Translate this page into:
A case of S-100 negative melanoma: A diagnostic pitfall in the workup of a poorly differentiated metastatic tumor of unknown origin
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
When confronted with a metastatic poorly differentiated tumor of unknown origin, the initial workup includes the standard panel of immunostains to rule out carcinoma, sarcoma, lymphoma, and the greatest mimicker in pathology – malignant melanoma. Although not specific, the S-100 protein is expressed in over 95% of malignant melanomas. Herein, we present a case of multiorgan metastatic malignancy with a dominant hilar and mediastinal mass in a current smoker; clinically, highly suggestive of widespread primary lung cancer. This case was eventually classified as malignant melanoma, despite a significant diagnostic challenge due to lack of prior history, unusual cytomorphology, and S-100 protein negativity. A battery of immunostains was performed and the addition of other melanocytic-associated markers confirmed the melanocytic lineage of the neoplasm. This case highlights the pitfalls in the differential diagnosis of a metastatic tumor of unknown origin by fine needle aspiration cytology due to the significant morphologic overlap of poorly differentiated malignancies. We emphasize that, albeit rare, malignant melanomas can be completely negative for S-100 protein and the use of additional melanocytic-associated markers in the differential workup maybe critical in arriving promptly at a proper diagnosis. We also briefly discuss other currently available immunohistochemical markers that can assist in the identification of the S-100 negative melanoma.
Keywords
Malignant melanoma
melanocytic-associated markers
poorly differentiated metastatic tumor of unknown origin
S-100
INTRODUCTION
Although the majority of cancer patients present with an obvious primary tumor, the initial presentation of 10–15% of patients is widespread metastatic disease with an unknown primary tumor. Fine needle aspiration cytology (FNAC) with image guidance is the frontrunner in the evaluation of masses in the most common metastatic sites of the human body such as liver, lung, and lymph nodes.[123] A stepwise approach to the diagnosis of metastases of unknown primary tumor employs a combination of clinical context, morphology, immunohistochemistry (IHC), and molecular studies.[4]
The importance of clinical history and imaging studies cannot be overemphasized when interpreting cytologic specimens; however, the clinical picture is often nonspecific in advanced stage disease.[5] Establishing a diagnosis of malignancy is usually straightforward in an adequate fine needle aspiration sample, but further classification maybe difficult unless hallmark cytologic features are present in well-differentiated tumors. Pure morphologic assessment is usually limited, and ancillary testing by IHC is often needed to better characterize cancer cells.[5]
In cases of poorly differentiated malignancies, in which the lineage of cancer cells is difficult to establish by morphology alone, the first-line IHC panel aims on broad tumor typing as carcinoma, melanoma, lymphoma, or sarcoma. Although not specific, S-100 immunostain labels almost all melanomas with a strong and diffuse staining; hence, it is commonly used in the first-line IHC panel along with an epithelial marker (e.g., pancytokeratin), and a lymphoid marker (e.g. [leukocyte common antigen (LCA)]).[6] Positivity with any one of these markers generally leads to a second IHC panel to provide further subtyping and to predict the primary tumor site. Negativity with the first-line panel raises the possibility of rarer tumors including sarcomas, germ cell tumors, or LCA-negative hematolymphoid tumors with additional workup being necessary to reach a final diagnosis.[45]
Here, we present a case of the S-100 negative amelanotic melanoma to emphasize the use of other melanocytic-associated markers early in the diagnostic workup of poorly differentiated metastatic tumor of unknown origin.
CASE REPORT
Clinical presentation and imaging studies
A 52-year-old woman, a current smoker without significant past medical history, presented with nonspecific symptoms of lethargy, involuntary weight loss, nausea, and new onset headaches. She also noticed several painful lumps on her skin in the epigastrium and her breasts. There was no known prior diagnosis of malignancy. Physical examination revealed moderate thoracic expansion with wheezing and multiple tender subcutaneous nodules on her left breast, left thorax, subxiphoid, and abdomen. Positron emission tomography-computed tomography showed a large hypermetabolic right hilar and mediastinal mass measuring 6.6 cm × 5.4 cm which severely narrowed the right bronchus intermedius. Hypermetabolic adenopathy was present in the chest, abdomen, and pelvis. Numerous distant metastases in the lungs and intraperitoneal cavity as well as a solitary hepatic metastasis were visualized. Several superficial hypermetabolic soft tissue densities were seen including subcutis overlying the upper abdomen and left anterolateral chest wall [Figure 1]. Magnetic resonance imaging of the brain showed multiple enhancing lesions within the supratentorial compartment that likely represented metastatic disease, as well as an enhancement in both frontal lobes raising the possibility of early leptomeningeal spread. Overall, the clinical picture and radiologic impression were suspicious for metastatic lung cancer. The patient underwent unassisted fine needle aspiration biopsy of an easily accessible and palpable subcutaneous nodule above the umbilicus.
