Translate this page into:
Comparison of small biopsy and cytology specimens: Subtyping of pulmonary adenocarcinoma

*Corresponding author: Lihua Zhang, Department of Pathology, Zhongda Hospital, School of Medicine, Southeast Universi, Nanjing, China. 15905179393@126.com
-
Received: ,
Accepted: ,
How to cite this article: Ma C, Zhang L. Comparison of small biopsy and cytology specimens: Subtyping of pulmonary adenocarcinoma. CytoJournal 2023;20:5.
Abstract
Objectives:
The aims of this study was to investigate the use of cytologic samples for subclassification of lung adenocarcinoma and the cytologic-histologic correlation in lung adenocarcinoma subtypes using small samples.
Methods and Methods:
Cytological characteristics of lung adenocarcinoma subtypes were summarized by a literature review. Cytology samples from 115 patients with lung adenocarcinoma confirmed by small biopsies were classified by subtype. The diagnostic concordance of subtypes between biopsy and cytology samples was assessed.
Results:
Among the 115 cases, 62 (53.9%) had acinar predominant pattern, 16 (13.9%) were papillary predominant pattern, 29 (25.2%) had solid predominant pattern, 3 (2.6%) had lepidic predominant pattern, and 5 (4.3%) had micropapillary predominant pattern. All corresponding cytologic samples were classified into five subtypes based on cytomorphology features, with concordance rates of 74.2% (46 patients) in c-acinar subtype, 56.3% (nine patients) in c-papillary subtype, 24.1% (seven patients) in c-solid subtype, 66.7% (two patients) in c-lepidic subtype, and 40% (two patients) in c-micropapillary subtype. Collectively, the cytology and small biopsy concordance rate was approximately 57.4%.
Conclusion:
Subtyping of lung adenocarcinoma using cytologic specimens is challenging and the consistency rate varies with the subtype. Acinar predominant tumors have an excellent cytologic-histologic correlation compared to tumors with predominant solid or micropapillary pattern. Evaluating cytomorphologic features of different lung adenocarcinoma subtypes can reduce the false-negative rate of lung adenocarcinoma, particularly for the mild, atypical micropapillary subtype, and improve diagnostic accuracy.
Keywords
Lung neoplasms
Diagnosis
Cytological techniques
INTRODUCTION
Adenocarcinoma is the most common subtype of the primary pulmonary malignancy, of which the incidence and detection rates are increasing annually.[1] Adenocarcinoma is a heterogeneous disease with different morphological characteristics that are significantly correlated with different prognoses.[2] The 2015 World Health Organization and International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) recommended classifying lung adenocarcinoma into five major subtypes (namely, lepidic, acinar, solid, papillary, and micropapillary subtypes) according to the predominant morphological pattern in surgical specimens.[3,4] Approximately 70% of patients with the primary lung cancer do not undergo curative surgery and small biopsy specimens or cytological specimens may be the only tissue material available for diagnosis.[5]
The current recommendation for small biopsies and cytological specimens is to classify non-small-cell lung cancer into subtypes such as adenocarcinoma or squamous cell carcinoma.[6] Further subtype analysis of lung adenocarcinoma is mainly focused on small biopsy specimens.[7,8] Matsuzawa et al. showed that the consistency between small biopsy specimens and resected specimens was 37–88% for different subtypes.[9] However, subtyping of lung adenocarcinoma using cytology specimens is rarely reported. Whether cytology samples can be used for subclassification of lung adenocarcinoma and the cytological characteristics of different subtypes of lung adenocarcinoma remain unclear.
Previously, some scholars used a cytology grading system to predict the outcome of lung adenocarcinoma, providing a feasible basis for pulmonary adenocarcinoma classification based on cytology specimens.[10] Subsequently, Rodriguez et al. attempted to use cytological samples for subtype diagnosis and elucidated the cytomorphological characteristics of different subclassifications of lung adenocarcinoma.[11,12] Unfortunately, the authors only partially described the cytological characteristics of subtypes, with other subtypes such as the micropapillary subtype not included in the article at all. Chang et al. explicitly described the micropapillary pattern in cytology samples and discussed the differential diagnosis of pulmonary entities exhibiting similar morphologies.[13]
In this study, we summarize the cytological characteristics of different subtypes of lung adenocarcinoma based on relevant literature review. According to the summarized cytological features, cytology samples from 115 patients with lung adenocarcinoma confirmed by small biopsies were processed for subtyping classification. The diagnostic results of subtypes were analyzed and compared to those of small biopsy specimens to assess the feasibility of cytological subtype diagnosis.
