Translate this page into:
Not all neck mass fine-needle aspirations with squamous cells are squamous cell carcinoma; report of a case of recurrent thyroid carcinoma with papillary and squamous components
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a case of a 65-year-old female who had a total thyroidectomy 12 years ago for papillary thyroid carcinoma (PTC) who presented with a recurrent thyroid bed mass. Fine-needle aspiration biopsy yielded malignant cells, consistent with squamous cell carcinoma (SCCa). Surgical resection was performed, and histologic evaluation of the mass showed mixed PTC and SCCa. The tumor cells were positive for BRAF V600E mutation. Thyroid carcinomas with admixed papillary carcinoma and SCCa are rare and are associated with aggressive behavior, high rates of metastasis, and poor outcomes. Although SCCa presenting as a neck mass is relatively common, clinical history and appropriate workup are essential for accurate diagnosis and determination of origin.
Keywords
Fine-needle aspiration
neck mass
papillary thyroid carcinoma
squamous cell carcinoma
INTRODUCTION
Squamous cell carcinoma is a common malignancy diagnosed in fine needle aspiration biopsies of neck masses. However, it is important to keep in mind that some primary tumors of other histologies may also show squamous differentiation. Here, we describe such a case of a woman with metastatic papillary thyroid carcinoma with squamous differentiation.
CASE REPORT
A 65-year-old female with a history of complete thyroidectomy 12 years ago for “some kinds of cancer” (later confirmed to be papillary thyroid carcinoma [PTC]) presented with a new neck mass in the left thyroid bed. On physical examination, the neck mass appeared fluctuant on the left side of the neck with overlying erythematous changes extending from the mass down to the upper chest just below the sternal notch. A fine-needle aspiration (FNA) was performed. The Diff-Quik-stained smears showed singly dispersed and clusters of epithelioid cells with dark chromatin and abundant cytoplasm [Figure 1a and b]. A Papanicolaou-stained smear showed epithelioid cells with dense and focally orangeophilic cytoplasm [Figure 2]. A cell block showed brightly eosinophilic cells with squamoid features [Figure 3]. Immunohistochemical stains were performed and showed the cells were immunoreactive for p63 and cytokeratin 5/6 and negative for thyroid transcription factor-1 (TTF-1) and thyroglobulin [Figure 4a–d]. The preoperative interpretation of the FNA at that time was “positive for malignant cells consistent with squamous cell carcinoma (SCCa).”
