Translate this page into:
Metastatic colorectal adenocarcinoma in cervicovaginal cytology specimens confirmed by immunocytochemical stains on liquid base specimens: Two study cases with review of the literature
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Only a few cases of adenocarcinoma (ACA) metastatic to the female lower genital tract diagnosed on cervicovaginal Pap smear have been reported during the past several decades. Both conventional and liquid based cytology (LBC) have limited sensitivity and specificity in diagnosing metastatic disease and immunocytochemical (ICC) staining may be needed for confirming the diagnosis. We present two cases of metastatic colorectal ACA diagnosed on cervicovaginal ThinPrep (TP) Pap smears, with one confirmed by ICC staining method. Recognition of extra-uterine malignancy in the cervicovaginal cytology specimen is critical for the disease diagnosis, prognosis, and the treatment. ICC staining performed on the residual LBC specimen is an important methodology to confirm the diagnosis.
Keywords
Colon cancer
immunocytochemistry
pap smear
INTRODUCTION
Metastatic adenocarcinoma (ACA) to the cervicovaginal region is rare. Only few cases of ACA metastatic to the female lower genital tract diagnosed on cervicovaginal Pap smear have been reported during the past several decades. The youngest reported patient was 17 years old.[1] The primary sites of metastatic tumors are stomach, colon, rectum, breast, and skin melanoma, with ACA of the gastrointestinal tract forming the bulk of the metastasis to the uterine cervix from the extra-genital site.[23] These patients carry a dismal prognosis.[4] The routine gynecological clinical examination can be the first step in identifying the metastatic malignancy. Both conventional and liquid based cytology (LBC) have limited sensitivity and specificity in diagnosing metastatic disease. Thus, immunocytochemical (ICC) staining may be needed for confirming the diagnosis.
We have previously reported the utilization of ICC in the differential diagnosis of high-grade squamous intraepithelial lesion and in confirming the interpretation of cervical small cell carcinoma (SMCC) in the LBC ThinPrep (TP) cervicovaginal cytology specimens.[56] Here, we present two cases of metastatic colorectal ACA on LBC TP specimens, with confirmation by ICC.
CASE REPORT
Recently, two Pap smears were interpreted as positive for malignant cells in LBC TP smears, consistent with ACA, possibly metastatic.
Clinical history
The first patient was an 82-year-old female with a history of hysterectomy and colon cancer, status postpartial colon resection who presented with vaginal bleeding. The second patient was a 56-year-old female with a history of invasive ACA of the rectosigmoid colon, status-post segmental resection who presented for routine examination.
Pathological findings
The LBC of vaginal specimens from both patients were received in PreservCyt fixative, processed by TP 2000 automated processor (Hologic Inc., Bedford, MA) and stained by modified Papanicolaou stain.
In the first case, the TP Pap smear preparation was moderately cellular and showed clusters and groups of columnar-shaped tumor cells with enlarged ovoid nuclei, an increased nuclear-to-cytoplasmic ratio, marked nuclear pleomorphism, hyperchromasia, and nucleoli in some of the cells. Mixed inflammatory cells and squamous cells were present in the background [Figure 1]. In the second case, the TP Pap smear showed tumor cells present in syncytial fragments of tumor cells with enlarged ovoid nuclei, increased nuclear to cytoplasmic ratio, nuclear pleomorphism, hyperchromasia, and prominent nucleoli [Figure 2].
