Translate this page into:
Proposal for including risk of malignancy and clinical management in the Japanese system for reporting thyroid cytopathology - A multi-institutional study

*Corresponding author: Mitsuyoshi Hirokawa, Department of Diagnostic Pathology and Cytology, Kuma Hospital, Kobe, Japan. mhirokawa@kuma-h.or.jp
-
Received: ,
Accepted: ,
How to cite this article: Hirokawa M, Katoh R, Amano T, Chiba T, Yamazaki N, Satoh S, et al. Proposal for including risk of malignancy and clinical management in the Japanese system for reporting thyroid cytopathology - A multi-institutional study. CytoJournal. 2025;22:55. doi: 10.25259/Cytojournal_229_2024
Abstract
Objective:
The Japanese System for Reporting Thyroid Cytopathology (JSRTC) does not include the risks of malignancies (ROMs) or recommended clinical management. This multi-institutional study aimed to determine the frequency, re-aspiration rate, resection rate, ROM, and clinical management options in seven different categories.
Material and Methods:
For 15,495 cases of thyroid fine-needle aspiration performed at seven Japanese institutions without molecular testing, the frequency, re-aspiration rate, resection rate, ROM, and clinical management options of each diagnostic category were examined. The categorization was based on JSRTC, and cases were subdivided into those with nuclear atypia and other subtypes for undetermined significance.
Results:
Re-aspiration of unsatisfactory and undermined significance diagnostic categories was mainly performed for cases of suspected malignancy on ultrasound. The median re-aspiration rate of cyst fluid nodules was 4.9%, which was significantly different from that (17.8%) of unsatisfactory cases (P < 0.05). The resected ROMs for nodules that were suspicious for malignancy and malignant were 94.2% and 99.6%, respectively. The low resection rates of nodules that were suspicious for malignancy (77.8%) and malignant (70.8%) could be attributed to active surveillance for low-risk papillary microcarcinoma. The overall ROMs of unsatisfactory, cyst fluid, benign, undetermined significance, and follicular neoplasms were 4.5%, 0.4%, 0.7%, 16.7%, and 11.4%, respectively. In the subtype of undetermined significance, the overall ROM of nuclear atypia (27.6%) was higher than that of the others (6.7%).
Conclusion:
Overall, this study determines the frequency, ROM, and recommended clinical management for thyroid cytopathology in Japan. These results were different from those proposed by the Bethesda System for Reporting Thyroid Cytopathology. In the future, our results will be helpful in the revision of JSRTC and will contribute to improving the outcomes among Japanese patients with thyroid nodules.
Keywords
Cytodiagnosis
Cytology
Fine-needle aspiration
Risk management
Thyroid
INTRODUCTION
In 2007, the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) was developed as a reporting system for thyroid fine-needle aspiration (FNA) specimens.[1] TBSRTC comprises six diagnostic categories, each with its own risk of malignancy (ROM) and recommended clinical management options. After two revisions, based on recent data, TBSRTC’s ROM and clinical management options were updated in the third edition, introduced in 2023.[2] ROM and clinical management are crucial for improving patient outcomes in the diagnosis and treatment of thyroid nodules. They are required for early detection of malignancy, treatment-plan determination, patient communication, optimization of medical resources, and strengthening of evidence. Therefore, TBSRTC is currently used worldwide as a reporting system for FNA specimens.
In contrast, due to the differences in the frequency of tumor types, indications for surgery, medical environments, and treatment strategies in Japan compared to the Western countries, Japan employs a different reporting system.[3] At present, the Japanese System for Reporting Thyroid Cytopathology (JSRTC), proposed by the Japan Association of Endocrine Surgery and the Japanese Society of Thyroid Pathology, is officially used [4-6] and consists of the following seven diagnostic categories: Unsatisfactory, cyst fluid, benign, undetermined significance, follicular neoplasm, suspicious for malignancy, and malignant. Although cyst fluid is considered an independent category in the JSRTC, its diagnostic criteria are the same as those in TBSRTC. Due to the lack of data, ROM and clinical management have so far not been included in the JSRTC; however, as noted above, they are essential in thyroid practice. In this study, we aimed to determine clinically significant metrics, including the frequency, re-aspiration rate, resection rate, ROM, and clinical management options in each of the seven categories using multi-institutional data from Japanese institutions.