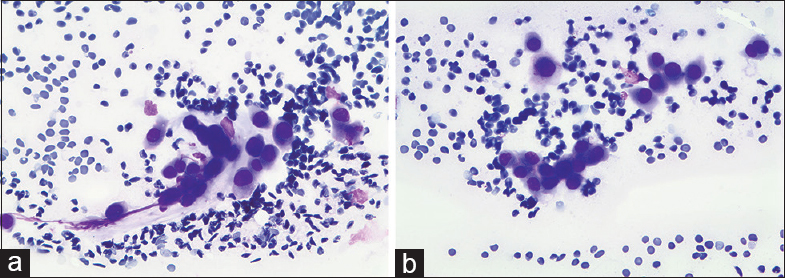
- (a) Diff-Quik stained smears showing clusters of epithelioid cells with hyperchromatic nuclei. (b) Diff-Quik stained smears showing similar-appearing singly dispersed epithelioid cells with hyperchromatic and irregular nuclei
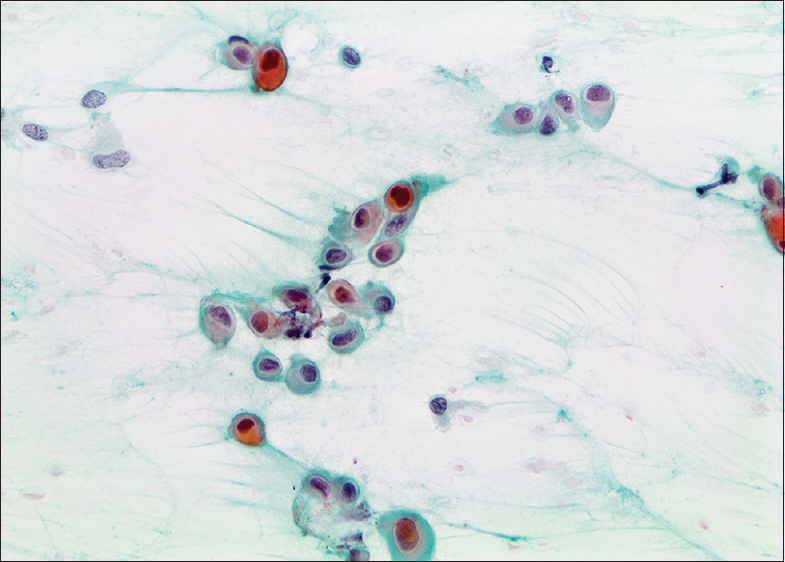
- Papanicolaou-stained smears showing atypical epithelioid cells with abundant dense cytoplasm and orangeophilia
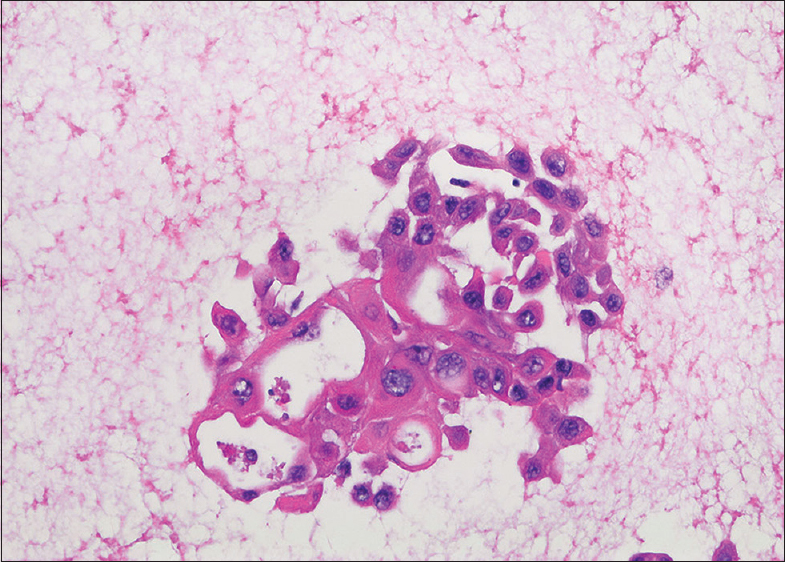
- Cell block showing cohesive cells with squamous features and atypical nuclei
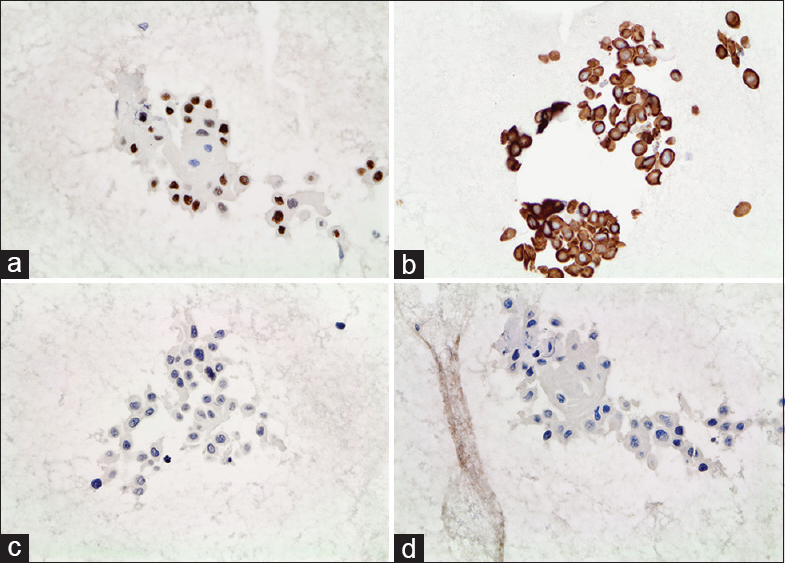
- (a) Cell block showing tumor cells with positive immunostaining for p63. (b) Cell block showing tumor cells with positive immunostaining for cytokeratin 5/6. (c) Cell block showing tumor cells with negative immunostaining for thyroid transcription factor-1. (d) Cell block showing tumor cells with negative immunostaining for thyroglobuin
The patient underwent surgical resection of the neck mass, but a complete resection could not be performed due to the proximity to major mediastinal structures. Histologic sections of the neck mass revealed admixed PTC and SCCa with cystic degeneration. The PTC areas of the tumor showed papillary structures with fibrovascular cores [Figure 5a–e] and cells with nuclear enlargement, overlapping, grooves, and pale chromatin. The PTC areas were intimately admixed with SCCa. The SCCa areas showed islands and nests of eosinophilic cells with squamous differentiation and focal keratinization [Figure 6a and b]. Immunohistochemical stains were performed and showed the PTC was negative for p63 and cytokeratin 5/6 and immunoreactive for TTF-1 and thyroglobulin [Figure 7a–d]. The SCCa component stained the exact opposite; immunoreactive for p63 and cytokeratin 5/6 and negative for TTF-1 and thyroglobulin [Figure 8a–d]. The tumor was found to be positive for BRAF V600E by immunohistochemical analysis (clone VE1, Ventana) in the SCCa component.