MATERIAL AND METHODS
All the specimens and information were obtained from the Department of Pathology, Zhongda Hospital, School of Medicine, Southeast University. We retrieved 115 bronchial brushings from our database that was collected between January 1, 2016, and June 30, 2019, for which lung adenocarcinoma was confirmed by small biopsies. The sensitivity and specificity of diagnosis and recognition of malignant cells vary with different cytological techniques.[14-16] Canberk et al. and Chen et al.[17,18] demonstrated that bronchial brushing or bronchoalveolar lavage samples have higher specificity compared to fine-needle aspiration (FNA) smears; therefore, we chose bronchial brushing samples for malignant diagnosis of lung adenocarcinoma. All small biopsy specimens were stained with hematoxylin and eosin and grouped according to the IASLC/ATS/ERS classification, which was subdivided into the lepidic, acinar, papillary, micropapillary, and solid predominant pattern. All bronchial brushing samples were processed using the liquid-based cytology method by SurePath method (BD Biosciences, Franklin Lakes, NJ, USA) and were stained with Papanicolaou stain. Subsequently, cytological samples were subdivided into five subtypes including c-acinar, c-papillary, c-solid, c-lepidic, and c-micropapillary by evaluating the structure, atypical features, and background. All cytology specimens were classified and analyzed independently by three cytopathologists according to cytomorphologic features [Table 1]. For more effective application, an algorithmic approach to subclassification of lung adenocarcinoma is drawn in [Figure 1]. The cytopathologists were not aware of the previous diagnoses of the specimens. When the diagnosis was inconsistent in cytological subtyping of pulmonary adenocarcinoma, the case was reevaluated until a unified diagnosis was reached.
| Cytological characteristics | |||
|---|---|---|---|
| Subtyping of pulmonary adenocarcinoma | Architecture | Atypia | Background |
| c-Acinar | Two-dimensional or three-dimensional clusters with nuclei located around the glandular lumen | Moderate atypia Small to medium-large nuclei (approximately 3‒4 lymphocytes) Smooth nuclear membrane Slightly rough chromatin Small nucleoli | Usually clean |
