Translate this page into:
Can cytomorphology of granulomas distinguish sarcoidosis from tuberculosis? Retrospective study of endobronchial ultrasound guided transbronchial needle aspirate of 49 granulomatous lymph nodes
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The differential diagnosis of tuberculosis (TB) and sarcoidosis on fine needle aspiration material is very challenging in tubercular endemic regions. We carried out a pilot study to explore cytomorphologic features of granulomas which could help in differentiation between sarcoidosis and TB. Final diagnoses in these patients were based on clinical, microbiologic and follow-up studies.
Materials and Methods:
Endobronchial ultrasound guided transbronchial needle aspiration smears of 49 consecutive patients with a final cytologic diagnosis of granulomatous lymphadenitis were reviewed. Based on cytologic features two cytologic categories were enunciated and the results were correlated with microbiologic studies and/follow-up of minimum of 6 months.
Results:
The cytologic categories did not correlate with the final clinical outcome of patients.
Conclusions:
Different patterns of granulomas observed in cytology smears do not help distinguish TB from sarcoidosis. The novel non-invasive techniques of mediastinal sampling though help in confirming granulomatous pathology, distinction between these entities and treatment decisions still depend upon correlating cytologic, microbiologic, clinical and radiological data in a large number of cases in tubercular endemic regions.
Keywords
Endobronchial ultrasound guided transbronchial needle aspiration
granulomas
sarcoidosis
tuberculosis
INTRODUCTION
Sampling of mediastinal lymph nodes by endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA) and endoscopic ultrasound guided fine-needle aspiration (EUS FNA) have been validated for staging in patients with lung cancers. EBUS-TBNA has also been successfully used to diagnose centrally located lung tumors.[123] In Western countries, it has also emerged as a safe tool to establish granulomatous pathology in suspected cases of sarcoidosis.[4] In countries with high prevalence of tuberculosis (TB), mediastinal lymphadenitis is most often due to TB while sarcoidosis is a less common cause.[5] The differential diagnosis of TB and sarcoidosis is very challenging in these regions. The clinic-radiologic features of two are overlapping.[6] Both can present with non-caseating granulomas (NCG). Results of culture and Zeihl-Neelsen (ZN) staining are variable with low sensitivity in non-necrotic lesions. The smear positivity (ZN stain) ranges from 18% to 75% in various studies and is lower in non-necrotic lesions. The culture positivity though higher than smear positivity is also variable and is reported as approximately 50% in granulomatous lesions.[7] Most patients with granulomatus lesions are put on therauptic anti-tubercular therapy (ATT) trials. A diagnosis of sarcoidosis is sometimes only made after failure of response to repeated courses of ATT.
We carried out a pilot study to explore if cytomorphologic features of granulomas could help in differentiation between sarcoidosis and TB. Final diagnosis in these patients was based on clinical, microbiologic and follow-up studies.
MATERIALS AND METHODS
EBUS-TBNA smears of 49 consecutive patients with a final cytologic diagnosis of granulomatous lymphadenitis were reviewed. Both Papanicolaou and May Grunwald Giemsa stained smears were available. The smears were reviewed by three trained cytopathologist without knowledge of clinical or microbiological data.
Features looked for were the presence of granulomas, size and number of granulomas, loose or compact granulomas, presence or absence of necrosis and inflammatory exudate.
Based on these features granulomas were classified as caseating granulomas (CG) or NCG. The latter (NCG) were further divided into two categories:
NCG I – The number of granulomas was less and the size was small. They were made of few epithelioid cells that were well spaced out. The epithelioid cells appeared to be falling away from margins of granulomas [Figure 1].
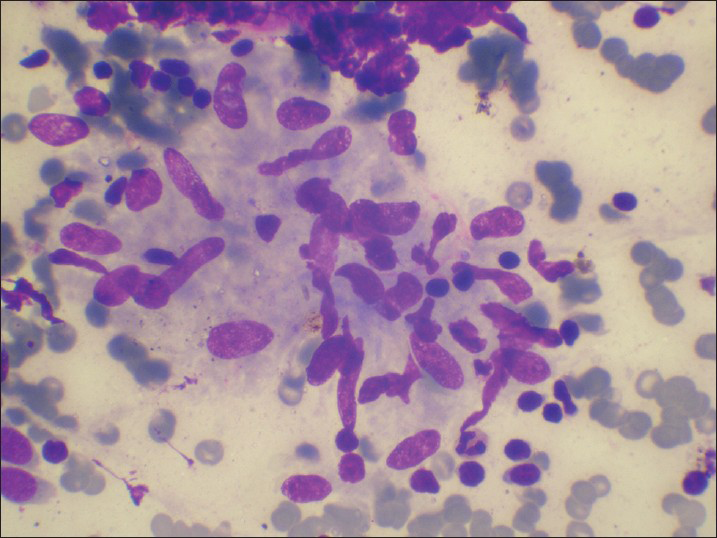
- Small granulomas made of few epithelioid cells. The epithelioid cells are well spaced out
NCG II – The number of granulomas was more and they were composed of numerous tightly packed epithelioid cells [Figure 2].