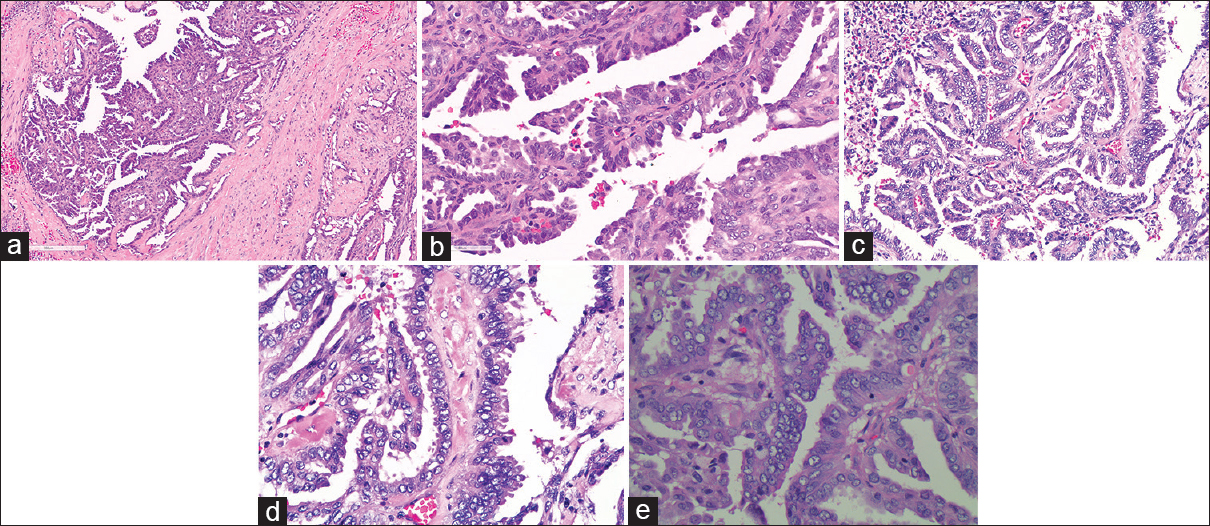
- (a) Low power H and E of resection specimen showing a tumor with papillary architecture in a dense fibrous stroma. (b) High-power H and E of resection specimen highlighting papillary architecture with fibrovascular cores. (c) H and E of resection specimen showing papillary tumor with enlarged overlapping nuclei and cleared chromatin. (d) High power H and E of resection specimen highlighting nuclear features of papillary thyroid carcinoma including overlapping nuclei, cleared chromatin, and focal nuclear grooves. (e) High power H and E of resection specimen showing nuclear and histologic features of classic variant of papillary thyroid carcinoma
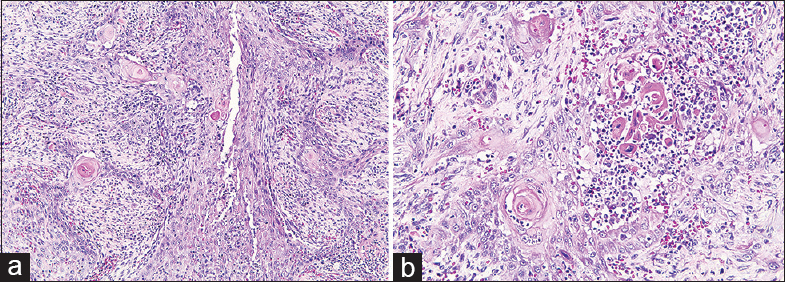
- (a) Low power H and E of resection specimen showing component of tumor with squamous features including infiltrating tumor cells in sheets with keratin pearls. (b) High power H and E of resection specimen showing tumor with squamous features including sheet-like architecture, abundant eosinophilic cytoplasm, keratin pearls, and dyskeratotic cells
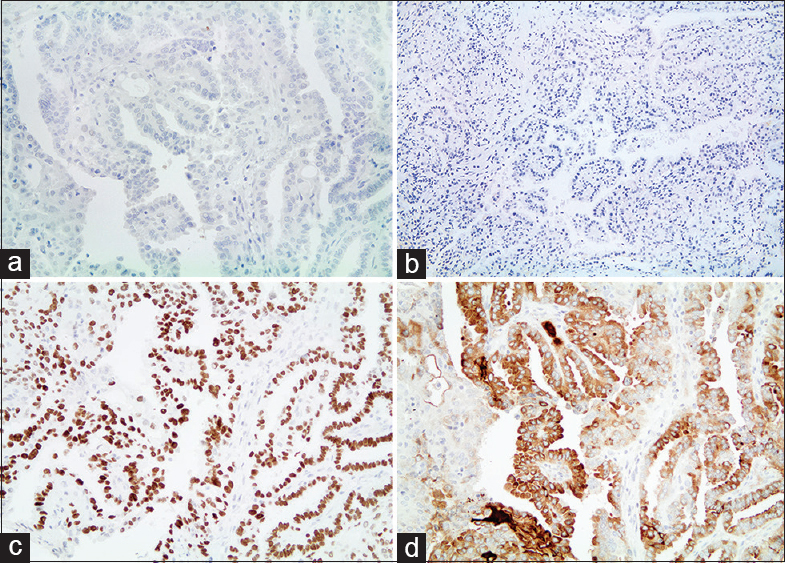
- (a) Papillary thyroid carcinoma component with negative immunostaining for p63. (b) Papillary thyroid carcinoma component with negative immunostaining for cytokeratin 5/6. (c) Papillary thyroid carcinoma component with positive immunostaining for thyroid transcription factor-1. (d) Papillary thyroid carcinoma component with positive immunostaining for thyroglobulin