| c-Papillary | Predominance of three-dimensional papillary clusters with fibrovascular cores | Moderate atypia Small to medium-large nuclei (approximately 3‒4 lymphocytes) Relatively smooth nuclear membrane and inconspicuous nucleoli Intranuclear inclusions and/or grooves | May show inflammation |
| c-Solid | Large complex, and rounded three-dimensional clusters without an acinar or papillary architecture | Severe atypia Nuclei sizes >5 lymphocytes with convoluted contours and coarse chromatin Prominent nucleoli | Evident necrosis or inflammation |
| c-Lepidic | Single tiled sheet | Mild atypia Small to medium-large nuclei Smooth nuclear membrane Relatively fine chromatin | Lack of necrosis or inflammation |
| c-Micropapillary | Clusters of small-sized cells with a three-dimensional structure | Mild atypia Small nuclei (approximately 1‒2 lymphocytes) with a high nuclear-cytoplasmic ratio Irregular nuclear membrane | Microcalcification resembling a psammoma body |
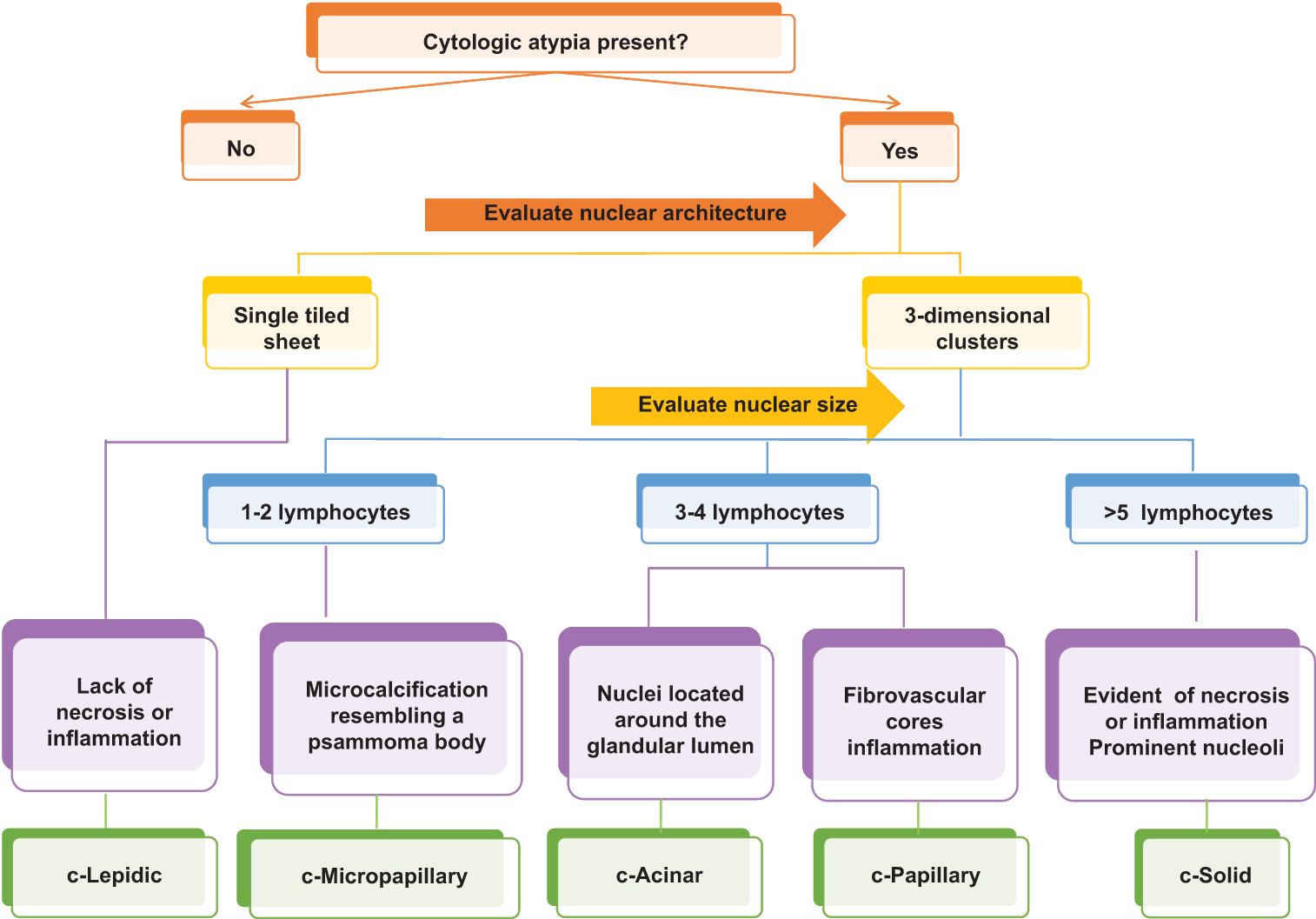
- Algorithmic approach to subclassification of lung adenocarcinoma applying cytomorphological features.
RESULTS
Of the 115 study patients, 64 were male and 51 were female (male-to-female ratio of 1.25–1). The median age of the patients was 67.3 years, ranging from 33 to 88 years. Fifty-five patients were current smokers or former smokers, and 60 patients had no history of smoking.
Among the 115 lung adenocarcinoma patients confirmed by small biopsy specimens, 62 cases (53.9%) had acinar predominant pattern, 16 cases (13.9%) had papillary predominant pattern, 29 cases (25.2%) had solid predominant pattern, three cases (2.6%) had lepidic predominant pattern, and five cases (4.3%) had micropapillary predominant pattern. We divided the cytological samples of corresponding matched patients into five different subcategories according to morphology. The best concordance rate with the small biopsy specimen was that for the c-acinar subtype (74.2%), followed by that for the c-lepidic subtype (66.7%), c-papillary subtype (56.3%), c-micropapillary subtype (40.0%), and c-solid subtype (24.1%). The overall cytology and small biopsy concordance rate was found to be approximately 57.4% [Table 2 and Figure 2].
