2 (1.7–1.9 cm), Q3 (2.0–2.3 cm), and Q4 (>2.3 cm). The results of ROC analysis showed that the AUCs of US-FNAC in the above groups were 0.978, 1.000, 0.977,0.971. The AUCs of Q1 group, Q2 group, Q3 group and Q4 group were all > 0.9, and US-FNAC had high diagnostic efficiency for the pathological properties of thyroid nodules with different diameters, as shown in Table 6 and Figure 5.
| Groups | Surgical pathological examination results | AUC | Sensitivity (%) | Specificity (%) | 95% CI | |
|---|---|---|---|---|---|---|
| Benign | Malignant | |||||
| Group Q1 (n=24) | ||||||
| Benign | 1 | 1 | 0.978 | 95.70 | 100.00 | 0.914-1.000 |
| Malignant | 0 | 22 | ||||
| Group Q2 (n=26) | ||||||
| Benign | 3 | 0 | 1.000 | 100.00 | 100.00 | 0.000 –1.000 |
| Malignant | 0 | 23 | ||||
| Group Q3 (n=24) | ||||||
| Benign | 2 | 0 | 0.977 | 100.00 | 66.70 | 0.818-1.000 |
| Malignant | 1 | 21 | ||||
| Group Q4 (n=19) | ||||||
| Benign | 2 | 0 | 0.971 | 100.00 | 66.7 | 0.774-1.000 |
| Malignant | 1 | 16 | ||||
US-FNAC: Ultrasound-guided fine-needle aspiration cytology, AUC: Area under the curve, CI: Confidence interval, 93 patients were divided into groups Q1 (≤1.6 cm), Q2 (1.7–1.9 cm), Q3 (2.0–2.3 cm), and Q4 (>2.3 cm).
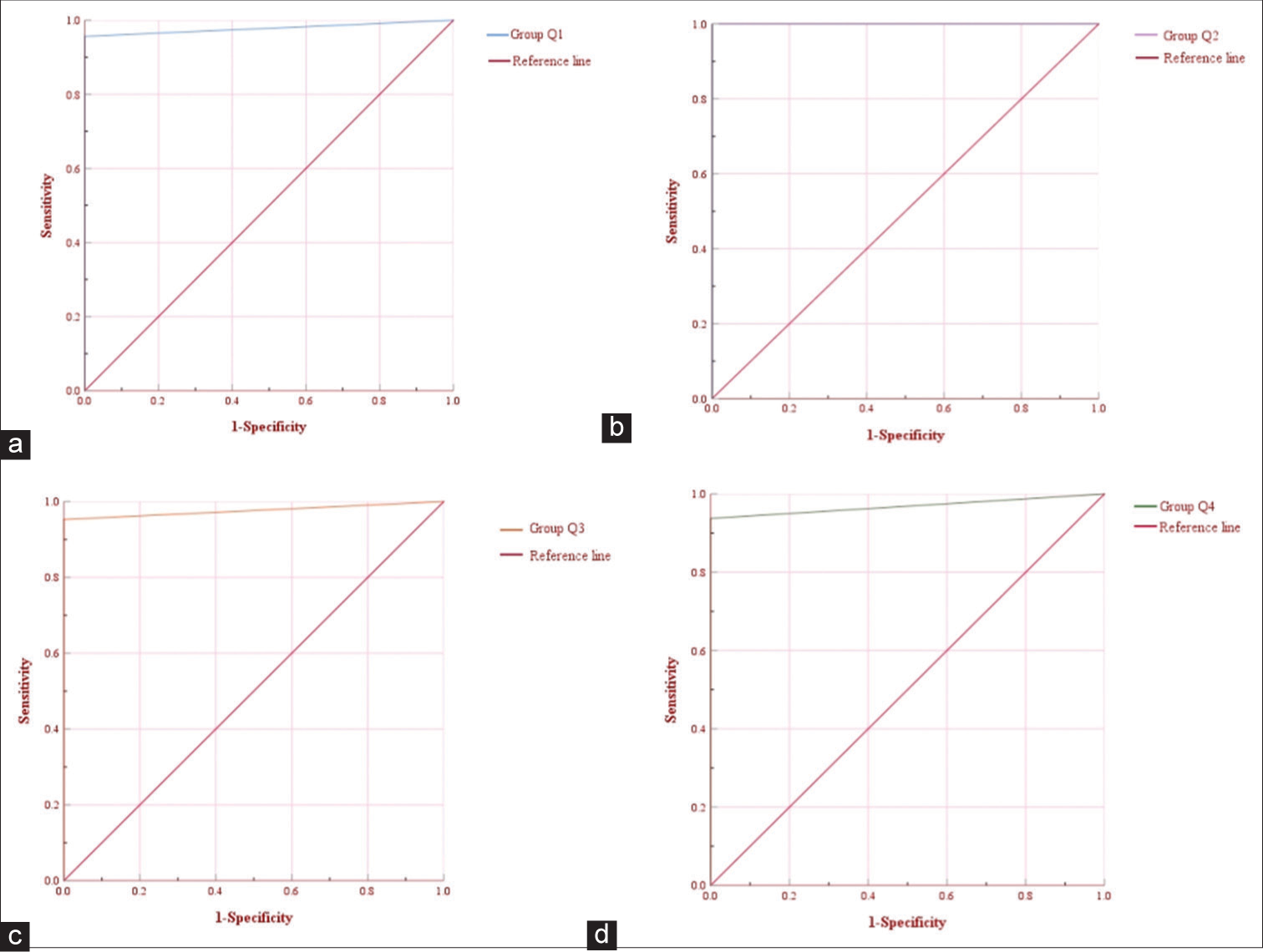
- Receiver operator characteristic (ROC) curve of ultrasound-guided fine-needle aspiration cytology (US-FNAC) in diagnosing pathological natures of thyroid nodules with different diameters. (a-d) Shows the ROC curve of US-FNAC in the diagnosis of groups Q1, Q2, Q3 , and Q4. 93 patients were divided into groups Q1 (≤1.6 cm), Q2 (1.7–1.9 cm), Q3 (2.0–2.3 cm), and Q4 (>2.3 cm).
DISCUSSION
Fine-needle aspiration cytology and ultrasonic examination are key tools for pre-operative evaluation of patients with thyroid lesions.