MATERIAL AND METHODS
Case collection
In total, seven Japanese institutions that employ pathologists and cytotechnologists specializing in thyroid diseases consented to participate in this study: Four thyroid-specialized hospitals, one university hospital, one cancer-specialized hospital, and one general hospital. The study was approved by the Institutional Review Board of all participating institutions. Data regarding thyroid FNA cases recorded between 2019 and 2022, comprising more than 500 cases from each institution, were collected [Table 1]. FNA was performed under ultrasound guidance in all cases by endocrinologists, endocrine surgeons, or pathologists. The follow-up period was at least 1 year, and cases with a shorter follow-up were excluded from the study. All institutions prepared Papanicolaou-stained conventional smears. Five of them also prepared liquid-based cytology specimens as needed. In total, 15,495 thyroid FNA cases were used in this study. In cases where more than one nodule was aspirated, the nodule with the highest prognostic value on the ultrasound was selected for this study.
| Institution | Period | Cases | |
|---|---|---|---|
| A Hospital | Thyroid specialization | 2022, 1-12 | 5,753 |
| B Hospital | 2022, 4-12 | 3,988 | |
| C Hospital | 2021-2022 | 1,843 | |
| D Hospital | 2020-2022 | 612 | |
| E Hospital | University hospital | 2020-2022 | 2,004 |
| F Hospital | Hospital with cancer specialization | 2019-2021 | 786 |
| G Hospital | General hospital | 2021-2022 | 509 |
| 15,495 | |||
Clinical, cytological, and pathological data
Clinical data were extracted from the electronic medical records of each institution. The re-aspiration rate was calculated based on the number of cases in which a second aspiration was performed within 3 months of the initial aspiration. Resection rates were calculated using cases performed within 1 year of the initial cytology. Cytological results were obtained from the original reports of cases diagnosed by cytotechnologists and/or cytopathologists, and the diagnostic categories were based on the JSRTC. For the diagnostic category “undetermined significance,” a review was conducted at each institution, and subcategorization (with nuclear atypia and others) was performed based on TBSRTC. Pathological results were determined by the pathologists of each institution. The ROMs were calculated for both the overall and resected cases. Low-risk neoplasms, including non-invasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP), uncertain malignant potential, and hyalinizing trabecular tumor, were not included as malignancies.
Statistical analysis
Statistical analysis was performed on adjacent diagnostic categories. The differences between each parameter showing non-normal distribution were analyzed using the Mann-Whitney U-test. The interquartile range (Q1: 25% percentile, Q3: 75% percentile) has been shown to reduce the influence of outliers. The statistical analysis was performed using Stat Flex v.6 statistical software (Artech Co. Ltd., Osaka, Japan). P < 0.05 was considered statistically significant.
RESULTS
Table 2 shows the frequency, re-aspiration rates, resection rates, and risks of malignancy by diagnostic category in the seven Japanese institutions.