| Cytological subtyping diagnosis | |||
|---|---|---|---|
| Histological subtyping | Number of patients | Consistency | Inconsistency |
| Acinar | 62 (53.9%) | 46 (74.2%) | 16 (25.8%) |
| Papillary | 16 (13.9%) | 9 (56.3%) | 7 (43.8%) |
| Solid | 29 (25.2%) | 7 (24.1%) | 22 (75.9%) |
| Lepidic | 3 (2.6%) | 2 (66.7%) | 1 (33.3%) |
| Micropapillary | 5 (4.3%) | 2 (40.0%) | 3 (60.0%) |
| Total | 115 (100%) | 66 (57.4%) | 49 (42.6%) |

- Cytomorphological and corresponding histological features of subcategories of pulmonary adenocarcinoma. (a) Clusters of cells arranged into a three-dimensional adenotubular structure with nuclei around the glandular lumen. Cells have moderate atypia, slightly rough chromatin, and smooth nuclear membrane with bronchial brushing, Pap (× 60). (b) Lung adenocarcinoma with acinar predominant pattern. Biopsy samples, HE (×40). (c) Predominance of three-dimensional papillary clusters with fibrovascular cores. Neoplastic cells showed moderate atypia and always had nuclear grooves. Bronchial brushing, Pap (×60). (d) Lung adenocarcinoma with papillary predominant pattern. Biopsy samples, HE (× 40). (e) Clusters of small-sized cells with three-dimensional structure and mild atypia. Tumor cells typically present as 1–2 lymphocytes with a high nuclear-cytoplasmic ratio and irregular nuclear membrane. Bronchial brushing, Pap (×60). (f) Lung adenocarcinoma with micropapillary predominant pattern. Biopsy samples, HE (×40). (g) Tumor cells are arranged in a single layer and can form a string of pearl-like structures with minimal nuclear atypia and a lack of necroinflammation in the background. Bronchial brushing, Pap (×60). (h) Lung adenocarcinoma with lepidic predominant pattern. Biopsy samples, HE (×40). (i) Large, complex, and rounded three-dimensional clusters of tumor cells with an irregular arrangement and pleomorphic nucleus. Neoplastic necrosis is often observed in the background. Bronchial brushing, Pap (×60). (j) Lung adenocarcinoma with solid predominant pattern. Biopsy samples, HE (×40).
We, further, compared the degree of subtyping diagnostic certainty of lung adenocarcinoma in the cytology samples versus the biopsy samples. Among the 115 patients, a high proportion of cases (69 cases) were classified as c-acinar subtype. The c-papillary and c-solid subtypes accounted for 23 and 18 cases, respectively, and were identified due to their prominent papillary structure and severe atypia. Due to their mild atypia and varying structural characteristics, three cases were classified as c-micropapillary type and two as c-lepidic type. As shown in [Table 3], in patients with lung adenocarcinoma, whose biopsy specimens were deemed as acinar dominant subtypes, cytological discordant cases also included the c-papillary subtype (seven cases) and c-solid subtype (five cases). In the papillary predominant pattern, incongruence was observed in four c-acinar cases, two c-solid cases, and one c-micropapillary case. In addition, the discordant cases of lung adenocarcinoma with a solid pattern were cytologically classified as c-acinar (n = 16) and c-papillary (n = 6), respectively. Of the three lepidic predominant cases, only one case was cytologically subclassified as c-acinar subtype.
| Histological subtyping | ||||||
|---|---|---|---|---|---|---|
| Cytological subtyping | Acinar | Papillary | Solid | Lepidic | Micropapillary | Total |
| c-Acinar | 46 | 4 | 16 | 1 | 2 | 69 |
| c-Papillary | 7 | 9 | 6 | - | 1 | 23 |
| c-Solid | 9 | 2 | 7 | - | - | 18 |
| c-Lepidic | - | - | - | 2 | - | 2 |
| c-Micropapillary | - | 1 | - | - | 2 | 3 |
| Total | 62 | 16 | 29 | 3 | 5 | 115 |
Although two cases of micropapillary-dominant lung adenocarcinoma were recognized based on cytology, there was some confusion when we initially encountered this subtype due to the extremely mild atypia observed. Cell blocks were prepared for the two samples of micropapillary-dominant lung adenocarcinoma, and well-prepared cell-blocks can provide the opportunity to examine the histological architecture of cytology material, as well as perform ancillary immunohistochemistry and gene tests.[19-21] Furthermore, immunohistochemistry analysis was performed to assist the diagnosis. The tumor cells were extremely small and only slightly larger than those of the normal bronchial epithelium. Small papillary clusters of glandular cells were observed and no fibrovascular cores were detected [Figure 3a]. The morphology of tumor cells in the cell block was essentially the same as that of cell liquid-based sections [Figure 3b]. Immunohistochemistry analysis showed that the tumor cell cytoplasm and nuclei were positively immunostained for cytokeratin 7 and thyroid transcription factor-1, respectively [Figure 3c and d].

