Translate this page into:
Fine-needle aspiration of axillary swelling: Cytodiagnosis of an unusual presentation of filariasis
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Lymphatic filariasis is a major public health problem in tropical and subtropical countries. Fine-needle aspiration cytology (FNAC) is not routinely used for its identification. However, it has been detected incidentally, while doing FNAC for the evaluation of other lesions. We describe a presentation of occult filariasis with microfilariae (mf) in an isolated axillary swelling wherein FNAC was helpful in establishing the diagnosis.
Keywords
Filariasis
microfilariae
occult
INTRODUCTION
Filariasis is a major health problem in a tropical country like India. A majority of the infected individuals in filariasis are asymptomatic.[1] The most common presentation of the disease is asymptomatic or subclinical microfilaremia, hydrocele, acute adenolymphangitis, and chronic lymphatic disease.[1] Occult infections can be caused by Wuchereria bancrofti or Brugia malayi with no detectable microfilariae (mf) in the peripheral circulation. These include different clinical conditions such as tropical pulmonary eosinophilia, monoarthritis, and endomyocardial fibrosis, resulting from the pathology mediated by filarial parasites or host's immune response against infection.[2]
Incidental detection of microfilaria in an isolated axillary swelling is unusual. We report such a case which was diagnosed on fine-needle aspiration cytology (FNAC).
CASE REPORT
A 38 Year old female patient, resident of district Gonda, Uttar Pradesh presented with the chief complaints of a painless swelling in the left axillary region for the past 5 months. She had no history of fever, cough, weight loss, or any other swelling elsewhere in the body.
Local examination revealed a nontender mass with limited mobility measuring 3 cm × 2 cm with heterogeneous (soft to firm) consistency [Figure 1a]. General examination revealed the absence of palpable peripheral lymphadenopathy.
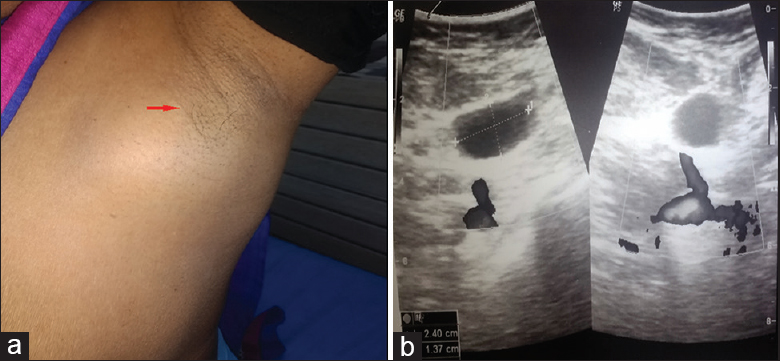
- (a) Swelling over the left axillary region, (b) Ultrasonography image showing ovoid solid mass in the left axilla with echogenic core
A provisional diagnosis of tubercular axillary lymphadenitis was considered. Ultrasonography revealed a well-defined ovoid solid mass in the left axilla measuring 50 mm × 22 mm with echogenic core [Figure 1b]. Morever, small cystic area was seen along posterior surface measuring 24 mm × 13 mm. A radiological diagnosis of large reactionary lymphadenitis was made.
Fine-needle aspiration from the swelling was performed and yielded 9 ml of hemorrhagic fluid. The smears revealed multiple sheathed, coiled, slightly curved mf of bancrofti with the prominence of lymphocytes along with the presence of few eosinophils in a proteinaceous background [Figures 2a and b]. On FNAC, a diagnosis of filarial parasitic infestation was made. Complete blood count revealed eosinophilia (15%) with absolute eosinophil count of 1680/μl of the blood. Peripheral blood smear examination did not reveal microfilaria. The patient was started on diethylcarbamazine citrate, and on follow-up, the swelling reduced.
