Translate this page into:
Myoepithelioma of soft tissue in the gluteal region: Diagnostic pitfall in cytology
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 14-year-old male presented with gradually enlarging, tender swelling in the left gluteal region for 3 months with a history of fall down from school bench. On examination, it was suspected as hematoma in the left gluteal region. On palpation, swelling was well-circumscribed firm with normal overlying skin. Ultrasonography (USG) showed well-defined, heterogeneously hyper-echoic lesion measuring approximately 3.5 cm × 5.7 cm noted in the subcutaneous plane. Magnetic resonance imaging (MRI) revealed well-defined lobulated lesion in subcutaneous plane in paramedian location in the left gluteal region. Anteriorly, it reached up to coccyx with no deeper extension/communication. Figure 1a–d shows cytomorphological features of the fine needle aspirate (FNA) of the lesion.
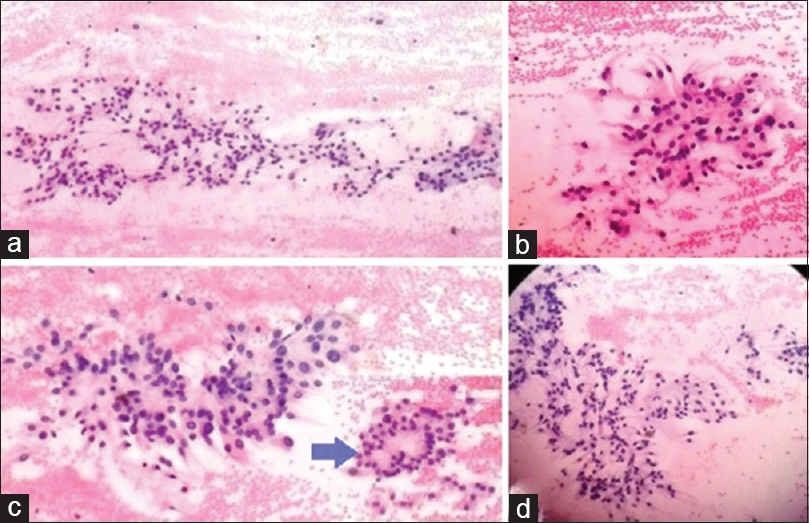
- Fine needle aspiration of the thigh lesion. (a) Cytology shows loosely arranged round to oval cells having eosinophilic cytoplasm in the fibrillary and myxoid background (H and E,100 ×). (b) Many loosely arranged cuboidal to columnar cells having polar eosinophilic cytoplasmic process in fibrillary background (H and E, 100). (c) Cytology showing oval and spindle cells having mild cytologic atypia (H and E, 400). Inset (zoomed) cells arrangement in rosette fashion (arrow). (d) Round to oval cells having plasmacytoid nuclei and eosinophilic cytoplasm in the fibrillary and myxoid background (H and E, 100)
QUESTION
Q1: What is your interpretation?
-
Extradural myxopapillary ependymoma
-
Chordoma
-
Myoepithelioma of soft tissue
-
Extraskeletal myxoid chondrosarcoma.
ANSWER
The correct cytopathology interpretation is:
C. Myoepithelioma of soft tissue.
Cytology (FNAC) is a simple and minimally invasive method for evaluating soft tissue lesions. Myoepithelial cells are normally contractile epithelial cells surrounding the acini and ducts of glands. Myoepithelioma is defined as tumor composed of myoepithelial cells with or without ductal structures.[1] Soft-tissue myoepithelioma is a very rare neoplasm as against to salivary gland myoepithelioma. It is largely unrecognized and underreported entity with considerable morphologic and architecture variability.
On Cytology, the smears were moderately cellular, showing loosely arranged clusters, sheets, isolated cells, rosette-like arrangement with fibrillary material within. The cells were round to oval and spindle shaped with many showing plasmacytoid appearance with bland round nuclei and finely distributed chromatin. Some cells had fibrillary tapering eosinophilic cytoplasmic process. Cytodiagnosis of myoepithelioma of soft tissue or extradural myxopapillary ependymoma was offered and advised biopsy/excision.
Rarely, myxopapillary ependymoma presents as extradural lesion as presacral/retrosacral soft tissue arising from ependymal rest. MRI revealed features as shown in Figure 2a–c.