- Cytomorphological features and immunohistochemical staining of c-micropapillary subcategories in pulmonary adenocarcinoma. (a) Cytological image (×60). (b) Cell block image (×60). (c) Cytokeratin 7-positive tumor cells (×20). (d) Thyroid transcription factor-1-positive tumor cells (×20).
Next, we calculated the sensitivity, specificity, positive, and negative predictive values of subtype analysis of lung adenocarcinoma using cytological samples. All statistical data are shown in [Table 4]. The results revealed that the sensitivity for detecting lung adenocarcinoma with different subtypes was 24.1–74.2%; the specificity of subtype analysis of lung adenocarcinoma was generally better when using cytological samples. The positive and negative predictive values of each subtype of lung adenocarcinoma were 39.1– 100% and 65.2–99.1%, respectively.
| Cytological subtyping | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| c-Acinar | 74.2% | 56.6% | 66.7% | 65.2% |
| c-Papillary | 56.3% | 85.6% | 39.1% | 92.4% |
| c-Solid | 24.1% | 87.2% | 38.9% | 77.3% |
| c-Lepidic | 66.7% | 100% | 100% | 99.1% |
| c-Micropapillary | 40% | 99.1% | 66.7% | 97.3% |
PPV: Positive predictive value, NPV: Negative predictive value
DISCUSSION
Different subtypes of lung adenocarcinoma are closely related to the prognosis of patients.[22,23] Prior studies have attempted to subdivide different patterns of lung adenocarcinoma on the basis of cytology specimens, which was quite difficult using cytology samples in most studies. Some scholars suggested that cytology samples cannot be used to obtain reliable and accurate diagnosis results in lung adenocarcinoma subclassification.[11,24,25] However, in 2015, Rodriguez et al.[12] described the cytological characteristics of some lung adenocarcinoma subtypes in detail and concluded that the architectural and nuclear features of cytology samples may be helpful, particularly for distinguishing prognostically adverse solid patterns from other patterns. A similar study by Nambirajan et al. demonstrated that using nuclear grade scoring may enhance the application value of cytology samples in subclassifying lung adenocarcinoma.[26]
These studies above-mentioned strongly suggested that cytological samples can be used to subtype lung adenocarcinoma. We evaluated the cytological subtypes of lung adenocarcinoma mainly by comprehensive judgment of structural characteristics, cell atypia, and the background. In this study, we found that acinar-predominant tumors have an excellent cytologic-histologic correlation compared to tumors with a predominant solid pattern. Rudomina et al. reported similar results.[27] However, these results are inconsistent with those of Rodriguez et al.[12] and Nambirajan et al.,[26] suggesting that the cytological and histological consistency of solid subtypes was superior to that of other subtypes in diagnosing lung adenocarcinoma subtypes. This difference may be partly related to the different methods of cell preparation. Liquid-based cytology eliminates the inflammatory necrosis background material and better preserves the three-dimensional structure of the cell mass.[28] This may have influenced the cytology subtyping of lung adenocarcinoma. In contrast, the acinar structure may be relatively easy to identify microscopically.[11]
In our study, the coincidence rate of lepidic and papillary patterns was also improved compared to the previous observations.[11,26] The cytomorphology of the lepidic subtype has been described as uniform cells with bland nuclei; the papillary pattern has been defined as complex branching structures with a fibrous vascular core. We hypothesized that these structures are likely to be preserved in liquid-based films, which may explain the improved concordance rate.
We detected inconsistencies in the c-micropapillary subtype between poor prognosis and mild cytologic atypia. Due to the low incidence of this subtype of lung adenocarcinoma and lack of definite morphological diagnostic criteria, few studies have described this subtype.[12,26] Through literature review,[13,27] we summarized the cytological characteristics of the c-micropapillary subtype of lung adenocarcinoma and performed immunohistochemical diagnosis. The existence of small micropapillary-like tufts in cytology specimens was not considered as an evidence of the c-micropapillary subtype by Rudomina et al.[27] However, our data showed that although the sensitivity in identifying the c-micropapillary subtype was very poor, the diagnostic specificity can reach as high as 99.1%. Micropapillary pattern adenocarcinoma with intermediate and high-grade cytological atypia are easily identified, whereas micropapillary pattern adenocarcinoma with mild cytological atypia are often misdiagnosed as benign lesions. The cytological morphology of seven cases of lung adenocarcinoma with micropapillary subtype reported by Tanaka et al. was almost all well differentiated.[29] Hence, accurate recognition of mild atypia is essential as it is correlated to poor prognosis. Although the results do not exactly correspond to the micropapillary subtype of lung adenocarcinoma, our findings will aid accurate recognition of mild atypia.