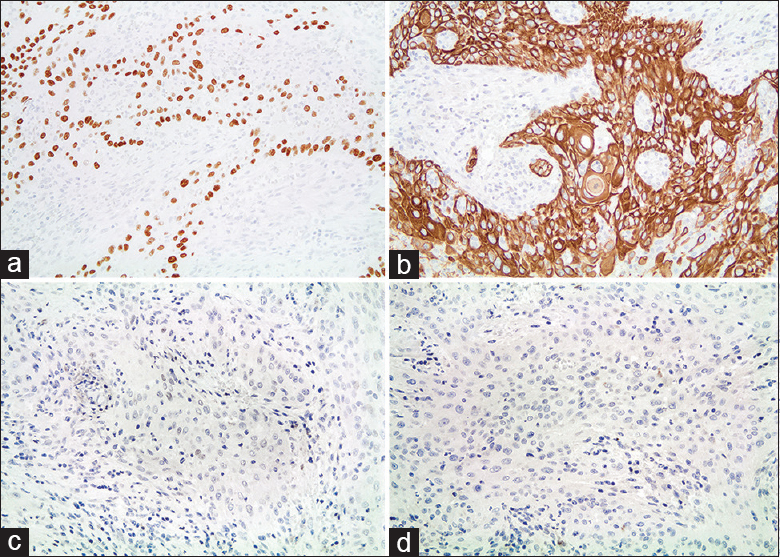
- (a) Squamous cell carcinoma component with positive immunostaining for p63. (b) Squamous cell carcinoma component with positive immunostaining for cytokeratin 5/6. (c) Squamous cell carcinoma component with negative immunostaining for thyroid transcription factor-1. (d) Squamous cell carcinoma component with negative immunostaining for thyroglobulin
Postoperatively, the patient was treated with combined chemoradiation (carboplatin and taxol), targeting the SCCa component, and radioactive iodine was used for the PTC component. Both courses were completed without severe side effects. Two months later at a follow-up appointment, the patient presented with a new, nontender left clavicle lesion and hypercalcemia. Positron emission tomography (PET) demonstrated increased activity in the left clavicle and also in a large left lower lobe pulmonary mass. Stereotactic body radiation therapy was used to treat the lesions in her lung and clavicle. After treatment, computed tomography and PET scans of the lung showed an almost complete resolution of the lung lesion but a persistent mass and metabolic uptake within the clavicular lesion. The clavicular lesion was resected and showed recurrent SCCa with a positive bone margin and infiltration of bone marrow. Magnetic resonance imaging (MRI) was performed and showed diffuse bone marrow involvement. In addition, an MRI of the head found multiple metastatic lesions in the brain. She was discharged to hospice care.
