Translate this page into:
Fine-needle aspiration of a slowly enlarging neck mass in a 61-year-old woman: An interesting adult blue cell tumor in an unusual location
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Slowly enlarging, nontender, right neck mass for 2- to 3-months in a 61-year-old woman. Computed tomography (CT) showed ill-defined, necrotic, 2.8 cm × 2.4 cm × 2.5 cm mass located adjacent to and inferior to the tail of the right parotid gland. Fine-needle aspiration cytology (FNAC) [Figure 1] of the mass was cellular with dispersed to clustered pleomorphic epithelioid tumor cells with focal rosette-like structure, focal nuclear molding, irregular nuclear contours, “speckled” granular chromatin, bare nuclei and occasionally visible nucleoli. Lymphglandular bodies were absent. The tumor cells were immunoreactive for cytokeratin (CK) AE1/AE3, CK 20 with paranuclear dot-like immuostaining, and synaptohysin. Concurrent flow cytometric studies were negative for a significant lymphoid population.
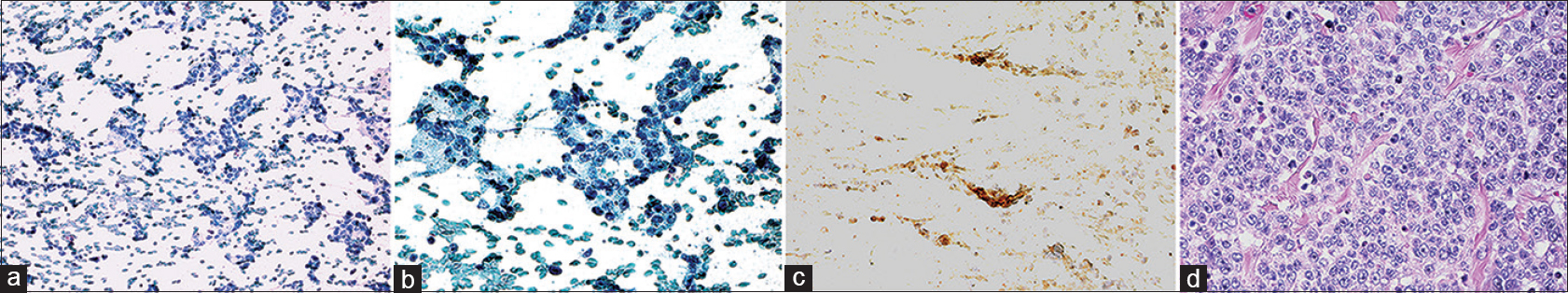
- (a) Aspirate were cellular with cells in clusters, small sheets, and small rosettes (Diff-Quik, ×200). (b) The cells with delicate cytoplasm had round to ovoid nuclei, coarse - clumped granular chromatin, and prominent nucleoli (Pap stain, ×400). (c) Cell block sections showed tumor cell Immunoreactivity for synaptophysin (×400). (d) Resection specimen showed the tumor cells organized as nests divided by thin fibrous septae. The cytomorphology of tumor cells was comparable to that noted in cytology smears (H and E, ×400)
QUESTION
Q1: What is your interpretation?
-
Squamous cell carcinoma (SCC)
-
Merkel cell carcinoma
-
Metastatic small cell carcinoma from lung primary
-
Follicular lymphoma.
ANSWER
Q1: (b) Merkel cell carcinoma.
Based on the tumor's cytologic appearance, immunohistochemical findings, and complex karyotype, a diagnosis of Merkel cell carcinoma involving the parotid gland was made.
Follow-up of the present case
The patient underwent subsequent superficial parotidectomy and neck dissection. The parotid gland and adjacent skeletal muscle were involved by tumor with florid lymphovascular and perineural invasion. Seven of 29 lymph nodes were positive for metastatic tumor.
Karyotyping showed a highly abnormal and complex hypodiploid karyotype in the tumor cells. In particular, nine cells showed monosomy 4, monosomy 13, and deletion 7q.
The patient began chemotherapy for merkel cell carcinoma and expired one month after diagnosis.
ADDITIONAL QUIZ QUESTION
Q2. What is the ideal immunohistochemical staining pattern for Merkel cell carcinoma?