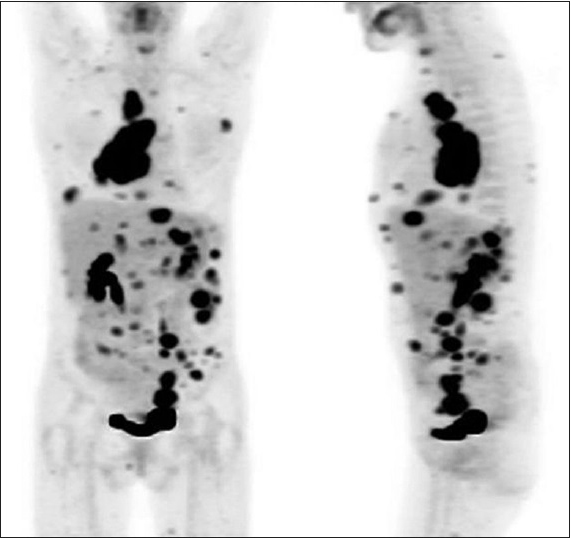
- Skull base to mid-thigh positron emission tomography-computed tomography, following intravenous injection of 18-fluoro-2-deoxyglucose. Multifocal hypermetabolic foci consistent with a metastatic malignancy with largest mass located in the thorax. (For improved resolution with enlargement of all images, please refer to the digital/online version of the article)
Specimen processing
A telepathology was used for an immediate adequacy assessment of cytology specimen. All needle passes were rinsed in CytoRich Red solution and processed overnight using cell button technique into Formalin-fixed, paraffin-embedded cell block preparation. Hematoxylin and eosin staining and IHC studies were performed on 4-μm thick tissue sections. IHC was run using automated methodology (Leica Bond; Leica Microsystems, Bannockburn, IL, USA). Standardized IHC protocols were followed with control slides as appropriate. Specifically, for S-100 IHC tissue sections were incubated with a rabbit polyclonal antibody to S-100 protein subunit beta (DAKO, Denmark, Z0311) at dilution of 1:400 for 15 min.
Cytologic findings
The Diff-Quik stained smears showed increased cellularity with a prominent cell dissociation pattern as well as malignant cells arranged in clusters. The cell groups displayed a syncytial growth pattern with poorly defined cell borders. The individual cells showed irregular nuclear borders and scant cytoplasm. There were mitotic figures and abundant tumor necrosis. Papanicolaou-stained slides highlighted coarse chromatin and occasional conspicuous nucleoli. No pigment or intranuclear inclusions were seen [Figure 2].
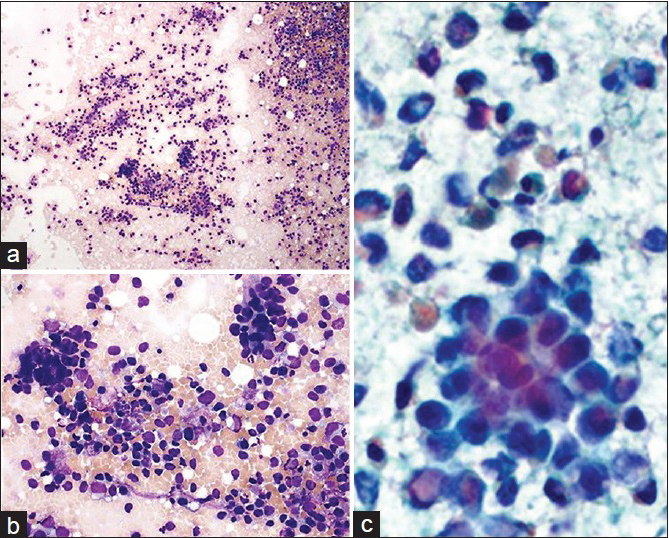
- Cytological preparations; Diff-Quik (a and b) and Papanicolaou (c) stained fine needle aspiration smears. (a) Hypercellular specimen; loosely dispersed malignant cells and occasional tumor clusters (×200). (b) Single and clustered tumor cells with marked anisonucleosis and poorly defined cell borders (×400). (c) Prominent cell dissociation and background necrosis. Hyperchromatic nuclei with irregular borders, coarse chromatin, and scant cytoplasm (×400, digitally magnified). (For improved resolution with enlargement of all images, please refer to the digital/online version of the article)
Histologic and immunohistochemical findings
Hematoxylin and eosin-stained cell block preparation showed malignant cells clustered and dispersed as single cells in the background of necrosis. The tumor clusters appear loosely cohesive with poor cell-to-cell adhesion. A radiating growth pattern surrounding the blood vessels and adipose tissue infiltration were noted. The malignant cells displayed high nucleus-to-cytoplasmic ratio, coarse chromatin pattern, occasional conspicuous nucleoli, irregular nuclear contours, and scant eosinophilic cytoplasm. Mitotic figures and apoptotic bodies were identified [Figure 3]. The cell block sections were initially studied for CKAE1/3, CK7, CK20, TTF-1, p40, S-100, synaptophysin, and LCA that all yielded negative results [Figure 4]. The second round of immunostains included CK5, CK5D3, GATA-3, BRST-2, ER, PR, PAX-8, WT-1, calretinin, CD3, CD20, CDX-2, and SMAD4 were also negative; SMAD4 showed nuclear staining (no loss of protein expression). The third round of stains comprised desmin, CD34, STAT-6, SOX-10, microphthalmia transcription factor (MITF), Melan-A, HMB-45, and INI-1. The lesional cells were immunoreactive with SOX-10, MITF, Melan-A, and HMB-45 and were negative for desmin, CD34, STAT-6, without INI-1 loss [Figure 5].