DISCUSSION
SCCa of the thyroid is rare and occurs in three different settings: (1) primary SCCa defined as carcinoma composed entirely of tumor cells with squamous differentiation, (2) secondary involvement by direct extension from an adjacent structure or metastasis from a distant SCCa,[1] and (3) as a component of an anaplastic or undifferentiated thyroid carcinoma often mixed with areas of well-differentiated PTC or follicular carcinoma.[2] Primary SCCa of the thyroid is extremely rare, accounting for <1% of all primary thyroid cancers.[3] These tumors present as sudden enlargement of a neck mass with associated compression symptoms, similar to the presentation of anaplastic thyroid carcinoma. The median survival of these tumors is <1 year. Secondary involvement by direct extension or metastasis can be reasonably excluded by clinical history and/or panendoscopy. The third scenario, thyroid carcinoma with both papillary and squamous features, is also rare and represents 2% of all thyroid carcinomas.[4] Ito et al reports ten cases of PTC with SCCa components.[5] Some authors report that these combination tumors often mimic the aggressive clinical course and prognosis of anaplastic carcinoma,[4] whereas others report better survival. Although the clinical presentation and prognosis may be similar in some cases, histologic features are different.[36] Occasionally, anaplastic carcinomas do show focal squamoid differentiation histologically; however, unlike the current case, these tumors tend to be nonkeratinizing and poorly differentiated with more frank pleomorphism and other more conventional anaplastic features such as spindle cell and giant cell components. The current case did not show anaplastic features morphologically. Many cases of SCCa of the thyroid have been reported in association with the tall cell variant of papillary carcinoma (TCV). TCV is often larger than classic PTC, typically occurs in older patients, and is found to have a more aggressive course.[2] Previous studies of the association between TCV and SCCa of the thyroid suggest that there may be a histopathologic link in the development of thyroid carcinogenesis.[7] In this case, the PTC component was considered the classic variant, as it did not meet diagnostic criteria for TCV (tumor cell height 3 times the width in >50% of tumor cells).
Unique to our case is that the combination of PTC and SCCa presented as a neck mass many years after the thyroid was removed for conventional PTC. Cervical metastasis with combined PTC-SCCa in a patient with a remote history of thyroidectomy due to conventional PTC has only been reported a few times.[37] Although some postulate the squamous cells in the tumor may derive from embryonic remnants, the more commonly accepted origin is squamous metaplasia of the thyroid tumor cells.[78]
This case highlights that although SCCa is a common tumor encountered in FNA biopsies of neck masses, it is prudent to remember that primary thyroid carcinomas may also contain components of SCCa in rare cases, and clinical history, imaging, and immunostains should be utilized to arrive at an accurate diagnosis.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE. Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
AH and MO performed the literature review and drafted the manuscript, and MO performed the diagnosis, contributed to the draft manuscript, and provided microscopic images. KD contributed to the draft manuscript, revised, and edited it critically for publication purposes and prepared it for submission. Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
As this is a case report without identifiers, our institution does not require approval from the Institutional Review Board.
LIST OF ABBREVIATIONS (In alphabetic order)
FNA - Fine-needle aspiration
MRI - Magnetic resonance imaging.
PET - Positron emission tomography
PTC - Papillary thyroid carcinoma
SBRT - Stereotactic body radiation therapy
SCCa - Squamous cell carcinoma
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Squamous cell carcinoma of the thyroid gland: Primary or secondary disease? J Laryngol Otol. 2011;125:3-9.
- [Google Scholar]
- Squamous cell carcinoma of the thyroid: An aggressive tumor associated with tall cell variant of papillary thyroid carcinoma. Mod Pathol. 2000;13:742-6.
- [Google Scholar]
- Papillary thyroid carcinoma recurring as squamous cell carcinoma 10 years after total thyroidectomy: Lessons from rapidly progressive papillary thyroid carcinoma. Intern Med. 2013;52:1593-7.
- [Google Scholar]
- Thyroid carcinoma with papillary and squamous features: Report of a case with histogenetic considerations. Pathol Res Pract. 2010;206:263-9.
- [Google Scholar]
- Biological behavior of papillary carcinoma of the thyroid including squamous cell carcinoma components and prognosis of patients who underwent locally curative surgery. J Thyroid Res. 2012;2012:230283.
- [Google Scholar]
- Thyroid papillary carcinoma recurring as squamous cell carcinoma: Report of a case. Surg Today. 2006;36:171-4.
- [Google Scholar]
- Spindle cell squamous carcinoma of the thyroid: An unusual anaplastic tumor associated with tall cell papillary cancer. Mod Pathol. 1991;4:637-43.
- [Google Scholar]
- Intrathyroidal epithelial thymoma: An entity distinct from squamous cell carcinoma of the thyroid. World J Surg. 1985;9:128-35.
- [Google Scholar]