-
Cytoplasmic positivity for synaptophysin, dot-like staining for keratin 20
-
Cytoplasmic positivity for CD56, nuclear staining for S100
-
Cytoplasmic positivity for thyroid transcription factor-1 (TTF-1), nuclear staining for keratin 20
-
Cytoplasmic positivity for CD45, dot-like staining for CAM5.2.
Q3. The immunohistochemical pattern of positive cytoplasmic staining for synaptophysin and chromogranin, positive nuclear staining for TTF-1, and negative staining for CK20 is most consistent with which small round blue cell tumor?
-
Poorly differentiated neuroendocrine tumor/small cell carcinoma
-
Merkel cell carcinoma
-
Melanoma
-
Metastatic poorly differentiated lung adenocarcinoma.
Q4. The most common tumor in the neck region in adult patients is:
-
Lymphoma
-
Rhabdomyosarcoma
-
Metastatic HPV-associated squamous cell carcinoma
-
Metastatic Merkel cell carcinoma.
ANSWERS TO ADDITIONAL QUIZ QUESTIONS
Q2: A; Q3: A; Q4: C.
BRIEF REVIEW OF THIS TOPIC
Small round blue cell tumors (SRBCTs) are amenable to FNA biopsy due to their high cellularity and frequent appearance in subcutaneous locations such as the head and neck. However, the similar cytomorphology of SRBCTs can lead to a wide differential diagnosis. Pathologist evaluation of the cytomorphology of the aspirate smears can successfully narrow the workup and conserve diagnostic material. An initial branchpoint we use in the workup of SRBCTs in the head and neck is the age of the patient. Most of the differential diagnoses that would be considered in an infant or child would not apply here.
In adults, the most common tumor in the neck region is metastatic carcinoma to lymph nodes or parotid gland. In particular, human papillomavirus (HPV)-associated SCC and basaloid SCC should be high on the differential for any adult presenting with a neck mass. HPV-associated SCC and basaloid SCC can be nonkeratinizing. FNAC shows cells with hyperchromatic nuclei, irregular and angulated nuclear contours, and scant to moderate amounts of dense cytoplasm. Tumor diathesis is common. In the cell block, tumor cells are arranged in cohesive nests with comedo-type necrosis. FNAC examination of the neck masses is frequently the first modality to raise the possibility of a metastatic SCC, setting off a search for the primary site frequently in the base of tongue or tonsil. Currently, there is no specific guideline for HPV testing or p16 cutoff value on FNAC for the establishment of HPV-driven carcinoma.[23]
Lymphomas are also high on the differential for any lateral neck mass. The most commonly occurring B-cell lymphomas are diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma. However, myriad other hematolymphoid neoplasms, including T-cell lymphomas, may also be present at this site. DLBCL is composed of large lymphoid cells with fine chromatin, single to multiple nucleoli, and scant to moderate pale cytoplasm.[4] Low-grade follicular lymphomas can be particularly difficult to discern from reactive lymph nodes on FNAC.[5] For this reason, allocation of fresh tissue for flow cytometric studies can help establish the presence of a monoclonal B-cell population, and the immunophenotype may suggest a more specific diagnosis. Differentiation between follicular lymphoma (particularly with transformation) and DLBCL and the accurate subclassification of many lymphomas is not possible based solely on FNAC sampling. This requires core needle or excisional biopsy. However, a diagnosis of a B-cell lymphoproliferative disorder on FNAC narrows the differential diagnosis significantly and can streamline the workup at the time of needle core or excisional biopsy. Furthermore, one can recommend further laboratory and imaging studies to determine the extent of systemic involvement as well as to help identify lymph nodes with the most worrisome features for biopsy (e.g., highest maximum standardized uptake values on positron emission tomography CT scan).
