Translate this page into:
Macrofollicular variant of papillary carcinoma, a potential diagnostic pitfall: A report of two cases including a review of literature
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Macrofollicular variant of papillary thyroid carcinoma (MFVPTC) is one of the rarest histologic types of papillary carcinoma. This tumor may mimic an adenomatoid/colloid nodule or follicular neoplasm (macrofollicular type) both on histology and cytology. There are very few articles describing the cytologic features of MFVPTC. We report the cytologic findings of two surgically confirmed MFVPTC. The first case showed abundant thin colloid with moderate amount of follicular cells arranged in a honeycombed and syncytial pattern. Some but not all the follicular cells showed enlarged round to ovoid nuclei, overlapping nuclei, few nuclear grooves and rare intranuclear inclusions. The second case showed abundant thin colloid and predominantly benign appearing follicular cells with few overlapping nuclei, enlarged round to ovoid nuclei and rare nuclear grooves. No intranuclear inclusions were identified. A review of the literature was done and the cytologic findings of MFVPTC including our two cases were tabulated. The cytologic findings showed moderate to abundant thin with focally thick colloid in 75% of cases and sheet like arrangement of follicular cells in 76%. Although nuclear features such as chromatin clearing, overlapping and grooves were present in majority of cases, the quantity varied from rare to focal. Small to prominent nucleoli were present in all of the evaluable cases. Intranuclear inclusions were seen only in 45% of patients. Hence, the cytologic features of macrofollicular variant of papillary carcinoma though present can be subtle and intranuclear inclusions may not be present always.
Keywords
Fine needle aspiration
macrofollicular variant
papillary carcinoma
thyroid
INTRODUCTION
The cytologic diagnosis of classic papillary thyroid carcinoma when all the characteristic nuclear features are present is relatively straightforward. However, the macrofollicular variant of papillary thyroid carcinoma (MFVPTC) is a potential pitfall given the rarity of this histologic subtype and limited reports of its cytologic features.[12345678] The presence of abundant watery colloid, low to moderate cellularity, syncytial to monolayered cell arrangement, subtle and focal nuclear features associated with papillary carcinoma can lead to an erroneous diagnosis of an adenomatoid/colloid nodule or a follicular neoplasm (macrofollicular type). We report two cases of macrofollicular variant of papillary carcinoma (MFPC) and a review of the literature.
CASE REPORTS
Case 1
A 33-year-old woman presented with a 5-year history of thyroid nodule. She noted a recent increase in the size of the nodule. Although she had a family history of thyroid disease, there was no history of radiation exposure or prior malignancy. Thyroid stimulating hormone levels were normal.
An ultrasound of the thyroid gland showed a 3.9 cm solid, isoechoic nodule almost replacing the right lobe. An ultrasound guided fine needle aspiration (FNA) was performed. Air-dried smears were stained with Diff-Quik and ethanol fixed smears with Papanicolaou stain.