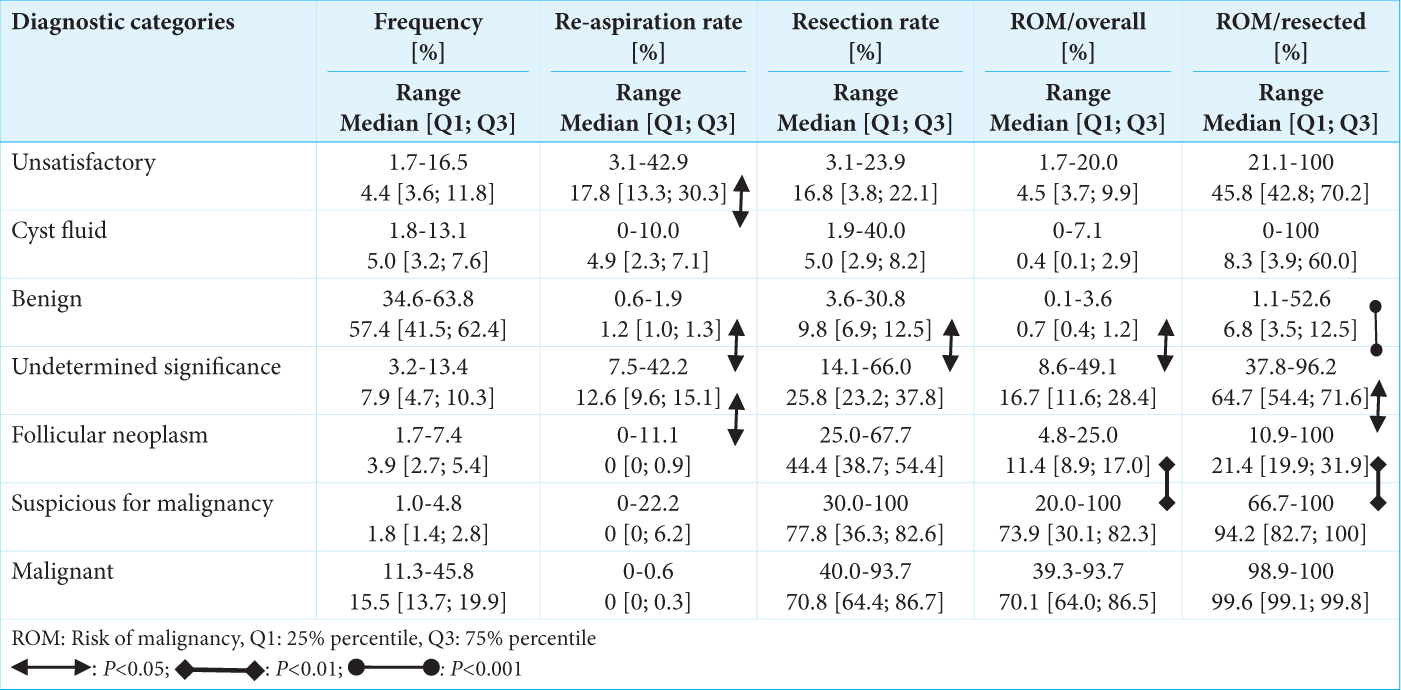 |
Unsatisfactory
The frequency ranged from 1.7% to 16.5% (median: 4.4%), with that of five institutions being <10%. In the two institutions with an incidence of >10%, liquid-based cytology was not performed, and the aspirator was unfamiliar or inexperienced with thyroid FNA. The re-aspiration rates ranged from 3.1% to 42.9% (median: 17.8%). Notably, in the institution with the lowest re-aspiration rate, re-aspiration was limited to nodules with suspected malignancy based on ultrasound examination, and both re-aspiration and ultrasound findings provided the basis for resection. The median ROMs for the overall and resected cases were 4.5% and 45.8%, respectively, and the institution with the highest overall ROM had the lowest unsatisfactory rate and highest re-aspiration rate.
Cyst fluid
The median frequency and re-aspiration rate were 5.0% and 4.9%, respectively. Re-aspiration was performed in cases suspected of malignancy based on ultrasound examination. Nodules diagnosed as malignant by re-aspiration, those with huge cystic lesions or those associated with another thyroid malignancy, were resected. The resection rate was <10% in six institutions. The median of ROMs of the overall and resected cases were 0.4% and 8.3%, respectively, and no malignant case was detected at the institution with the highest resection rate (40.0%). A significant difference was noted between unsatisfactory and cyst fluid in terms of the re-aspiration rate (P < 0.05). The resection rate and overall ROM of cyst fluid were lower than those of unsatisfactory, but no significant difference was observed.
Benign
The median frequency and re-aspiration rate were 57.4% and 1.2%, respectively. The institution with the lowest frequency (34.6%) was the one specializing in malignancy. Resection rates ranged from 3.6% to 30.8% (median, 9.8%). Notably, in six of the seven institutions, follow-up was carried out for nodules categorized as benign, and surgical resection was performed for those suspected to be malignant based on ultrasound findings. In the remaining institution, which presented the highest resection rate, resection was performed for nodules that were determined to be benign. Despite the large difference in resection rates, the difference in overall ROM was minimal (0.1-3.6%; median, 0.7%).