Our study had some limitations. The subjects selected in this study all had advanced disease and their tumors could not be resected. All studies were based on small biopsy specimens and corresponding matched cytological specimens. Due to the heterogeneity of tumors, more than 75% of lung adenocarcinoma are considered mixed subtypes.[30] Thus, we cannot guarantee that the biopsy will be in the same location as the brush, and it is not reliable to determine whether cytological samples can be used for subtype analysis only by comparing the coincidence rate of the two methods. Some patients may be in the advanced stage during clinical studies and cannot undergo surgical resection; thus, small biopsy and/or cytology samples are the only tissue available for subtype classification. For these patients, using cytology samples for subtype, diagnosis may be particularly important. In addition, some lung adenocarcinoma subtypes, such as the lepidic pattern, were limited by the number of cases, and thus, the sensitivity and specificity data may not fully reflect the normal characteristics of these subtypes. In our future study, we will continue to collect data for these subtypes to obtain more accurate results.
At present, there are no established unified cytomorphologic criteria for subclassifying lung adenocarcinoma based on cytology. Our research was based on the previous reports and our own experience, and thus, further studies are needed. Using cytological materials to diagnose, lung adenocarcinoma subtypes remain challenging and controversial. Cytological samples are not recommended for subtype diagnosis when other types of samples are available. The present study demonstrated that understanding the cytological characteristics of each subtype of lung adenocarcinoma may contribute to the identification of the mild atypical subtype (micropapillary pattern), which is closely related to a poor prognosis. We will, further, determine an accurate and complete cytology subtype diagnosis for lung adenocarcinoma.
SUMMARY
Cytology specimens is a valuable, accurate, and reliable tool in diagnosing pulmonary adenocarcinoma. Although it is relatively difficult to use cytological materials alone for accurate subtype analysis of lung adenocarcinoma, familiarity with its morphological characteristics will help us to improve our own diagnostic level and minimize the missed diagnosis of the mild atypical subtype.
DATA AVAILABILITY STATEMENT
All relevant data are within the paper.
ACKNOWLEDGMENTS
We thank Jinjun Nie and Yueyue Hao for help with cytological samples evaluation and the slides review.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
The authors declare that no competing interest exist.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Cao Ma collected, analyzed the data and drafted the original manuscript. Lihua Zhang designed the study and revised the manuscript.
ETHICS STATEMENT BY ALL AUTHORS
This retrospective study was carried out in the department of Pathology, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, Jiangsu, China. Patient consent was taken during the EUS guided bronchial brushings. The study was approved in accordance with ethical standards and regulations, the Declaration of Helsinki, and national and international guidelines.
LIST OF ABBREVIATIONS (In alphabetic order)
ATS - American Thoracic Society
ERS - European Respiratory Society.
FNA - Fine-needle aspiration
IASLC - International Association for the Study of Lung Cancer
EDITORIAL/PEERREVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
References
- Inaccuracy of lung adenocarcinoma subtyping using preoperative biopsy specimens. J Thorac Cardiovasc Surg. 2017;154:332-9.e1.
- [Google Scholar]
- A grading system of lung adenocarcinomas based on histologic pattern is predictive of disease recurrence in stage I tumors. Am J Surg Pathol. 2010;34:1155-62.
- [Google Scholar]
- The 2015 world health organization classification of lung tumors: Impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015;10:1243-60.
- [Google Scholar]
- International association for the study of lung cancer/American thoracic society/European respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6:244-85.
- [Google Scholar]
- Napsin A/p40 antibody cocktail for subtyping non-small cell lung carcinoma on cytology and small biopsy specimens. Cancer Cytopathol. 2016;124:472-84.
- [Google Scholar]
- Diagnosis of lung cancer in small biopsies and cytology: Implications of the 2011 International association for the study of lung cancer/American thoracic society/European respiratory society classification. Arch Pathol Lab Med. 2013;137:668-84.