[18-20] Ultrasound examination provides a reference for nodular selection in US-FNAC. Ultrasound guidance assists physicians in seeking a more accurate puncture path and the best puncture position, thus effectively avoiding blood vessels and nerves and improving the success rate of puncture while ensuring safety. In comparison with palpation-guided fine-needle aspiration cytology, USFNAC has higher accuracy.[21] A foreign study indicated that ultrasound features such as low echo, fine calcification, irregular edge, and nodular aspect ratio >1 were potential indicators of malignant thyroid nodules.[22] This is consistent with the result of the analysis of this study, which fully confirms the application value of ultrasonic examination in fine-needle aspiration cytology of thyroid nodules.
The US-FNAC results in this study showed 9 (9.18%) benign nodules, 84 (85.72%) malignant nodules, and 5 (5.10%) nodules with uncertain pathological natures 2 (2.04%) specimens had unsatisfactory diagnoses, and 3 (3.06%) specimens were atypical cellular lesions with unclear diagnostic significance). According to surgical pathology results, two benign nodules and one malignant nodule were not correctly diagnosed in this study, including that two nodules were diagnosed as Hashimoto’s thyroiditis by pre-operative US-FNAC but were diagnosed as papillary carcinoma by surgery. Hou et al.[23] have also obtained similar results, finding that Hashimoto’s thyroiditis, a risk factor for the increase of false-negative rate, would reduce the diagnostic accuracy of US-FNAC. There may be two main reasons for this phenomenon, uniform lesions can result in omission during the puncture process, and second, insufficient experience among physicians can lead to incorrect cytopathologic diagnoses. In addition, one nodule was diagnosed with a malignant tumor by pre-operative USFNAC but was diagnosed as Hashimoto’s thyroiditis by surgical pathology, speculating that it may be related to the limitations of US-FNAC. US-FNAC is based on ultrasonic features, but some benign nodules are easily misdiagnosed as malignant tumors because of irregular edges and uneven echoes.