Undetermined significance
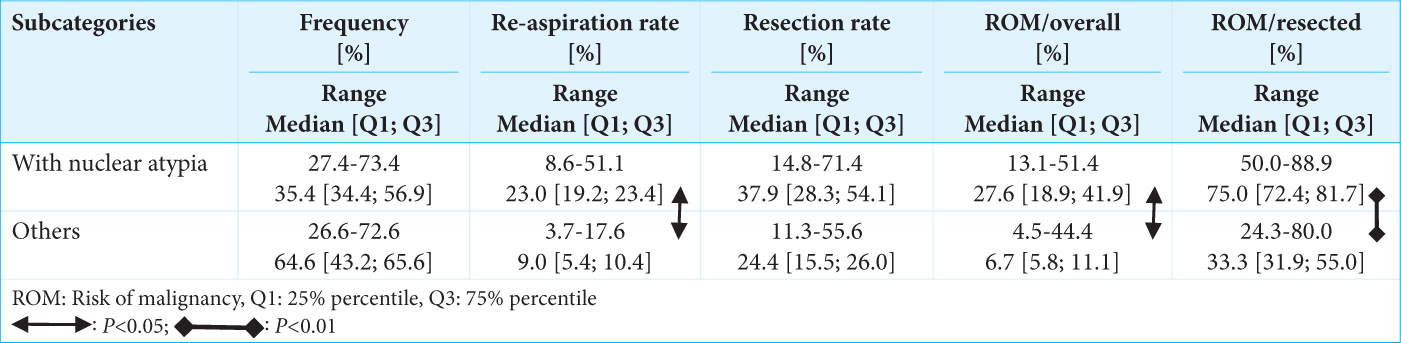
The frequencies were <8.0% (3.2-7.9%) in four institutions and >10% (10.1-13.4%) in the remaining institutions. The institutions with high frequencies presented a considerable number of unsatisfactory results, with the main cause being inappropriate specimen preparation by the aspirators due to their unfamiliarity or inexperience with thyroid FNA. Notably, no significant difference in the frequency of the subtype, namely, with nuclear atypia and others, was observed. Most nodules with nuclear atypia were suspected or possible papillary thyroid carcinoma. In contrast, nodules with subtype “others” were categorized into other types, including undeniable or possible NIFTP, parathyroid adenoma, or lymphoma. For nodules with subtype “others,” three institutions, two institutions, and one institution routinely performed immunocytochemical staining, biochemical measurement of aspirated materials, and flow cytometry as ancillary diagnostic methods, respectively. Notably, cases with suspected malignancy, as indicated by ultrasound examinations, were considered for resection. The re-aspiration rate ranged from 7.5% to 42.2% (median: 12.6%), and re-aspiration was limited to nodules with suspected malignancy on ultrasound examination in the institute with the lowest rate. The resection rate and overall ROM ranged from 14.1% to 66.0% (median: 25.8%) and 8.6% to 49.1% (median: 16.7%), respectively. Institutions with high resection rates tended to exhibit a high overall ROM. The frequency of subtype “nuclear atypia” for the following parameters was higher than that for subtype “others:” re-aspiration rates (median: 23.0% and 9.0%, respectively), resection rates (median: 37.9% and 24.4%, respectively), overall ROMs (median: 27.6% and 6.7%, respectively), and resected ROMs (median: 75.0% and 33.3%, respectively) [Table 3]. Among them, re-aspiration rates (P < 0.05), overall ROMs (P < 0.05), and resected ROMs (P < 0.01) were significantly different.
 |
Follicular neoplasm
In all institutions, the frequency of follicular neoplasm was <10%. Four of seven institutions revealed no re-aspiration cases, and the median re-aspiration rate was 0%. The resection rates ranged from 25.0% to 67.7% (median: 44.4%). Surgical resection of follicular neoplasm nodules was considered primarily based on the ultrasound findings and serum thyroglobulin levels, such as capsular invasion, size of >3.0 cm, serum thyroglobulin (1,000 ng/mL), or tumor volume-doubling rate of >1.0/year. No cases of molecular testing were observed. The median overall ROM was 11.4%, which was lower than that of the undermined significance, but no statistically significant difference was observed (P = 0.212).