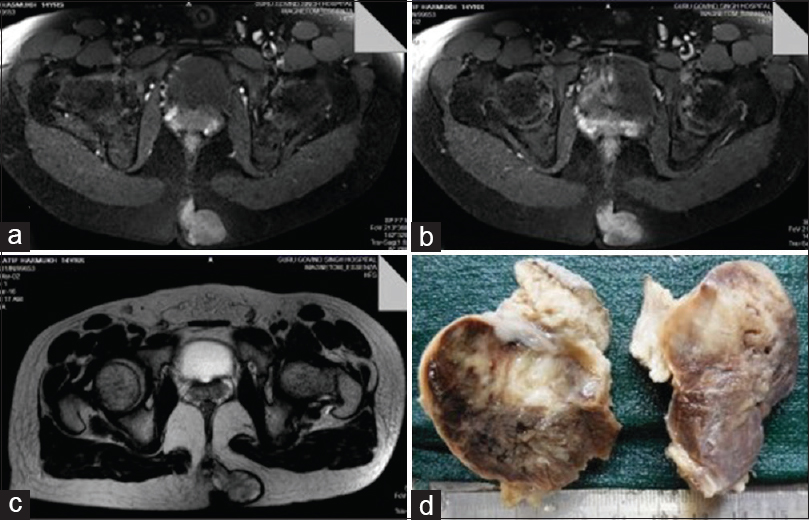
- (a) Magnetic resonance imaging showing well-defined lobulated lesion shows heterogeneous enhancement on postcontrast study, approximately size (27 mm × 43mm × mm) is noted in subcutaneous plane, paramedian location in the left gluteal region. Anteriorly, it lesion reaches up to tip coccyx. (b) The lesion is hypointense onT1-weighted image. (c) The lesion is heterogeneously hyperintense onT2-weighted image. (d) Gross photograph shows subcutaneous tumor Heterogeneous gray-white and glistening brown cut surface
Cytomorphological features of chordoma
-
Abundant metachromatic myxoid background- “Physaliferous cell” which features bubbly cytoplasm and an eccentric, round and bland nucleus
-
Other cell types may have a fusiform or stellate morphology, uniform eosinophilic cytoplasm without bubbles.
Cytomorphological features of extradural myxopapillary ependymoma
-
Usually yields highly cellular smears, slim columnar cells are arranged radially around vascularized stromal cores and globules of hyaline-myxoid appears as intense metachromatic material
-
The cells are loosely overlapped and display distinctive bipolar and unipolar processes. Nuclei have finely granular chromatin and inconspicuous nucleoli.
Cytomorphological features of extraskeletal myxoid chondrosarcoma
-
Abundant myxoid background, variable arrangement of tumor cells, clusters, branching, strands, cell balls and dispersed cells
-
Chondroblastoma like nuclei with nuclear folds or indentations (coffee bean nuclei). Cells are variably rounded, elongated and fusiform. Nuclei are rounded, ovoid or spindle-shaped.
Preoperative cytologic diagnosis of soft-tissue myoepithelioma is very difficult and challenging due to above-mentioned morphologic mimics, leading to diagnostic dilemma and pitfalls. Cytology of soft tissue myoepithelioma shows rosette with fibrillary material completes the morphological mimicry of extradural myxopapillary ependymoma. It is important to recognize the lesion correctly as treatment implications differ.
Chordoma - en bloc resection and/or adjuvant radiotherapy.
Extradural myxopapillary ependymoma- complete surgical excision, may need adjuvant radiotherapy.
Extraskeletal myxoid chondrosarcoma - conservative surgery.
ADDITIONAL QUIZ QUESTIONS
Q2: Which age group malignant myoepithelial tumor frequently occur?
-
0–18 years (pediatric age group)
-
20–60 years (adult age group)
-
Above 65 years (elderly age group)
-
All of the above.
Q3: Following immunohistochemistry (IHC), which IHC marker is NOT expressed in myoepithelioma of soft tissue?
-
S-100
-
Pan-cytokeratin
-
Vimentin
-
Desmin.
Q4: Which gene rearrangement is commonly seen in myoepithelioma of soft tissue?
-
WT1
-
PLAG1
-
EWSR1
-
FUS.
ANSWER TO ADDITIONAL QUESTIONS
Q2: A; Q3: D; Q4: C.