It has been reported that the accuracy of US-FNAC may also be affected by the size of thyroid nodules.[24,25] In response to this problem, this study divided the patients into four groups according to the median and quartile. Statistical analysis found the AUCs of groups Q1, Q2, Q3, and Q4>0.9, and USFNAC had high diagnostic efficiency for the pathological properties of thyroid nodules with different diameters. We speculate that this may be related to the small number of cases in our study. The needle may slide out of the nodule during sampling or enter the normal tissue. In addition, Zhao et al.[26] point out that nodular size has a certain effect on the positive rate of fine needle aspiration, mainly due to the lower diagnostic efficiency of conventional ultrasound on suspected malignant features in small nodules. Therefore, it is necessary to actively perform long-term follow-up for patients with thyroid nodules in types I and III through US-FNAC and patients with small nodular diameters and perform repeat punctures if necessary.
However, US-FNAC diagnosis is also susceptible to factors such as clinical physicians’ diagnostic experience and proficiency.[27-29] In this study, two patients were excluded due to inexperienced physicians who caused puncture failure, with an incidence of 1.90% (2/105) when screening patients, and this situation needs attention, although the incidence is not high. It is advocated that experienced physicians should perform US-FNAC, and patients should experience comprehensive evaluation before puncture to minimize the occurrence of adverse conditions such as insufficient sample acquisition, diluted blood cells caused by bleeding at the puncture site, and failure of puncture to reach the lesion site, thereby improving the effectiveness, accuracy, and safety of US-FNAC.
There are some limitations in this study. First, among patients undergoing US-FNAC, most patients with malignant nodules and few patients with benign nodules will receive surgical treatment, so selection bias occurred. Second, this single-center study had small sample numbers, so subsequent studies need to extend the observation time and increase the samples. Finally, the different studies had multiple grouping criteria for nodular size, affecting the study results. Therefore, complete verification should be taken by including more samples and conducting multiple studies to provide more reliable information for clinical work.
SUMMARY
US-FNAC has a high diagnostic efficiency for the pathological properties of thyroid nodules. Whether the nodule diameter has an effect on the accuracy of this method requires more clinical evidence.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author upon reasonable request.
ABBREVIATIONS
US-FNAC- ultrasound-guided fine-needle aspiration cytology ROC- receiver operator characteristic ATA- American Thyroid Association
AUTHOR CONTRIBUTIONS
GX: Interpreted the data and wrote the manuscript; WT: Designed the study; WT and GX: Contributed to writing the manuscript. All authors read and approved the final version of the manuscript. All authors read and approved the final manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the ethics committee of Zibo Central Hospital, Approval No. 2024052. Considering the anonymity of data, informed consent was waived. The study was conducted in accordance with the Declaration of Helsinki.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
EDITORIAL/PEER REVIEW
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through an automatic online system.
FUNDING
Not applicable.
References
- Association between Hashimoto's thyroiditis and papillary thyroid carcinoma: A retrospective analysis of 305 patients. BMC Endocr Disord. 2019;19(Suppl 1):26.
- [CrossRef] [PubMed] [Google Scholar]
- SuperSonic shear imaging for the differentiation between benign and malignant thyroid nodules: A meta-analysis. J Endocrinol Invest. 2022;45:1327-39.
- [CrossRef] [PubMed] [Google Scholar]
- Use of strain ultrasound elastography versus fine-needle aspiration cytology for the differential diagnosis of thyroid nodules: A retrospective analysis. Clinics (Sao Paulo). 2020;75:e1594.
- [CrossRef] [PubMed] [Google Scholar]
- Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: A review for pathologists. Mod Pathol. 2018;31:39-55.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of molecular testing with three molecular markers on thyroid fine-needle aspiration cytology with abnormal category. Diagn Cytopathol. 2020;48:507-15.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided fine needle aspiration cytology of angiosarcoma of head and neck: A review of cytomorphologic features and discussion of diagnostic pitfall of aspiration cytology of vascular lesions. Diagn Cytopathol. 2021;49:902-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fine needle aspiration cytology of thyroid nodule: Diagnostic accuracy and pitfalls. J Ayub Med Coll Abbottabad. 2006;18:26-9.
- [Google Scholar]
- Chondroid syringoma of the axilla: A potential for misdiagnosis as metastatic carcinoma on fine needle aspiration cytology. Diagn Cytopathol. 2022;50:E315-9.