Suspicious for malignancy
All institutions presented a frequency of <5%. In four institutions, the re-aspiration rate was 0%. The re-aspiration was performed mainly to confirm the diagnosis, as smears from another hospital were considered suspicious for malignancy. The resection rate ranged from 30.0% to 100% (median: 77.8%). In institutions with a low resection rate, patients with low-risk papillary microcarcinoma were followed up without resection (active surveillance). The median resected ROM was 94.2%.
Malignant
The median frequency of malignant cases was 15.5%. The institution with the highest malignancy rate (45.8%) specializes in malignancy. The resection rate ranged from 40.0% to 93.7% (median: 70.8%). In institutions with a low resection rate, active surveillance was conducted. The median resected ROM was 99.6%. Regarding the re-aspiration rate, resection rate, overall ROM, and resected ROM, the difference between suspicion for malignancy and malignant nodules was not statistically significant.
DISCUSSION
FNA is the most effective pre-operative diagnostic modality for thyroid nodules and can reduce the rate of unnecessary thyroidectomy for benign nodules. TBSRTC was first developed to facilitate communication between cytopathologists and clinicians, with different diagnostic categories having their own ROMs and management.[1] Although adopted globally as a reporting system for thyroid FNA, it is not employed in Japan due to differences in various factors between Western countries and Japan, including race, lifestyle, medical environment, surgical indication, and interpretation of pathological criteria.[3] Next-generation sequencing-based molecular testing in Japan is not performed in medical practice, and cyst fluid is handled as an adequate specimen. At present, the JSRTC is the official reporting system for thyroid FNA in Japan;[3-5] however, it does not include the ROM or clinical management for the different diagnostic categories. The reason for this is the lack of data and evidence on ROM and clinical management for each category. Based on our data, we propose the frequency, ROM, and recommended clinical management in JSRTC, as shown in Table 4. For calculating ROM, we used the percentages of overall cases for unsatisfactory, cyst fluid, benign, undetermined significance, and follicular neoplasms and that of resected cases for suspicious for malignancy and malignant. For frequency and ROM ranges, the 25th and 75th percentiles of the interquartile range were used. For the recommended clinical management, the practice followed by most of the institutions was adopted.
| Diagnostic category | Frequency [%] Median [Range] |
Risk of malignancy✶ [%] Median [Range] |
Recommended clinical management |
|---|---|---|---|
| Unsatisfactory | 4.4 [3.6-11.8] | 4.5 [3.7-9.9] | Re-aspiration or follow-up for benign ultrasound findings |
| Cyst fluid | 5.0 [3.2-7.6] | 0.4 [0.1-2.9] | Follow-up or re-aspiration for malignant ultrasound findings |
| Benign | 57.4 [41.5-62.4] | 0.7 [0.4-1.2] | |
| Undetermined significance | 7.9 [4.7-10.3] | 16.7 [11.6-28.4] | Re-aspiration, follow-up based on ultrasound findings or Ancillary study |
| Follicular neoplasm | 3.9 [2.7-5.4] | 11.4 [8.9-17.0] | Resection or follow-up based on other clinical findings |
| Suspicious for malignancy | 1.8 [1.4-2.8] | 94.2 [82.7-100] | Resection or active surveillance for low-risk papillary thyroid microcarcinoma |
| Malignant | 15.5 [13.7-19.9] | 99.6 [99.1-99.8] |
According to the JSRTC, unsatisfactory nodules should be <10% of the total number of specimens, and if this number is exceeded, the aspiration and preparation methods should be reconsidered.[4-6] In two institutions with >10% frequency of unsatisfactory nodules, liquid-based cytology was not performed. Sayer et al. reported that the adequacy rate was significantly higher for the liquid-based cytology method than for the conventional method.[7] Therefore, we recommend incorporating liquid-based cytology as a potential approach to reduce the unsatisfactory rate. Our results showed that re-aspiration is a part of routine clinical management, for unsatisfactory nodules, but follow-up can be carried out for nodules with benign ultrasound findings.
