Translate this page into:
Pancreatic tuberculosis – A common disease at a rare site diagnosed on cytology

*Corresponding author: Debasis Gochhait, Department of Pathology, JIPMER, Puducherry, India. debasis.go@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thambiraj P, Gudivada V, Gochhait D, Siddaraju N, Pottakat B. Pancreatic tuberculosis – A common disease at a rare site diagnosed on cytology. CytoJournal 2024;21:1. doi: 10.25259/Cytojournal_33_2023
Dear Editor,
Tuberculosis (TB) is a significant health problem in developing countries like India. Abdominal involvement in TB is seen only in 12% of systemic TB, with the most common sites being mesentery, small bowel, peritoneum, liver, and spleen. Involvement of the pancreas is extremely rare, accounting for 5% of extra-pulmonary cases, possibly due to the enzymatic milieu, which has inherent biologic activity against tubercle bacilli.[1,2] Although reports of isolated pancreatic TB[3] have been claimed, there is always a possibility that one could have missed the evidence of the prior occurrence of the disease elsewhere. Chronic pancreatitis with inflammatory head mass could mimic malignancy clinicoradiologically. Here is a case of chronic calcific pancreatitis with a strong clinicoradiological suspicion of malignancy with TB.
A 47-year-old immunocompetent male patient presented with intermittent upper abdominal pain and loss of appetite for duration of 6 months along with jaundice for 2 weeks. Contrast-enhanced computed tomography (CECT) chest and abdomen [Figure 1a and b] showed an enlarged pancreatic head with multiple intraductal stones in the head, uncinate process, body, and tail of the pancreas. A few small hypodense areas were present in the head region, suggesting pseudocysts, and features were suspicious for malignancy. In suspicion of pancreatic head malignancy in the background of chronic calcific pancreatitis, pancreaticoduodenectomy was planned. Intraoperatively, dense adhesions were noted. Pancreatic parenchyma showed multiple parenchymal calcifications and abscess cavities, yielding purulent discharge [Figure 1c and d]. Intraoperative fine-needle aspiration was performed. Giemsa and Papanicolaous-stained smears showed numerous non-caseating epithelioid granulomas and Langhans giant cells in an acute and chronic inflammatory background, along with tiny fragments of normal pancreatic ductal and acinar cells [Figure 2a-c]. Ziehl–Neelsen staining shows acid-fast bacilli [Figure 2d]. Due to clinicoradiologic solid suspicion of malignancy and to provide symptomatic relief, the surgery team proceeded with pancreatoduodenectomy. Cut section through the pancreas revealed many tubercles with yellowish cheesy areas and ill-defined whitish lesions [Figure 3a]. Histological findings concurred with the fine-needle aspiration cytology (FNAC) report revealing caseating epithelioid granulomas with Langhans giant cells in the pancreas [Figure 3b and c]. Retropancreatic nodes also showed caseating granulomatous lymphadenitis [Figure 3d]. Sampling of adjacent pancreatic tissue showed changes in chronic pancreatitis. Chronic pancreatitis alters the enzymatic milieu, thereby predisposing to the secondary infection of the organ. The involvement of the pancreas may have occurred through a hematogenous route or by reactivation of previous abdominal TB foci in contiguous peripancreatic nodes. Pancreas is relatively resistant, and two postulated ways of spreading are directly from involved peripancreatic lymph nodes and, more rarely, from the hematogenous route. In this scenario, chronic pancreatitis could have led to local immunosuppression reactivating the latent tuberculous foci presenting as pancreatic head mass.