- [CrossRef] [Google Scholar]
- The accuracy of fine needle aspiration cytology in the clinical diagnosis of minor salivary gland tumours. Int J Oral Maxillofac Surg. 2021;50:1408-12.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid carcinoma, version 2.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20:925-51.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of modified cell block cytology compared to fine needle aspiration cytology for diagnostic oral cytopathology. Biotech Histochem. 2021;96:197-201.
- [CrossRef] [PubMed] [Google Scholar]
- Cyto-morphological features of parathyroid lesions: Fine-needle aspiration cytology series from an endocrine tumor referral center. Diagn Cytopathol. 2022;50:75-83.
- [CrossRef] [PubMed] [Google Scholar]
- Fine needle aspiration cytology for two cases of ameloblastoma-Key highlights and diagnostic features. Cytopathology. 2023;34:91-3.
- [CrossRef] [PubMed] [Google Scholar]
- A radiologist's perspective of the value of ultrasound-guided fine needle aspiration cytology in the assessment of head and neck lesions. Cytopathology. 2021;32:394-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic utility of fine needle aspiration cytology in pediatric thyroid nodules based on Bethesda classification. J Pediatr Endocrinol Metab. 2021;34:449-55.
- [CrossRef] [PubMed] [Google Scholar]
- 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1-133.
- [CrossRef] [PubMed] [Google Scholar]
- The Bethesda system for reporting thyroid fine-needle aspiration specimens. Am J Clin Pathol. 2010;134:343-4.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided fine needle aspiration cytology and ultrasound examination of thyroid nodules in the UAE: A comparison. PLoS One. 2021;16:e0247807.
- [CrossRef] [PubMed] [Google Scholar]
- How accurate is fine-needle aspiration cytology (FNAC) for thyroid lesion: A correlation of FNAC with histopathology. J Family Med Prim Care. 2023;12:15-20.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of ultrasound scans as compared to fine needle aspiration cytology in the diagnosis of thyroid nodules. Cureus. 2023;15:e35108.
- [CrossRef] [Google Scholar]
- Diagnostic accuracy of palpation versus ultrasound-guided fine needle aspiration biopsy for diagnosis of malignancy in thyroid nodules: A systematic review and meta-analysis. BMC Endocr Disord. 2022;22:181.
- [CrossRef] [PubMed] [Google Scholar]
- The comparison of accuracy of ultrasonographic features versus ultrasound-guided fine-needle aspiration cytology in diagnosis of malignant thyroid nodules. J Ultrasound. 2019;22:315-21.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of Hashimoto's thyroiditis on the diagnostic efficacy of ultrasound-guided fine needle aspiration cytology for thyroid nodules = 1 cm. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2021;35:807-12.
- [Google Scholar]
- Malignancy risk for thyroid nodules larger than 4 cm and diagnostic reliability of ultrasound-guided FNAB results. Turk J Surg. 2019;35:13-8.
- [CrossRef] [PubMed] [Google Scholar]
- Size and ultrasound features affecting results of ultrasound-guided fine-needle aspiration of thyroid nodules. J Ultrasound Med. 2018;37:1367-77.
- [CrossRef] [PubMed] [Google Scholar]
- Positive rate and accuracy of ultrasound-guided fine-needle aspiration cytology for detecting suspected thyroid carcinoma nodules of different sizes. Nan Fang Yi Ke Da Xue Xue Bao. 2020;40:693-7.
- [Google Scholar]
- Independent risk factors and feasibility of ultrasound diagnosis of ultrasound-guided non-cytologically diagnostic thyroid nodules. Gland Surg. 2021;10:2724-33.
- [CrossRef] [PubMed] [Google Scholar]
- The value of ultrasound-guided fine-needle aspiration cytology combined with puncture feeling in the diagnosis of thyroid nodules. Acta Cytol. 2021;65:368-76.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing the sample adequacy of ultrasound-guided fine-needle aspiration from solid thyroid nodules for liquid-based cytology: A demographic, sonographic, and technical perspective. Medicina (Kaunas). 2022;58:1639.
- [CrossRef] [PubMed] [Google Scholar]