- Large granulomas, with numerous epithelioid cells, packed tightly
Presence or absence of giant cells was not used as a criterion in this classification.
A case was labeled as TB if CG or NCG I were observed while cases with NCG II type of granulomas were labeled as sarcoid. This hypothesis was based on anecdotal observations by us while reporting mediastinal granulomatous lymphadenopathy (LAP). Cytological categories so enunciated were correlated with the final diagnosis in each case. A final diagnosis of TB was considered if acid fast bacilli (AFB) could be demonstrated on ZN staining of smears or culture for Mycobacterium tuberculosis (MTB) was positive or the patient showed therauptic response to ATT. A final diagnosis of sarcoidosis was considered in patients where no AFB was demonstrated in smears and/or culture; and therauptic response to steroids or hydroxychloroquine was seen on follow-up.
RESULTS
Table 1 depicts the type of granulomas in these cases. NCG lymphadenitis were observed in 34 cases while in 14 cases caseation was observed.
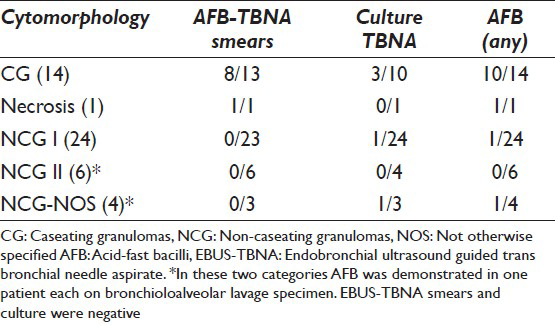
The NCG were further classified into category I or II. 4 cases could not be classified further due to scant material and were labeled as NCG-Not otherwise specified (NOS)
Amongst the CG AFB was demonstrated by ZN staining in eight of the 13 cases. It was not done in one case due to scant material. The case with only necrosis showed strong AFB positivity. Amongst the NCG, ZN staining was negative in 32 cases and not done in 2 cases. Culture for MTB using material obtained by EBUS was performed in 10 cases with CG and was positive in 3 cases. In two of the 3 cases, smears were negative. MTB culture was performed in 26 of the 34 cases with NCG and was positive in 2 cases. In another 2 patients, AFB was demonstrated in bronchioloalveolar lavage (BAL) specimen.
Follow-up and correlation of data
Based upon clinical and radiologic features, EBUS-TBNA results (where helpful in picking up AFB or CG) and therauptic follow-up for at least 6 months, final diagnosis are given in Table 2.
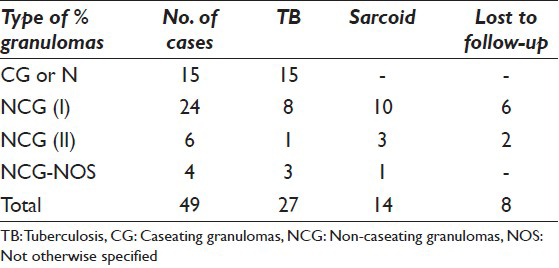
Eight patients did not complete 6 months follow-up. As is evident from Table 2, cytomorphologic classification of NCG did not correlate with final diagnosis of patients. Of the cases showing NCG I pattern (which was considered consistent with TB in our study), almost 55.5% patients turned out to be sarcoid.
DISCUSSION
TB is the major cause of mediastinal LAP in India. Until the recent advent of EUS FNA/EBUS-TBNA, patients with mediastinal LAP warranted therauptic ATT trial. However, recently these modalities are being increasingly used to elucidate etiology and exclude alternate diagnosis of lymphoma, metastatic carcinoma and sarcoidosis.[8] In a recent publication of EUS FNA of mediastinal lymph nodes from our center, granulomatous pathology was present in 206 of 269 cases studied. Only 76 of 206 cases could be further categorized as TB based on the presence of necrosis or AFB positivity on ZN staining. Though EUS FNA confirmed the presence of granulomatous lymphadenitis, the dilemma of TB versus sarcoidosis could not be resolved in patients with overlapping clinico-radiologic features from tubercular endemic areas.[9]
Few studies in the literature have evaluated the role of EBUS-TBNA in diagnosis of TB. Most of these do not address the dilemma of TB versus sarcoidosis.