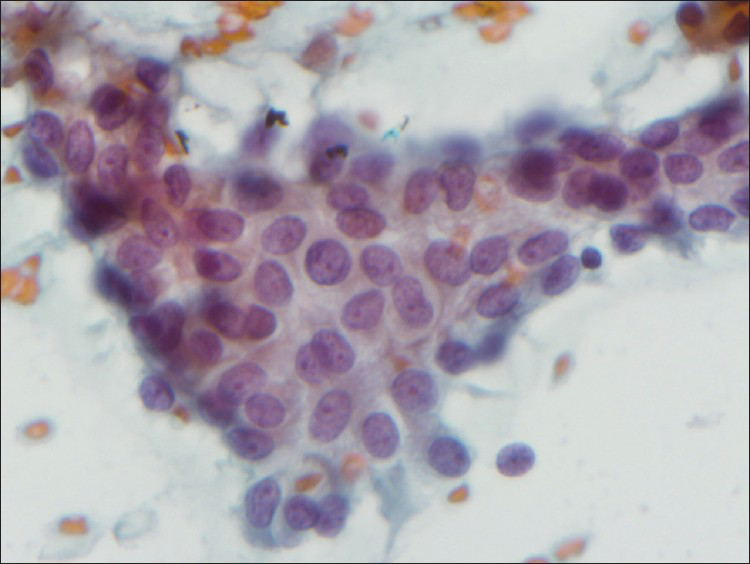
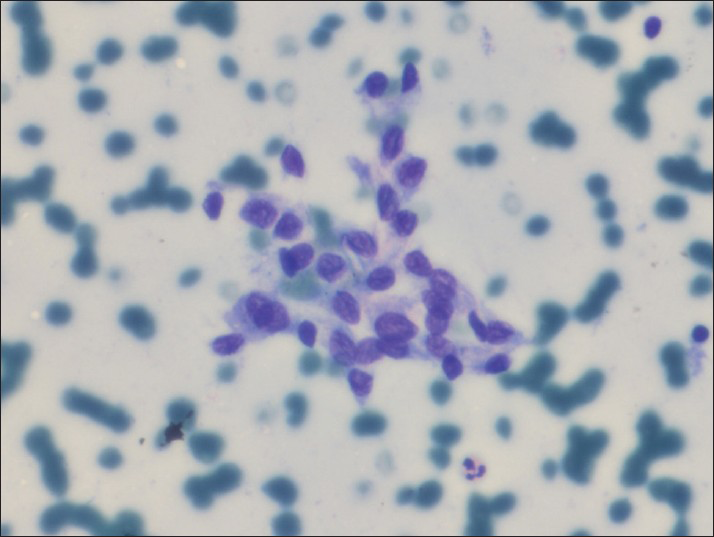
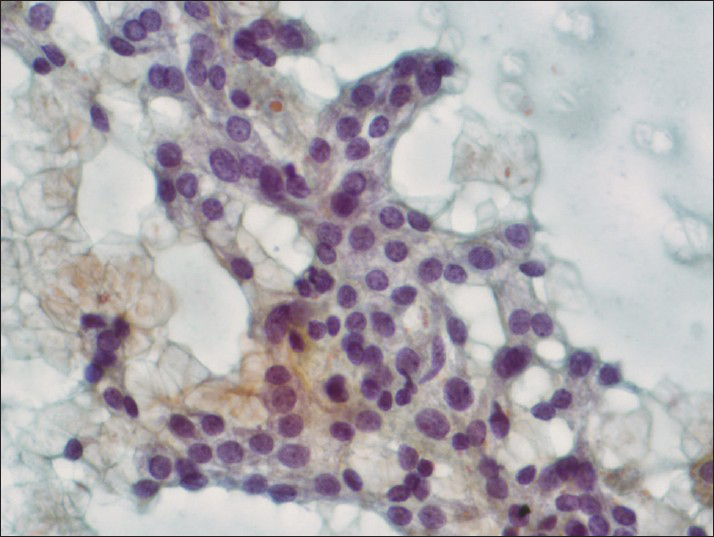
The Diff-Quik smears showed abundant thin colloid and moderate amount of follicular cells arranged in a honeycombed and syncytial pattern [Figure 1]. Some of the follicular cells showed nuclear overlapping enlarged round to ovoid nuclei, small prominent nucleoli and few nuclear grooves [Figure 2]. Rare intranuclear inclusions were also identified [Figure 3]. Few multinucleated giant cells were present. Nuclei with fine powdery chromatin pattern and small nucleoli were present on Papanicolaou stained smears [Figure 4]. The FNA was reported as suspicious for papillary thyroid carcinoma.