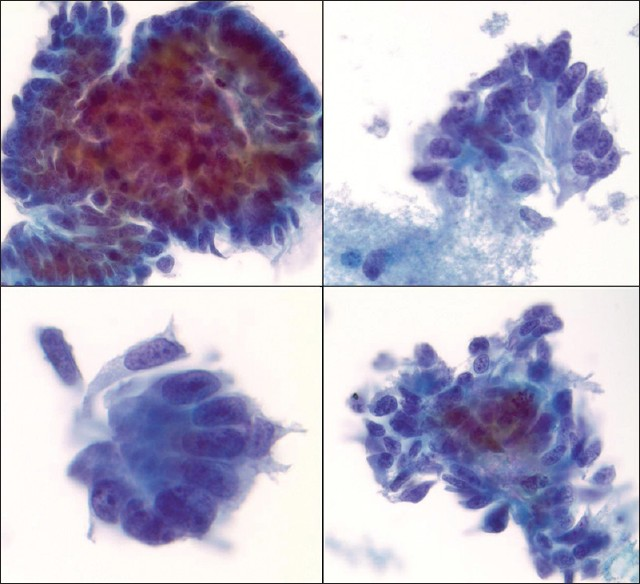
- ThinPrep Pap smear, case 1 (Papanicolaou stain, ×60). Groups of columnar shaped cells showing cytomorphological features of malignancy including increased nuclear to cytoplasmic ratio, nuclear pleomorphism, hyperchromasia, and prominent nucleoli

- ThinPrep Pap smear, case 2 (Papanicolaou stain, ×60). Syncytial fragments of cells showing cytomorphological features of malignancy including increased nuclear to cytoplasmic ratio, nuclear pleomorphism, hyperchromasia, and prominent nucleoli
ICC staining
For the first case, further evaluation with ICC was not possible for confirmation of the primary tumor due to the lack of sufficient material. In the second case, the residual LBC specimen was utilized to prepare additional TP slides for ICC. The ICC stains for cytokeratin 7 (CK7), CK20, and caudal-related homeobox 2 (CDX2) were performed on the Ventana Bench Mark Automated stainer utilizing commercial pre-diluted antibodies and protocol previously described.[56] ICC stain was considered positive when more than 5% of the tumor cells showed immunostaining. For the second case, ICC showed immunoreactivity in the tumor cells for cytoplasmic CK20 and nuclear CDX2, while the tumor cells were non-immunoreactive for CK7 [Figure 3].
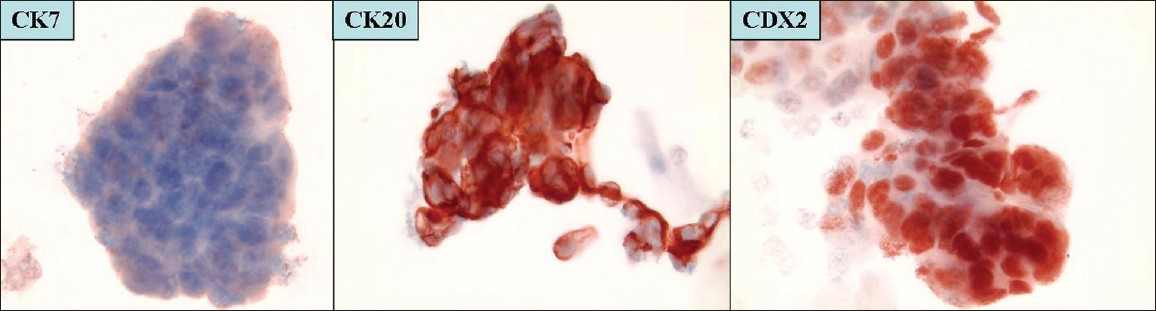
- Immunocytochemical results, case 2. cytokeratin 7−, cytokeratin 20+ and caudal-related homeobox 2+ immunostaining pattern (×20)
Concurrent vaginal biopsy results were used for confirmation in both cases. The vaginal biopsies showed metastatic colorectal carcinoma infiltrating the vaginal tissue [Figure 4]. The immunohistochemical stains performed on the vaginal biopsies supported the diagnosis of metastatic ACA of colorectal origin consistent with the clinical history of colon carcinoma. The material from the primary colorectal carcinoma from case 1 was available for review and showed morphology similar to that seen in the vaginal biopsy.