Q2. A) The age incidence of these tumors ranged from 3 to 83 years, with a mean age of 38 years.[2] There is no significant gender predilection. Malignant myoepithelial tumor frequently occur in pediatric age group (0–18 years).[3] In the series by Hornick and Fletcher, 61 out of 101 tumors were classified as histologically benign, whereas 40 tumors were felt to be histologically malignant. Cytological features determine malignancy in myoepithelial tumor and it frequently occurs in pediatric age groups.[2]
Q3. D) Most sensitive IHC markers for soft tissue myoepithelioma include wide-spectrum cytokeratin (nearly 100%), S-100 (87%), calponin (86%), and glial fibrillary acidic protein (GFAP) (50%). Desmin is usually negative.[4] Coexpression of cytokeratin, vimentin, and S-100 helps exclude other morphological mimicker. Consistent expression of S-100 excludes most metastatic carcinoma, except those from the breast.[5]
Q4. C:) Recent cytogenetic studies demonstrated EWSR1 gene rearrangement detectable in 45% of myoepithelial tumors of soft tissue. The common fusion partner genes include PBX1, POU5F1, and ZNF444 which differ from translocations involving PLAG1 and HMGA2 genes reported in myoepithelial tumors of the salivary glands.[67] It indicates different pathogenesis for myoepithelial tumor of soft tissue.[4] EWSR1-POU5F1 gene fusion resulting from t (6;22)(p21;q12) has been found in deeply located soft tissue tumors, with clear cells disposed of in the nests and in a malignant bone tumor.[8]
BRIEF REVIEW OF THE TOPIC
The patient underwent complete surgical excision. The specimen consisted of a well circumscribed ovoid firm gray-white mass. The cut surface showed tan whitish brown mass with glistening myxoid surface [Figure 2d]. Postoperative period was uneventful. Histopathologically, the tumor showed a lobulated growth pattern with cords, trabeculae and rosette-like arrangement of bland cells having round eccentric nucleus embedded in a myxoid, collagenous, fibrillary stroma. No duct structure was identified. No nuclear pleomorphism, necrosis or mitotic figures were present [Figure 3a–d]. Final diagnosis of myoepithelioma of soft tissue was considered and further substantiated by IHC. IHC studies showed that strong diffuse positive staining of tumor cells with cytokeratin AE1/AE3, CAM5.2, epithelial membrane antigen, S-100 and vimentin confirms the diagnosis of myoepithelioma of soft tissue.
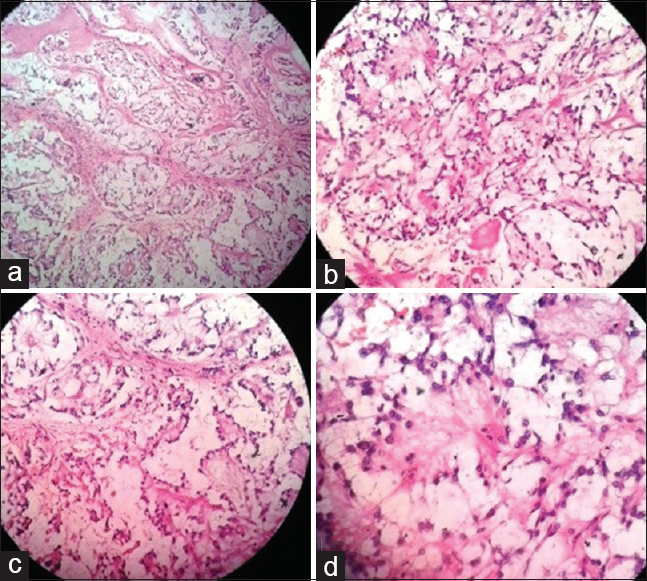
- Histopathology of the thigh lesion. (a) Tumor cells arranged in lobules in myxoid background separated by fibrous septa (H and E, 200). (b & c) Tumor cells arranged in cords, trabeculae, and rosette like arrangement in the myxoid and fibrillary background (H and E, 400). (d) Tumor cells arranged in rosette with fibrillary material within (H and E, 400)
In 1874, Minssen first used the term mixed tumor to describe tumors of the parotid gland with both epithelial and mesenchymal features.[29] In 2002, the World Health Organization (WHO) introduced myoepithelioma in the classification of soft tissue tumor. Following publication of a relatively small series, Fletcher has now seen over 400 additional examples, suggesting that pathologists are showing more willingness to propose this diagnosis.[5]
Hornick and Fletcher in their series described 101 cases where majority arose in the lower limb/limb girdles followed by upper limb/limb girdles, head, neck and trunk. Out of which, only 5 (5.0%) tumors were located in the buttock area.[2] Only 6% cases occur in the second decade and 54% cases occur in subcutaneous plane.[2]
Very few cases of cytodiagnosis of myoepithelioma of soft tissue are reported in literature. Wang et al. described FNAC of myoepithelioma of the lower chest wall showed round to oval epithelioid cells in myxoid background.[4] Narick et al. described plump spindle cells in myxoid background on FNAC of thyroid nodule.[10] Park et al. described imprint cytology of myoepithelial tumor in forearm showing round to spindle, epithelioid and plasmacytoid cells in the myxoid background.[11] Machado et al. described FNAC of soft tissue myoepithelial carcinoma with rhabdoid features and EWSR1 rearrangement.[12]
In the recent WHO classification of softtissue tumor (2013), myoepithelioma is placed under the category- tumors of uncertain differentiation (intermediate–rarely metastasizing variety). Although most myoepitheliomas of soft tissue are benign, local recurrence rate is 20%. Out of the 33 histologically benign cases with follow-up, 6 (18%) cases locally recurred, but none metastasized (mean follow-up of 36 months).[2] The 5-year event-free survival and relapse rate for low-grade soft tissue myoepitheliomawere 88% and 29%, respectively.[13]
Complete surgical excision is the treatment of choice for benign myoepithelial tumor of soft tissue. In the present case, no cytological features of malignancy were identified so advised for routine yearly follow-up after complete excision.