Navani et al.,[10] reported that with the use of EBUS-TBNA, a diagnosis of TB could be established in 146 of the 156 patients with intrathoracic tubercular lymphadenitis. Their study included only patients with a confirmed diagnosis or unequivocal clinical and radiologic response to ATT during follow-up for a minimum period of 6 months. Cytological findings in EBUS-TBNA smears were granulomas with necrosis (68 cases), granulomas without necrosis (58 cases) and only necrosis (8 cases). Further smears were positive for AFB in 27 cases while in 74 cases AFB grew on culture. Smears were positive with negative culture in 8 cases. Thus, microbiologic confirmation was obtained in 82 of the 146 cases. They concluded that granulomas without caseation along with supportive clinical evidence and response to therapy be considered as consistent with final diagnosis of TB. Study of Navani et al., cannot be compared with the present study as the sample selection is different. They included only patients with a confirmed diagnosis of TB and studied cytological and microbiologic findings. Present study included cases with granulomas in EBUS-TBNA smears without consideration of clinical and radiologic features. However like Navani et al., we also found NCG in patients finally diagnosed as TB.
Hassan et al.,[11] demonstrated that EBUS-TBNA performed well in diagnosis of isolated intrathoracic TB. It confirmed TB in 19/24 patients with high pre-test probability of TB.
Fristcher-Ravens et al.,[12] did a prospective study to investigate diagnostic yield of EUS FNA in differentiation between sarcoidosis and TB. They differentiated TB from sarcoidosis predominantly based on “dirty background” in TB and “clean background” in sarcoidosis. In their study, EUS FNA cytology alone led to diagnosis of TB in 24/28 cases. When bacteriological studies were taken into account EUS FNA provided diagnosis in 27/28 cases. However, 3 patients with a “clean background” and cytologic diagnosis of sarcoidosis had positive culture for MTB.
In the present study, we attempted to classify NCG into TB and sarcoidosis based on cytologic features. The hypothesis was based on our observation that two distinct morphologic patterns of granulomatous lymphadenitis were observed in smears. Few small loose granulomas were observed more commonly in TB compared to numerous compact granulomas in sarcoidosis. However, this observation could not be substantiated in the present study.
Out of 49 patients, 27 were confirmed to be TB. Tubercular etiology could be established on EBUS-TBNA (cytology and microbiology) in 17 patients. Another 2 patients had AFB demonstrated in BAL specimen. 8 patients were confirmed as TB and 14 as sarcoidosis based on clinical and radiologic grounds. Sampling of mediastinal lymph nodes by EUS FNA and EBUS-TBNA is been increasingly done nowadays in tubercular endemic regions with clinical suspicion of TB versus sarcoidosis. Though different patterns of granulomas are observed in smears, these do not correlate with the diagnosis of TB and sarcoidosis. Further categorization of granulomatous pathology is not possible in a large subgroup of patients who have NCG with negative ZN staining and culture.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author. Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article. GK, AD, PB and KV contributed in conception and design of the study. GK, AD, JA and KV contributed in data acquisition, analysis and interpretation of data. GK, JA, PB and KV drafted and critically analyzed the article. All authors read and approved the final manuscript. Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
This was a retrospective analysis of the data and all the procedures were done after obtaining informed consents from patients; hence, ethics committee had given exemption.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through automatic online system.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2013/10/1/19/119008
REFERENCES
- Diagnosis of mediastinal adenopathy-real-time endobronchial ultrasound guided needle aspiration versus mediastinoscopy. J Thorac Oncol. 2008;3:577-82.
- [Google Scholar]
- Endobronchial ultrasound-guided transbronchial needle aspiration cytology: A state of the art review. Cytopathology. 2010;21:6-26.
- [Google Scholar]
- Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and metaanalysis. Chest. 2007;131:539-48.
- [Google Scholar]
- Endobronchial ultrasound for the diagnosis of pulmonary sarcoidosis. Chest. 2007;132:1298-304.
- [Google Scholar]
- Endoscopic ultrasound: Imaging techniques and applications in the mediastinum. Trop Gastroenterol. 2010;30:S4-19.
- [Google Scholar]
- Correlation of fine needle aspiration cytology, smear and culture in tuberculous lymphadenitis: A prospective study. J Postgrad Med. 2002;48:113-6.
- [Google Scholar]
- Endoscopic ultrasound (EUS) features of mediastinal tubercular lymphadenopathy. Hepatogastroenterology. 2011;58:819-23.
- [Google Scholar]
- Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of mediastinal lymph nodes: Experience from region with high prevalence of tuberculosis. Diagn Cytopathol 2011 doi: 10.1002/dc21698
- [Google Scholar]
- Utility of endobronchial ultrasound-guided transbronchial needle aspiration in patients with tuberculous intrathoracic lymphadenopathy: A multicentre study. Thorax. 2011;66:889-93.
- [Google Scholar]
- EBUS-TBNA performs well in the diagnosis of isolated thoracic tuberculous lymphadenopathy. Am J Respir Crit Care Med. 2011;183:136-7.
- [Google Scholar]
- Granulomatous mediastinal adenopathy: Can endoscopic ultrasound-guided fine-needle aspiration differentiate between tuberculosis and sarcoidosis? Endoscopy. 2011;43:955-61.
- [Google Scholar]