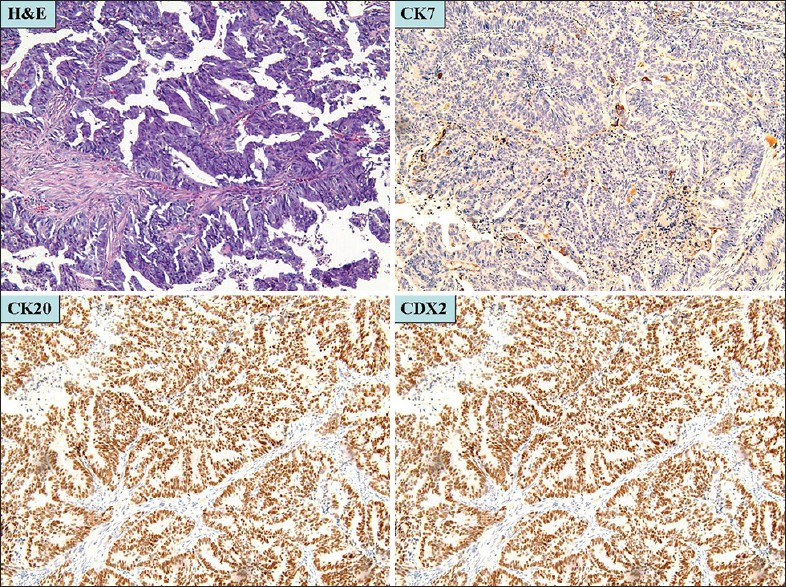
- Vaginal biopsy, case 1 (H and E, ×10), Malignant glands infiltrating the vaginal stroma. cytokeratin 7−, cytokeratin 20+ and caudal-related homeobox 2+ immunohistochemical staining pattern (×10)
DISCUSSION
Metastasis to the cervicovaginal region is relatively uncommon. The majority of metastatic cells in Pap smears arise from the uterine cervix, followed by endometrium, vulva, and ovary. Other sites include breast, gastrointestinal tract, and rarely other sites.[234] Recognition of the extra-uterine malignancy in the cervicovaginal cytology specimen is critical for the disease diagnosis, prognosis, and treatment. Abnormal findings on the routine gynecological clinical examination can be the first step to lead to the discovery of a metastatic lesion.
The cytomorphological features in these two cases that are consistent with a colonic primary include syncytial tissue fragments and clusters of columnar cells with atypical features including high nuclear to cytoplasmic ratio and prominent nucleoli with cellular debris in the background.
The differential interpretations include a malignancy of gynecological tract origin such as endometrial or endocervical carcinoma. Although the cytomorphological features and history are most consistent with the diagnosis of a gastrointestinal primary, an endocervical or endometrial primary is a distinct possibility that needs to be further evaluated.
The cytomorphological features of endocervical and endometrial ACA seen in the LBC TP cervicovaginal cytology specimens are well-established.[7] However, because of overlapping features, sometimes seen with gastrointestinal ACA, including columnar cells, mucinous cytoplasm, and necrotic background, cytomorphology may be insufficient for confirmation of the metastatic origin.
CK7 and CK20 immunoexpresssion is commonly used in combination to evaluate coordinate immunoreactivity pattern in tumor cells to confirm the origin of metastatic disease with unknown primary sites. CK7 immunoreactivity is observed in tumors of lung, breast, upper gastrointestinal and pancreatobiliary tract, endometrium, vagina, and ovary, while tumors of colonic origin are generally non-reactive to this immunomarker. CK20 immunoexpression is detected in tumors of gastrointestinal tract and urothelium.[8] CDX2 immunoexpression has recently been shown to be useful in establishing gastrointestinal origin in metastatic tumors and has become a useful addition to the standard immunohistochemistry panel for carcinomas of unknown primary sites.[9]
In routine clinical practice, a panel of immunostains with expression pattern of CK7−/CK20+/CDX2+ is used to confirm colonic primary origin. However, CDX2 immunoexpression may be seen in genitourinary tract cancers with mucinous and intestinal-type differentiation and recently has also been noted in 73% of endometrioid carcinomas with squamous differentiation and in squamous morules.[10] Therefore, comparison with the primary tumor morphology may be of pivotal importance in confirming the diagnosis of a metastatic disease as was carried out in these cases.
Some additional benefits of cervical cytology with LBC include utilization of the residual LBC specimen for ancillary studies including ICC and molecular analysis.[111213141516] In cervicovaginal LBC specimens, the residual material is widely used for HPV (Human papillomavirus) DNA (Deoxyribonucleic acid) detection by molecular methods. However, review of the literature shows that the remaining cellular material in fluid fixative can also be used for ICC such as p16INK4 and other HPV-related surrogate marker expression.[1415161718]
Application of ancillary studies is also becoming more and more useful for non-gynecological LBC specimens, including those of thyroid and breast.[1112] We have previously reported that ICC performed on additionally prepared TP slides is helpful in differentiating histiocytic aggregates from high grade squamous intraepithelial lesions as well in confirming the diagnosis of primary cervical SMCC.[56]
In a recent report by Tanaka et al., ICC was used for confirming the diagnosis of metastatic colon cancer in a vaginal stump using a panel of immunostains including CKAE1/AE3, CK7, CK20, CEA (Carcinoembryonic antigen), and vimentin.[4] We agree with their opinion that in metastatic cancers to the cervicovaginal region with characteristic ICC findings such as colorectal carcinoma, biopsy may not be needed for confirming the diagnosis as it may be associated with excessive bleeding.[4] However, a more inclusive panel of immunohistochemical markers including CK7, CK20, and CDX2 showing characteristic CK7−/CK20+/CDX2+ pattern of immunohistochemical expression is needed for confirmation.