Myoepithelioma of soft tissue is clinically heterogeneous tumors, with varied clinical behavior, and several observed histology, cytogenetic findings, and molecular signatures. Cytopathologist should be aware of bland nature of round, epithelioid and plasmacytoid cells in myxoid and fibrillary background to hit the correct diagnosis.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE. Each author has participated sufficiently in the work and takes responsibility for appropriate portions of the content of this article.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from Institutional Review Board.
LIST OF ABBREVIATIONS (In alphabetic order)
EMA - Epithelial membrane antigen
FNAC - Fine needle aspiration cytology
GFAP - Glial fibrillary acidic protein
H and E - Hematoxylin & eosin
IHC - Immunohistochemistry
MRI - Magnetic resonance imaging
USG - Ultrasonography
WHO - World health organization
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
ACKNOWLEDGMENT
We are very thankful to Dr. Pravina Santwani, Professor & Head, Department of pathology and Dr. Nandini J. Desai, Professor of Pathology and Medical superintendent, G.G.G.hospital, Jamnagar, Dr. Shamim Sheikh, Associate Professor of Pathology, for their kind support and guidance.
REFERENCES
- Myoepithelioma of soft tissue in the knee: A case report of an unusual location. Indian J Pathol Microbiol. 2016;59:254-6.
- [Google Scholar]
- Myoepithelial tumors of soft tissue: A clinicopathologic and immunohistochemical study of 101 cases with evaluation of prognostic parameters. Am J Surg Pathol. 2003;27:1183-96.
- [Google Scholar]
- Myoepithelial neoplasms of soft tissue: An updated review of the clinic-pathologic, immunophenotypic, and genetic features. Head Neck Pathol. 2015;9:32-8.
- [Google Scholar]
- Fine-needle aspiration of soft tissue myoepithelioma. Diagn Cytopathol. 2016;44:152-5.
- [Google Scholar]
- Recently characterized soft tissue tumors that bring biologic insight. Mod Pathol. 2014;27(Suppl 1):S98-112.
- [Google Scholar]
- EWSR1-POU5F1 fusion in soft tissue myoepithelial tumors. A molecular analysis of sixty-six cases, including soft tissue, bone, and visceral lesions, showing common involvement of the EWSR1 gene. Genes Chromosomes Cancer. 2010;49:1114-24.
- [Google Scholar]
- High-resolution genomic profiling of adenomas and carcinomas of the salivary glands reveals amplification, rearrangement, and fusion of HMGA2. Genes Chromosomes Cancer. 2009;48:69-82.
- [Google Scholar]
- EWSR1 is fused to POU5F1 in a bone tumor with translocation t(6;22)(p21;q12) Genes Chromosomes Cancer. 2005;43:217-22.
- [Google Scholar]
- Mixed tumors and myoepitheliomas of soft tissue: A clinicopathologic study of 19 cases with a unifying concept. Am J Surg Pathol. 1997;21:13-22.
- [Google Scholar]
- Fine needle aspiration cytology of a myoepithelioma presenting as a thyroid nodule. Diagn Cytopathol. 2015;43:153-7.
- [Google Scholar]
- Imprint cytology of soft tissue myoepithelioma: A case study. Korean J Pathol. 2013;47:299-303.
- [Google Scholar]
- Soft tissue myoepithelial carcinoma with rhabdoid-like features and EWSR1 rearrangement: Fine needle aspiration cytology with histologic correlation. Diagn Cytopathol. 2015;43:421-6.
- [Google Scholar]
- Myoepithelioma of soft tissues: A single institution retrospective case series. Am J Clin Oncol 2016 [Epub ahead of print]
- [Google Scholar]