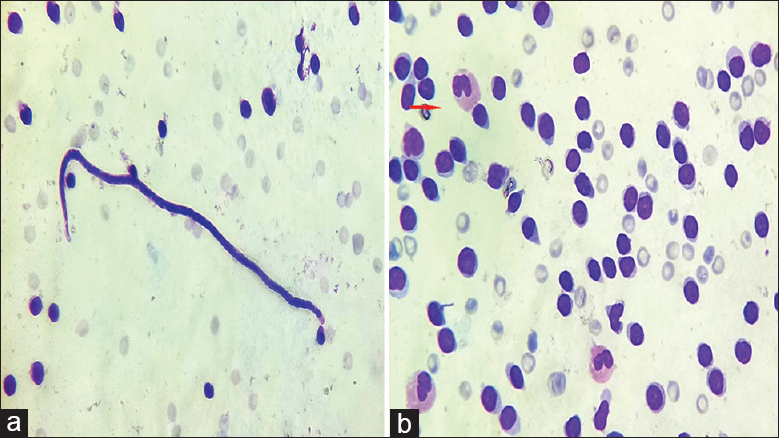
- (a) Sheathed microfilaria consistent with morphology of Wuchereria bancrofti admixed with lymphocytes (Papanicoloau, ×400). (b) Prominence of lymphocytes along with presence of few eosinophils in the background (Giemsa, ×400)
DISCUSSION
Filariasis is a major public health problem in tropical countries, including India. It is caused by nematodes wuchereria bancrofti, Brugia malayi, Brugia timori, Loa loa, Onchocerca volvulus, Mansonella perstans, and Mansonella ozzardi.[12] W. bancrofti (95%) and B. malayi (5%) are the most common species causing filariasis in India.[1] Adult worms live in the lymphatic channels of the definitive host, and microfilaria is released and circulated in the peripheral blood. The disease most frequently involves lymphatics of the lower limbs, retroperitoneal tissue, spermatic cord, epididymis, and mammary gland.[3] mf has been identified cytologically by FNAC at unusual sites, such as epitrochlear lymph node, axillary lymph node, breast, spleen, ovarian fluid, bone marrow, thyroid, and liver space-occupying lesion.[4] It has also been reported in various other exfoliative samples.[5] The filarial worm in the tissue fluids and exfoliated surface material probably occurs owing to conditions causing lymphovascular obstruction resulting in extravasations of blood and release of mf.[5]
Axillary involvement is an uncommon presentation of filariasis even in endemic communities. Basu et al. reported a case of in large mass of axilla in the background of reactive lymphoid population.[1]
Rare reports of microfilaria have been noted in the axillary cystic swelling in clinically unsuspected cases of filariasis with the absence of microfilariae in the peripheral blood. Axillary swelling can raise suspicion of tubercular lymphadenopathy especially in a country with increased incidence of tuberculosis like India.
Monoclonal antibodies against circulating filarial antigen are used for diagnosis of filaria. Molecular biology techniques such as in situ hybridization (ISH), fluorescence ISH, and polymerase chain reaction are now available for specific diagnosis but are available only in specialized centers.[6] Limited reports are available in the literature highlighting the importance of FNAC as a diagnostic tool in the occult filariasis.
We reiterate that FNAC is a useful tool for early diagnosis of occult filariasis at unusual sites. Patients with axillary swelling may be clinically mistaken for tuberculosis, and FNAC resolves it by demonstration of the larva without needing further tests for confirmation of filariasis.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
ETHICS STATEMENT BY ALL AUTHORS
As this is a case report without identifiers, our institution does not require approval from institutional Review Board (IRB).
LIST OF ABBREVIATIONS (In alphabetic order)
B.malayi - Brugia malayi
B.timori - Brugia timori
DEC - Diethylcarbamazine
Mf - Microfilariae
SOL - Space occupying lesion
W.bancrofti - Wuchereria bancrofti
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (the authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Lymphadenovarix in the axilla - An unusual presentation of filariasis. Filaria J. 2006;5:9.
- [Google Scholar]
- Isolated epitrochlear filarial lymphadenopathy: Cytomorphological diagnosis of an unusual presentation. Turk Patoloji Derg 10.5146/tjpath. 2018.01423
- [Google Scholar]
- Microfilariae in association with neoplastic lesions: Report of five cases. Cytopathology. 2001;12:120-6.
- [Google Scholar]
- Cytodiagnosis of microfilaria at unusual sites. Indian J Clin Pract. 2014;25:535-7.
- [Google Scholar]
- Toward molecular parasitologic diagnosis: Enhanced diagnostic sensitivity for filarial infections in mobile populations. J Clin Microbiol. 2011;49:42-7.
- [Google Scholar]