- [Google Scholar]
- Subtype classification of lung adenocarcinoma predicts benefit from adjuvant chemotherapy in patients undergoing complete resection. J Clin Oncol. 2015;33:3439-46.
- [Google Scholar]
- Can IASLC/ATS/ERS subtype help predict response to chemotherapy in small biopsies of advanced lung adenocarcinoma? Eur Respir J. 2014;43:1240-2.
- [Google Scholar]
- Factors influencing the concordance of histological subtype diagnosis from biopsy and resected specimens of lung adenocarcinoma. Lung Cancer. 2016;94:1-6.
- [Google Scholar]
- Predicting pulmonary adenocarcinoma outcome based on a cytology grading system. Cancer Cytopathol. 2012;120:35-43.
- [Google Scholar]
- Cytologic subtyping of lung adenocarcinoma by using the proposed international association for the study of lung cancer/American thoracic society/European respiratory society (IASLC/ATS/ ERS) adenocarcinoma classification. Cancer Cytopathol. 2013;119:629-37.
- [Google Scholar]
- Cytopathology of pulmonary adenocarcinoma with a single histological pattern using the proposed international association for the study of lung cancer/American thoracic society/European respiratory society (IASLC/ATS/ ERS) classification. Cancer Cytopathol. 2015;123:306-17.
- [Google Scholar]
- Cytodiagnostic aspects of lung adenocarcinoma manifesting with micropapillary pattern in sputum: A case report of potential diagnostic pitfall. Diagn Cytopathol. 2014;42:902-5.
- [Google Scholar]
- Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e142S-65S.
- [Google Scholar]
- Committee I: Indications for pulmonary cytology sampling methods. Diagn Cytopathol. 2016;44:1010-23.
- [Google Scholar]
- Comparative assessment of the diagnostic value of transbronchial lung biopsy and bronchoalveolar lavage fluid cytology in lung cancer. Asian Pac J Cancer Prev. 2015;16:201-4.
- [Google Scholar]
- The new guidelines of Papanicolaou society of cytopathology for respiratory specimens: Assessment of risk of malignancy and diagnostic yield in different cytological modalities. Diagn Cytopathol. 2018;46:725-9.
- [Google Scholar]
- Evaluation of the diagnostic accuracy of bronchial brushing cytology in lung cancer: A meta-analysis. Cancer Cytopathol. 2021;129:739-49.
- [Google Scholar]
- Cellblockistry: Chemistry and art of cell-block making-a detailed review of various historical options with recent advances. Cytojournal. 2019;16:20.
- [Google Scholar]
- CellBlockistry 101 In: CytoJournal Monograph (CMAS #1) (1st ed). United States of America: Cytopathology Foundation Inc; 2021.
- [Google Scholar]
- The utility of the proposed IASLC/ATS/ ERS lung adenocarcinoma subtypes for disease prognosis and correlation of driver gene alterations. Lung Cancer. 2013;81:371-6.
- [Google Scholar]
- Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: Prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol. 2011;24:653-64.
- [Google Scholar]
- Cytological cell blocks: Predictors of squamous cell carcinoma and adenocarcinoma subtypes. Diagn Cytopathol. 2012;40:380-7.
- [Google Scholar]
- Subtyping of pulmonary adenocarcinoma in cytologic specimens: The next challenge. Cancer Cytopathol. 2013;121:601-4.
- [Google Scholar]
- Adenocarcinoma predominant pattern subtyping and nuclear grading in cytology: Is there a role in prognostication of advanced pulmonary adenocarcinomas? Cytopathology. 2018;29:163-71.
- [Google Scholar]
- Cytologic diagnosis of pulmonary adenocarcinoma with micropapillary pattern: Does it correlate with the histologic findings? Diagn Cytopathol. 2009;37:333-9.
- [Google Scholar]
- Comparison of liquid-based preparation and conventional smear of fine-needle aspiration cytology of lymph node. J Cytol. 2016;33:187-91.
- [Google Scholar]
- Cytomorphometric and flow cytometric analyses using liquid-based cytology materials in subtypes of lung adenocarcinoma. Diagn Cytopathol. 2022;50:394-403.
- [Google Scholar]
- Clinicopathological predictors of EGFR/KRAS mutational status in primary lung adenocarcinomas. Mod Pathol. 2010;23:159-68.
- [Google Scholar]