In the TBSRTC, cyst fluid-only specimens are included in the unsatisfactory category. However, in the JSRTC, they are classified as an independent category - cyst fluid - due to their low ROM (0.2-2.0%).[8,9] This study showed that the overall ROM (0.4%) of cyst fluid was considerably lower than that of unsatisfactory (4.5%) and close to that of benign (0.7%) category. No statistically significant differences were found between them, but we considered that cyst fluid-only nodules could be followed up over time in the same way as benign nodules. However, nodules with malignant ultrasound findings should be considered for re-aspiration. Thus, the management of cyst fluid-only cases could be the same as that of benign nodules and different from that of unsatisfactory nodules.
Benign was the most frequently noted category, with a frequency of 57.4% in our study. Benign nodules are usually followed up. However, since they revealed a ROM of 0.1-3.6%, re-aspiration should be performed for nodules with malignant ultrasound findings.
Undetermined significance represents specimens that cannot be differentiated as benign or malignant, do not fall into any other categories, and are difficult to diagnose. Notably, the recommended frequency is ≤10% of adequate samples in JSRTC and TBSRTC.[2,4] The results of this study were consistent with this criterion, showing a median frequency of 7.9%. The TBSRTC proposes that the atypia of undetermined significance (AUS): malignant ratio should not exceed 3.0 and recommends sub-classification of AUS with nuclear atypia and others to improve risk stratification of malignancy as the resected ROM for AUS with nuclear atypia (36-44%) is higher than that for others (15-23%). Similar findings were observed in this study (resected ROM with nuclear atypia, 75.0%; resected ROM with others, 33.3%), suggesting that differences in ROM by sub-classification were more accentuated in the overall ROM (with nuclear atypia, 27.6%; others, 6.7%). Presently, the JSRTC does not include subclassifications, but the concept should be incorporated. For the clinical management of nodules of undetermined significance, either re-aspiration or follow-up should be chosen based on the ultrasound findings. When ancillary techniques, including immunocytochemistry, biochemical measurements, and flow cytometry were considered necessary, re-aspiration was required to perform those studies. However, no molecular studies have been conducted in Japan.
In this study, the median frequency and overall ROM of follicular neoplasms were 3.9% and 11.4%, respectively. These data were calculated using NIFTP as a non-malignant neoplasm. The ROM in Japan was considerably lower than that in Western countries (23%), despite using the same diagnostic criteria and a similar frequency (7%). However, due to the unavailability of molecular testing for follicular neoplasm nodules, resection or follow-up is selected based on other clinical findings.[3,10] Surgical indications differ among institutions. A high-volume thyroid center described follicular neoplasm nodules with no cytological findings favoring malignancy, no ultrasonography findings of high suspicion, tumor size of <30 mm, and tumor volume-doubling rate of <1.0/year as low risk, which could be followed up without molecular testing.[10] Therefore, with regard to follicular tumors, it is difficult to define the differences in ROM between Japan and the West. Notably, in Japan, the ROM of follicular neoplasm was considerably lower than that of undetermined significance.
Suspicious for malignancy and malignant nodules typically undergo surgical resection; however, the resection rates were considerably low: suspicious for malignancy (77.8 %) and malignant (70.8 %). In Japan, thyroid nodules of >5 mm with strongly suspicious ultrasound findings are targeted for FNA.[3,11] Active surveillance has been accepted as an option for low-risk papillary thyroid microcarcinoma nodules.[12,13] Therefore, the low resection rate can be attributed to broader FNA indications and active surveillance.
This study has some limitations. The ROM was calculated based on cases that were resected and histologically diagnosed as malignant. Not all non-resected cases are benign, and it was not possible to definitively state that the nodules under follow-up are benign. However, non-malignant cases were those that could be followed for at least 1 year without any events. Diagnostic categories were used with original reports and have not been reviewed, except for cases of undetermined significance. Study data were obtained from institutions with large numbers of thyroid cytology cases and with surgeons, pathologists, and cytotechnologists who are experienced in thyroid disease. Thus, this study did not include data from institutions with few thyroid cases and with inexperienced diagnosticians. Nevertheless, our proposal could be accepted as the standard, providing reference values.