Neuroendocrine tumors, particularly small cell carcinoma, can form rosettes composed of monotonous small blue cells. Pulmonary, gastroenteropancreatic, gynecologic, or genitourinary small cell carcinoma can present initially as metastatic lesions. Small cell carcinoma can also present as primary salivary gland neoplasms, most commonly the parotid gland, without antecedent or concurrent visceral primary lesions. Regardless of the site, the cells have small to medium-sized nuclei with stippled, “salt-and-pepper” granular chromatin, inconspicuous nucleoli, and scant fragile cytoplasm. Nuclear molding is characteristically seen in small cell carcinoma. Necrosis is common. A Ki67 or MIB-1 immunostain highlights the high proliferation rate. These cells are positive for neuroendocrine markers, cytokeratins (in a paranuclear dot-like pattern), and epithelial membrane antigen. While TTF-1 is usually positive in small cell carcinomas of pulmonary origin, it can also be positive in small cell carcinomas of other sites, such as bladder and prostate. Correlation with imaging findings is essential when immunohistochemical markers cannot determine a cell of origin in metastatic lesions.[6]
Merkel cell carcinoma may present as a primary cutaneous lesion in the head and neck, as a metastatic lesion in lymph nodes, and as a primary salivary gland lesion.[6] As in case 2 above, the cells are frequently dispersed and have an epithelioid appearance. Like other neuroendocrine tumors, the nuclei of Merkel cell carcinoma demonstrate “salt-and-pepper” chromatin, inconspicuous to occasional visible nucleoli, nuclear molding, and crush artifact. Merkel cell carcinomas are characteristically positive for neuroendocrine and epithelial markers. They show cytoplasmic positivity for synaptophysin, chromogranin, and CD56, and paranuclear dot-like staining for low-molecular-weight keratin and cytokeratin 20. In contrast to small cell carcinomas, Merkel cell carcinomas are always negative for TTF-1.[7] Cytogenetic analysis of Merkel cell carcinoma has shown complex karyotypes, with trisomy 6 and chromosomal losses reported.[8] Merkel cell carcinomas have been reported as both primary and secondary carcinomas.[910]
COMPETING INTERESTS' STATEMENT BY ALL AUTHORS
For all authors, the authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
SC carried out literature review, coordinated submission, and drafted and edited the manuscript. SH collected clinical cases, performed additional literature review, and edited the manuscript. DYL collected clinical cases and edited the manuscript. RCM photomicrographs and drafted the manuscript. MVL collected cases, and helped draft and edit the manuscript. NAM conceived of the quiz case, collected clinical cases, performed additional literature review, and edited the manuscript. All authors read and approved the final manuscript.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from Institutional Review Board (or its equivalent).
LIST OF ABBREVIATIONS (In alphabetic Order)
CT - Computerized tomography
DLBCL - Diffuse large B-cell lymphoma
FISH - Fluorescence in situ hybridization
FNA - Fine-needle aspiration
HPV - Human papilloma virus
RMS - Rhabdomyosarcoma
SCC - Squamous cell carcinoma
SRBCT - Small round blue cell tumor.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted through automatic online system.
REFERENCES
- Approach to the diagnosis of soft tissue tumors. In: Goldblum JR, Weiss SW, Folpe AL, editors, eds. Enzinger and Weiss's Soft Tissue Tumors (5th). New York: Elsevier; 2013.
- [Google Scholar]
- The utility of p16 immunostaining in fine needle aspiration in p16-positive head and neck squamous cell carcinoma. Hum Pathol. 2016;54:193-200.
- [Google Scholar]
- Adequacy of fine-needle aspiration specimens for human papillomavirus infection molecular testing in head and neck squamous cell carcinoma. Cytojournal. 2013;10:21.
- [Google Scholar]
- Sinonasal small round blue cell tumors: An approach to diagnosis. Semin Diagn Pathol. 2016;33:91-103.
- [Google Scholar]
- Cytology: Diagnostic Principals and Clinical Correlates. (4th). New York: Elsevier; 2014.
- [Google Scholar]
- Tumors of the salivary glands. In: Fletcher CD, ed. Diagnostic Histopathology of Tumors (4th). New York: Elsevier; 2013.
- [Google Scholar]
- Recent advances in the biology of Merkel cell carcinoma. Hum Pathol. 2011;42:1063-77.
- [Google Scholar]
- Primary Merkel cell carcinoma of the parotid gland. Ear Nose Throat J. 2010;89:E24-7.
- [Google Scholar]
- Secondary merkel cell carcinoma manifested in the parotid. Case Rep Dermatol Med. 2013;2013:960140.
- [Google Scholar]