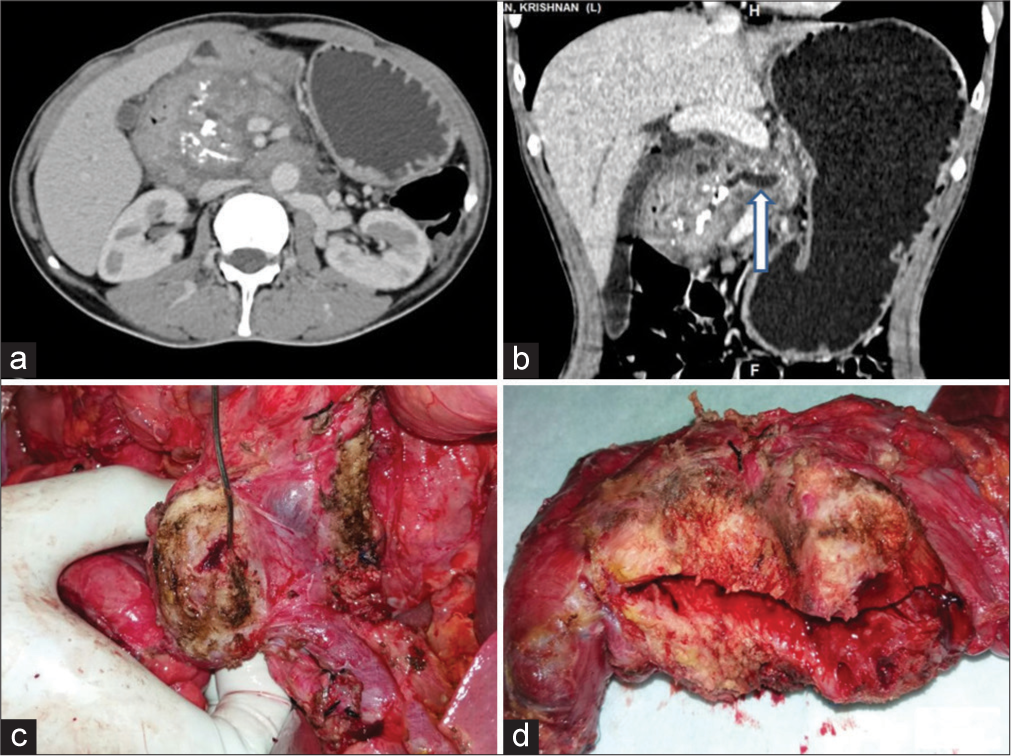
- Contrast-enhanced computed tomography images axial (a) and coronal (b) images showing infiltrative mass in the head of the pancreas, pancreatic calcifications, and main pancreatic duct (MPD) dilatation (arrow). The intraoperative pictures (c) show the pancreatic transection surface showing multiple cavitary lesions with cheesy discharge and (d) coronal section specimen showing fibrotic pancreas with multiple cavitary lesions and ectatic duct.
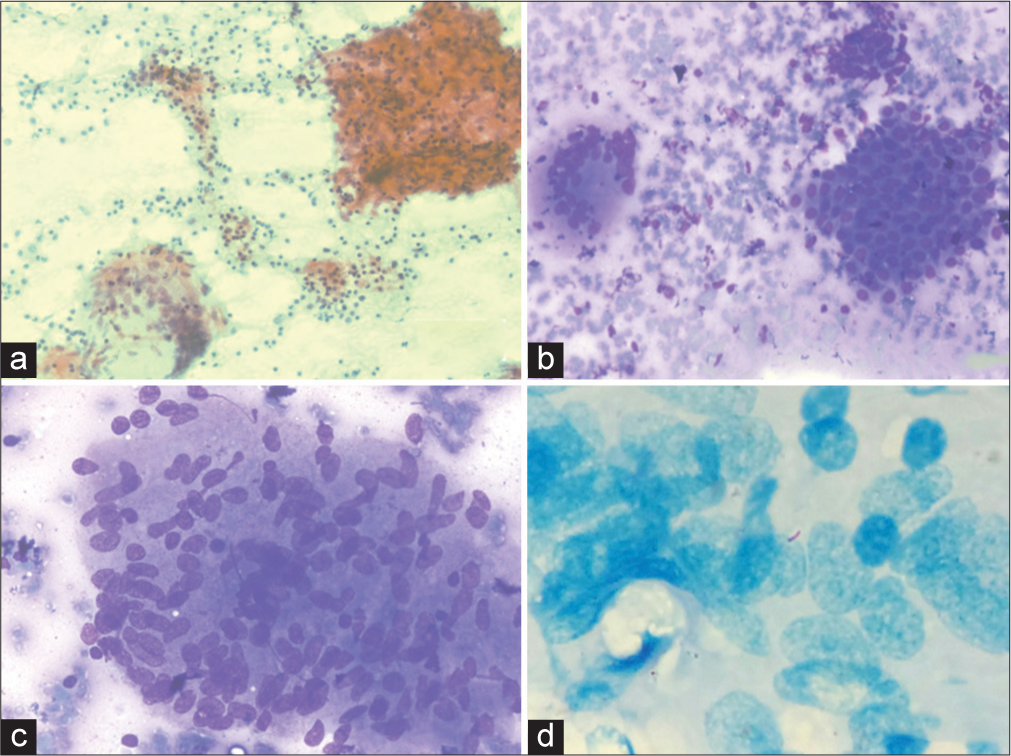
- Fine-needle aspiration cytology smear images: Low-power Papanicolaou-stained image (a) showing the granulomas and mixed inflammation in the background. (b) Low-power May-Grunwald-Giemsa (MGG)-stained image showing granuloma multinucleated giant cell and cluster of benign ductal epithelial cells. (c) High-power MGG-stained image showing multinucleated giant cells with epithelioid nuclei. (d) High-power Ziehl–Neelsen-stained image showing epithelioid cells and acid-fast bacilli.