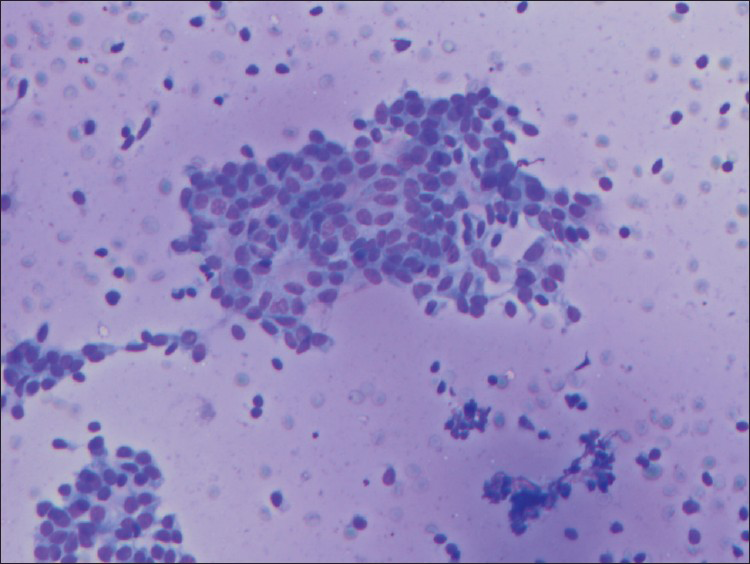
- Case 1. Abundant thin colloid and follicular cells arranged in honeycombed and syncytial pattern (Diff-Quik, ×200)

- Case 1. Follicular cells with enlarged round to ovoid nuclei, focally overlapping nuclei, and nuclear grooves (Diff-Quik, ×600)

- Case 1. Follicular cells with occasional intranuclear inclusions (Diff-Quik, ×600)
- Case 1. Follicular cells with fine nuclear chromatin pattern and small eccentrically located nucleoli (Papanicolaou, ×600)
A total thyroidectomy was performed. The right lobe weighed 42 g and measured 7.0 cm × 4.2 cm × 3.0 cm. Cut section showed a 4.0 cm × 3.8 cm × 3.0 cm well circumscribed encapsulated tan-pink nodule located at the inferior lobe. Microscopic examination showed an encapsulated tumor with predominance of macrofollicles lined by overlapping follicular cells with enlarged, optically clear nuclei, containing few nuclear grooves and rare intranuclear inclusions. The tumor was positive for Hector Battifora mesothelial cell-1 (HBME-1).
Case 2
A 55-year-old woman presented with a clinical history of hyperparathyroidism. An ultrasound of the thyroid gland revealed a right-sided 2.9 cm mixed echogenic nodule and a 0.6 cm isthmic nodule containing fine internal calcifications.
An ultrasound guided FNA of the right lobe was performed. Air dried smears were stained with Diff-Quik and ethanol fixed smears with Papanicolaou stain. The Diff-Quik smears showed abundant thin colloid and predominantly benign-appearing follicular cells arranged in monolayered pattern. However, other areas showed enlarged round to ovoid follicular cells with nuclear crowding and rare grooves [Figure 5]. Few follicular cells with occasional small nucleoli were also present [Figure 6]. No intranuclear inclusions were identified. Occasional multinucleated giant cells were present. The final diagnosis was atypia of undetermined significance (AUS). Although the Bethesda Recommendation for AUS is repeat FNA after a period of observation, based on the clinical presentation of patient and imaging studies, a total thyroidectomy was performed. The right lobe showed a 2.2 cm encapsulated nodule and two smaller ill-defined white firm nodules measuring 0.3 cm and 0.5 cm. No tumor was seen in the left lobe. Histologic sections from the 2.2 cm right lobe revealed a well-encapsulated tumor composed of colloid-filled macrofollicles occupying more than 50% of the nodule and admixed with smaller follicles. The epithelium of both small and large follicles showed nuclear overlapping, fine chromatin pattern, small eccentrically located nucleoli and few nuclear grooves. No intranuclear inclusions were identified. Capsular or vascular invasion was not identified. Immunohistochemical stain for HBME-1 was positive. The remaining two smaller nodules showed classic micropapillary thyroid carcinoma.