Due to a chance of overlapping immunoreactivity pattern with non-gastrointestinal primary tumors with intestinal/mucinous differentiation, one should use ICC judiciously in concert with cytomorphological features and appropriate clinical history. This study clearly illustrates the utility of ICC in confirming the diagnosis of metastatic disease in liquid-based cervicovaginal cytology specimens.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The author(s) declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from Institutional Review Board (IRB) (or its equivalent).
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind mode (authors are blinded for reviewers and vice versa) through automatic online system
ACKNOWLEDGMENTS
This study was presented in part as poster at the Michigan Society of Pathologists 2011 Winter Conference and Meeting, Plymouth, MI.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2013/10/1/9/112297
REFERENCES
- Adenocarcinoma of the cervix metastatic from a colon primary and diagnosed from a routine pap smear in a 17-year-old woman: A case report. J Reprod Med. 2005;50:793-5.
- [Google Scholar]
- Cytomorphological features of metastatic mammary lobular carcinoma in cervicovaginal smears: Report of a case and review of literature. Cytopathology. 2005;16:42-8.
- [Google Scholar]
- Cytomorphological features of extra-genital metastases in SurePath™ cervical liquid-based cytology: A series of eight cases. Cytopathology. 2013;24:123-8.
- [Google Scholar]
- Utility of histiocytic immunomarkers in differentiating histiocytic aggregates with marked nuclear atypia from high grade squamous intraepithelial lesions in liquid-based cervicovaginal cytology specimens. Acta Cytol. 2009;53:479-81.
- [Google Scholar]
- Small cell carcinoma of the cervix in liquid-based Pap test: Utilization of split-sample immunocytochemical and molecular analysis. Diagn Cytopathol. 2012;40:214-9.
- [Google Scholar]
- Gyn cytology. In: Demay RM, ed. The Art and Science of Cytopathology Vol 1. (2nd ed). Hong Kong: ASCP Press; 2012. p. :105.
- [Google Scholar]
- Use of cytokeratins 7 and 20 in determining the origin of metastatic carcinoma of unknown primary, with special emphasis on lung cancer. Eur J Cancer Prev. 2001;10:77-82.
- [Google Scholar]
- CDX-2, a new marker for adenocarcinoma of gastrointestinal origin. Adv Anat Pathol. 2004;11:101-5.
- [Google Scholar]
- CDX2 as a marker for intestinal differentiation: Its utility and limitations. World J Gastrointest Surg. 2011;3:159-66.
- [Google Scholar]
- Estrogen and progesterone receptor contents in ThinPrep-processed fine-needle aspirates of breast. Am J Clin Pathol. 1999;112:50-6.
- [Google Scholar]
- Diagnostic efficacy of immunocytochemistry on fine needle aspiration biopsies processed by thin-layer cytology. Acta Cytol. 2006;50:129-35.
- [Google Scholar]
- P16INK4A as an adjunct test in liquid-based cytology. Anal Quant Cytol Histol. 2003;25:8-11.
- [Google Scholar]
- Overexpression of p16INK4A in liquid-based specimens (SurePath) as marker of cervical dysplasia and neoplasia. Diagn Cytopathol. 2002;27:365-70.
- [Google Scholar]
- Comparison of p16INK4A and Hybrid Capture 2 human papillomavirus testing as adjunctive tests in liquid-based gynecologic SurePath preparations. Diagn Cytopathol. 2008;36:142-8.
- [Google Scholar]
- p16 immunocytochemistry on cell blocks as an adjunct to cervical cytology: Potential reflex testing on specially prepared cell blocks from residual liquid-based cytology specimens. Cytojournal. 2011;8:1.
- [Google Scholar]
- p16INK4a immunostaing of liquid based cervical cytology smears with surepath® - Comparison of two antibodies. Mod Pathol. 2005;18:1A-359A. (Abstract #305)
- [Google Scholar]
- Application of p16INK4A immunostaing for definitive interpretation of ASC-H in liquid based cervical cytology smears with surepath®. Mod Pathol. 2005;18:1A-359A. (Abstract #306)
- [Google Scholar]