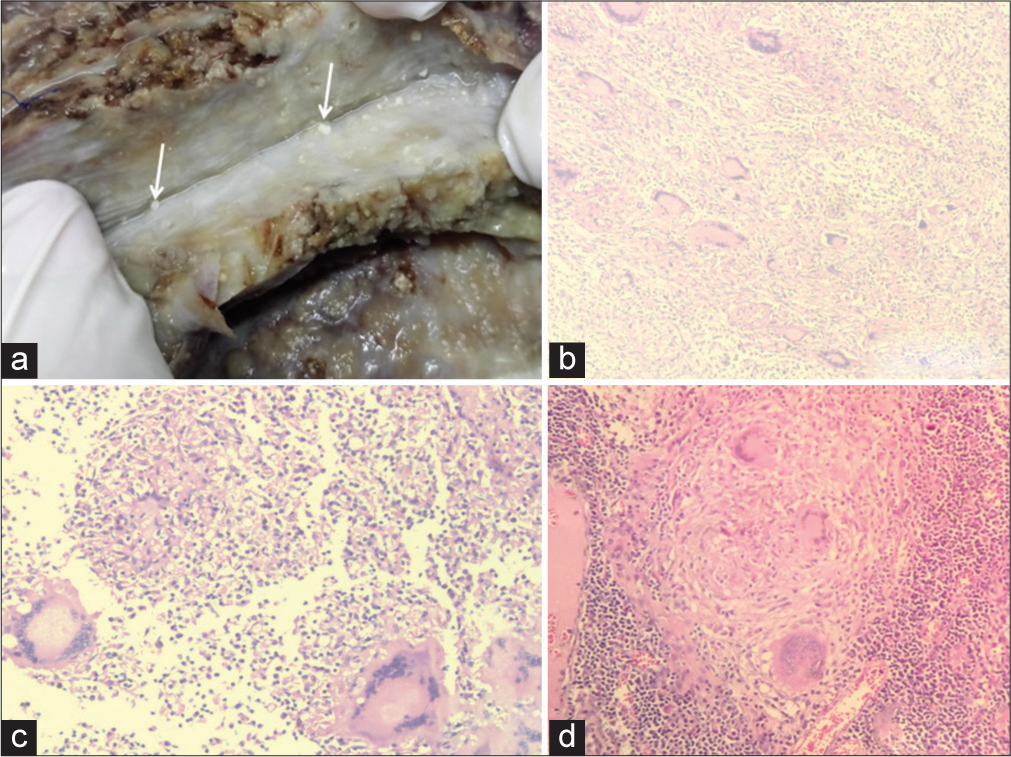
- Gross specimen and histopathology images: Gross image (a) shows the scattered tubercules in the pancreatic tissue. (b) Low-power hematoxylin and eosin (H&E)-stained image showing multiple granulomas and multinucleated giant cells. (c and d) High-power H&E-stained image showing granuloma with multinucleated giant cells.
TB may be suspected on the basis of imaging showing heterogeneous, predominantly hypodense mass lesions in the head coexistent with diffuse enlargement of the pancreas. Furthermore, necrotic peripancreatic nodes with rim enhancement suggest tubercular etiology.[3,4] However, none of the radiological features differentiate it from malignancy, and pancreatic TB remains a pathological diagnosis. Intraoperative FNAC from the head of the pancreas could confirm TB with acid-fast bacilli in the special stain. Thus, the simple and cost-effective technique of image-guided pre-operative or intraoperative FNAC is a valuable tool in establishing neoplastic and inflammatory pancreatic pathology. Secondary involvement of the pancreas by TB may occur in chronic pancreatitis, even in immunocompetent individuals of endemic areas. In these patients, a pre- or intraoperative needle aspiration and acid-fast staining can provide a definitive diagnosis for further management.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
There is no competing interest from any of the authors.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Dr. Paruvarthavardhini and Vijaylaxmi - Collection of data and preparation of the manuscript. Histopathology, Imaging, and review of the manuscript - Dr. Debasis. Review of the manuscript and cytodiagnosis - Dr Siddaraju. Management of patients - Dr. Biju. All authors have contributed to the diagnosis, management and the manuscript preparation.
ETHICS STATEMENT BY ALL AUTHORS
Consent was obtained for intraoperative FNAC and permission was obtained for publication. No identification details of the patient are disclosed.
LIST OF ABBREVIATIONS (IN ALPHABETIC ORDER)
CECT - Contrast Enhanced Computerized Tomography
TB – Tuberculosis
FNAC - Fine needle aspiration cytology
EDITORIAL/PEER REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through the automatic online system.
References
- The bacteriolytic action of gland extracts on tubercle bacilli. J Hyg (Lond). 1917;16:55-65.
- [CrossRef] [PubMed] [Google Scholar]
- The action of pancreatic juice on bacteria. J Infect Dis. 1930;46:26-30.
- [CrossRef] [Google Scholar]
- Resection versus drainage in treatment of chronic pancreatitis. Gastroenterology. 2008;134:1604-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pancreatic tuberculosis: An elusive diagnosis. HPB (Oxford). 2003;5:43-5.
- [CrossRef] [PubMed] [Google Scholar]