SUMMARY
This study determined the frequency, ROM, and recommended clinical management for thyroid cytopathology in Japan. They were different from those proposed by TBSRTC. In the future, our results will certainly be helpful in the revision of JSRTC and will contribute to the outcomes of Japanese patients with thyroid nodules.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this study are available from the corresponding author on request.
ABBREVIATIONS
FNA: Fine-needle aspiration
JSRTC: Japanese System for Reporting Thyroid Cytopathology
NIFTP: Noninvasive follicular thyroid neoplasm with papillary-like nuclear features
ROM: Risk of malignancy
TBSRTC: The Bethesda System for Reporting Thyroid Cytopathology
AUTHOR CONTRIBUTIONS
MHir: Conception and design of the work; MHir, RK, TA, TC, NY, SS, MT, YO, YM, MF, ES, HY, and MHig: Data collection, analysis, and interpretation; MHir and AS: Drafting the article; AS and TA: Critical revision of the article. All authors: Final approval of the version to be published. All authors meet ICMJE authorship requirements.
ACKNOWLEDGMENT
Not applicable.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institutional Review Board (approval number: Kuma Hospital; 20231109-1, Ito Hospital; 2024-3-2, Cancer Institute Hospital of the Japanese Foundation for Cancer Research; 2023-GB-185, Yamashita Thyroid Hospital; 20, Sagara Hospital;23-29, Showa University Northern Yokohama Hospital;2023-316-A, and Osaka Police Hospital;1865), and was in accordance with the 2024 Helsinki Declaration. The authors certify that they have obtained all appropriate patient consent.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
EDITORIAL/PEER REVIEW
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through an automatic online system.
FUNDING: Not applicable.
References
- The Bethesda system for reporting thyroid cytopathology. Thyroid. 2009;19:1159-65.
- [CrossRef] [PubMed] [Google Scholar]
- The 2023 Bethesda system for reporting thyroid cytopathology. Thyroid. 2023;33:1039-44.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid FNA cytology: The eastern versus western perspectives. Cancer Cytopathol. 2023;131:415-20.
- [CrossRef] [PubMed] [Google Scholar]
- Pathological diagnosis of general rules for the description of thyroid cancer by Japanese society of thyroid pathology and Japan association of endocrine surgery. Endocr J. 2022;69:139-54.
- [CrossRef] [PubMed] [Google Scholar]
- The Japanese reporting system for thyroid aspiration cytology 2019 (JRSTAC2019) Gland Surg. 2020;9:1653-62.
- [CrossRef] [PubMed] [Google Scholar]
- Introduction of histological classification and cytology reporting format of the Japanese general rules for the description of thyroid cancer with a special focus on the differences of the WHO histological classification and the Bethesda system of thyroid cytology. Endocr J. 2021;68:621-30.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of conventional smear and liquid-based cytology in adequacy of thyroid fine-needle aspiration biopsies without an accompanying cytopathologist. Sisli Etfal Hastan Tip Bul. 2022;56:353-9.
- [Google Scholar]
- Reappraisal of “cyst fluid only” on thyroid fine-needle aspiration cytology. Endocr J. 2017;64:759-65.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of malignancy and clinical outcomes of cyst fluid only nodules in the thyroid based on ultrasound and aspiration cytology. Diagn Cytopathol. 2020;48:30-4.
- [CrossRef] [PubMed] [Google Scholar]
- Criteria for follow-up of thyroid nodules diagnosed as follicular neoplasm without molecular testing-the experience of a high-volume thyroid centre in Japan. Diagn Cytopathol. 2022;50:223-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic strategies for thyroid nodules based on ultrasonographic findings in Japan. Cancers (Basel). 2021;13:4629.
- [CrossRef] [PubMed] [Google Scholar]
- Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: Consensus statements from the Japan association of endocrine surgery task force on management for papillary thyroid microcarcinoma. Thyroid. 2021;31:183-92.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term outcomes of active surveillance and immediate surgery for adult patients with low-risk papillary thyroid microcarcinoma: 30-year experience. Thyroid. 2023;33:817-25.
- [CrossRef] [PubMed] [Google Scholar]