- Case 2. Follicular cells with enlarged round to ovoid overlapping nuclei and occasional nuclear grooves (Diff-Quik, ×400)
- Case 2. Follicular cells with focally enlarged round to ovoid nuclei and small nucleoli (Papanicolaou, ×400)
DISCUSSION
In 1991, Albores-Saavedra et al., described MFPC, a rare variant of follicular variant of papillary carcinoma (FVPC).[9] Their criteria for this variant included a combination of FVPC in which over 50% of the cross-sectional area of the tumor was composed of macrofollicles (follicle measuring more than 200 μm in diameter). The macrofollicles were lined either by cells with large ground-glass nuclei, large cells with pale nuclei and stippled chromatin or cuboidal cells with hyperchromatic nuclei. A few macrofollicles were lined by two or even all three of all the cell types. Nuclear grooves and cytoplasmic inclusions were found only in the cells with clear or ground-glass nuclei. All tumors had randomly distributed foci of conventional FVPC. Based on these criteria, it is not surprising that both the histologic and cytologic features could mimic follicular neoplasm (macrofollicular pattern) or an adenomatoid/colloid nodule.
There are very few reports describing the cytologic features of MFVPTC. In 1998, Mesonero et al., published the first cytologic findings of MFVPTC. They described the presence of follicular cells with round to ovoid nuclei, nuclear hypochromasia and nuclear grooves.[1] Nuclear pseudoinclusions and psammoma bodies were absent. The follicular cells were arranged in sheets, spherules and occasionally in small papillary tufts. Colloid was described as abundant, thick, in “chunks” or in thin films in the background and within spherules. Only one of their cases showed multinucleated-type giant cells. A month later, a report by Woyke et al., described the cytologic findings as containing numerous dispersed foamy histiocytes admixed with groups of small and large epithelial cells.[2] The small epithelial cells showed tightly arranged overlapping oval, slightly irregular hyperchromatic nuclei with delicate, pale and poorly defined cytoplasm. It was the presence of loosely arranged larger epithelial cells with centrally located round nuclei, powdery chromatin and well-defined eosinophilic cytoplasm containing intracytoplasmic and intranuclear vacuoles which prompted a cytologic diagnosis of cystic papillary thyroid carcinoma. The final diagnosis of MFVPTC was given only after histologic evaluation of the surgical specimen. Cystic degeneration of MFVPTC may have occurred in their case since this finding has been described by Gamboa-Dominguez et al., in 1 of their 6 cases of MFVPTC.[10] Hirokawa et al., described the presence of abundant dense and inspissated colloid and cohesive monolayered tumor cells with minimal nuclear pleomorphism, nuclear grooves, intranuclear inclusions and delicate cytoplasm.[3] There were no multinucleated giant cells, inflammatory cells, psammoma bodies or three-dimensional branching papillae with fibrovascular cores. Hernández-Ortiz et al., described similar cytologic findings of abundant eosinophilic colloid with monolayered sheets and fragments of follicular cells with enlarged round to oval nuclei, hypochromatic, powdery chromatin, small prominent nucleolus and few nuclear grooves with rare pseudoinclusions.[4] Hemosiderin laden macrophages but no giant cells were identified. Although most of these earlier papers described the presence of moderate to abundant colloid and moderate cellularity, the cases reported by Fadda et al., described small amount of colloid, scant cellularity, medium to large sized follicular cells with some clearing but no nuclear grooves or intranuclear inclusions.[5] Three cases reported by Lugli et al., described presence of nuclear grooves and ground glass chromatin in 2 of their 3 cases. One of their cases had no cytologic features of papillary carcinoma.[6] The largest series by Chung et al., described the abundance of colloid, macrophages, follicular cells arranged in macrofollicular pattern and/or absence of widespread cytologic features of papillary carcinoma.[7] A more recent paper by Bongiovanni et al., showed similar findings as one of Mesonero's cases except for the inconspicuous nucleoli. We tabulated the degree of cellularity, architecture, nuclear findings [Table 1] and background material [Table 2] of the previously published cytology cases of MFVPTC in the English literature and included our two cases. This table does not include reported cases, which primarily emphasized the surgical pathologic findings and those with very limited cytologic description. The more common nuclear findings on evaluable cases were as follows: Presence of round/ovoid nuclei, small eccentric to conspicuous nucleoli, chromatin clearing, nuclear overlapping and nuclear grooves. However, given the variability in the degree or quantity of nuclear features it might be difficult to completely rely on these features, since they can be rare to focal and nonspecific. Only 45% showed the presence of intranuclear inclusions, which ranged from rare to few. The heterogeneous appearance of MFVPTC, both in FNA specimens as well as in histologic sections, is probably the main reason for low sensitivity of FNA for MFPC.[7] The background material may also be a contributing factor leading to a false negative or benign diagnosis since 75% showed moderate to abundant thin with focally thick colloid. Macrophages were present in 73%; a finding which may be seen in cystic degeneration of a colloid nodule or cystic papillary thyroid carcinoma. No psammoma bodies were identified in 11 of the evaluable cases. Hence, the cytologic findings are not specific and defining the cytologic criteria for MFPC is fraught with difficulties. However, if the follicular cells with round/ovoid nuclei, small to prominent eccentrically located nucleoli, nuclear overlapping and chromatin clearing are present in a background of abundant colloid, it might be prudent to briefly consider MFVPTC in the differential diagnosis or render a diagnosis of at least AUS instead of a benign colloid nodule so that appropriate patient management may be done. Likewise, updating our colleagues about this rare variant and informing them of the sampling limitation, diagnostic difficulty and pitfalls on cytology may help them understand the reason behind an occasional false negative diagnosis on cytology. MFVPTC has been described as an indolent disease with a good prognosis and moderate risk of metastasis. However, rare lung and bone metastasis as well as death have been reported.[11]


COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interest.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
As this is a case report without identifiers, our institution does not require approval from the Institutional Review Board or its equivalent.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2013/10/1/16/117352
REFERENCES
- Fine-needle aspiration of the macrofollicular and microfollicular subtypes of the follicular variant of papillary carcinoma of the thyroid. Cancer. 1998;84:235-44.
- [Google Scholar]
- Macrofollicular variant of papillary thyroid carcinoma diagnosed by fine needle aspiration biopsy: A case report. Acta Cytol. 1998;42:1184-8.
- [Google Scholar]
- Macrofollicular variant of papillary thyroid carcinoma. Report of a case with fine needle aspiration biopsy findings. Acta Cytol. 1998;42:1441-3.
- [Google Scholar]
- Fine needle aspiration cytology of macrofollicular variant of thyroid papillary carcinoma in a male. Acta Cytol. 2001;45:483-6.
- [Google Scholar]
- Macrofollicular encapsulated variant of papillary thyroid carcinoma as a potential pitfall in histologic and cytologic diagnosis. A report of three cases. Acta Cytol. 2002;46:555-9.
- [Google Scholar]
- Macrofollicular variant of papillary carcinoma of the thyroid: A histologic, cytologic, and immunohistochemical study of 3 cases and review of the literature. Arch Pathol Lab Med. 2004;128:54-8.
- [Google Scholar]
- Macrofollicular variant of papillary carcinoma: A potential thyroid FNA pitfall. Diagn Cytopathol. 2007;35:560-4.
- [Google Scholar]
- Macrofollicular variant of follicular thyroid carcinoma: A clinical, cytologic, morphologic, and image analysis study of a unique case. Ann Diagn Pathol. 2009;13:101-5.
- [Google Scholar]
- The macrofollicular variant of papillary thyroid carcinoma: A study of 17 cases. Hum Pathol. 1991;22:1195-205.
- [Google Scholar]
- Macrofollicular Variant of papillary thyroid carcinoma: A Case and Control Analysis. Endocr Pathol. 1996;7:303-8.
- [Google Scholar]
- Two patients with highly aggressive macrofollicular variant of papillary thyroid carcinoma. Thyroid. 2009;19:413-6.
- [Google Scholar]