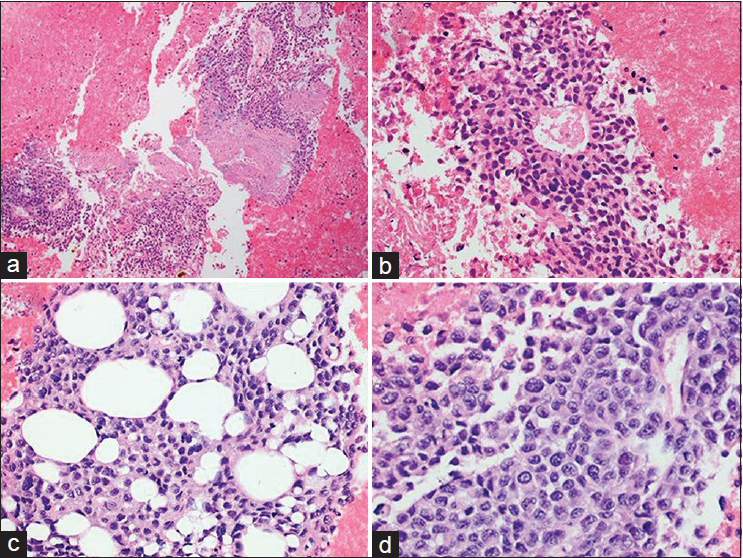
- Cell block preparation (H and E) (a). Loosely cohesive clusters of malignant cells and background of necrosis (×200) (b). Radiating growth pattern around blood vessels and poor cell-to-cell adhesion (×400) (c). Adipose tissue infiltration by tumor cells (×400) (d). High N/C ratio, coarse chromatin pattern, irregular nuclear contours, occasional conspicuous nucleoli, and scant eosinophilic cytoplasm (×400, digitally magnified). (For improved resolution with enlargement of all images, please refer to the digital/online version of the article)
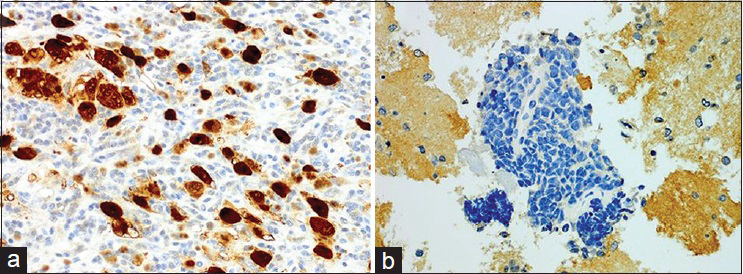
- S-100 protein expression (immunohistochemistry). (a) Positive control, strong and diffuse immunoreactivity with S-100 antibody. (b) Negative S-100 immunostaining in the current case (both × 400, digitally magnified). (For improved resolution with enlargement of all images, please refer to the digital/online version of the article)
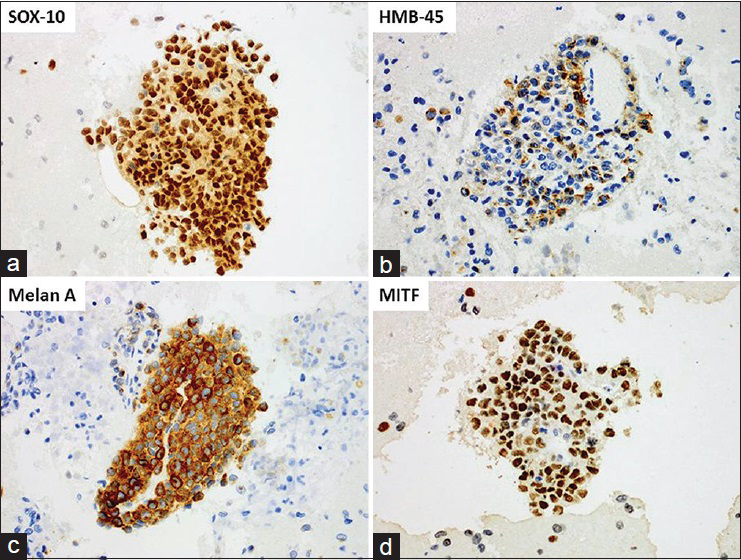
- Expression of other melanocytic-associated markers (immunohistochemistry). Positive immunostaining for: (a) SOX-10, nuclear (b) HMB-45, cytoplasmic, finely granular (c) Melan-A, cytoplasmic, diffuse (d). Microphthalmia transcription factor, nuclear (all × 400, digitally magnified). (For improved resolution with enlargement of all images, please refer to the digital/online version of the article)
Molecular studies
Genomic DNA extracted from formalin-fixed paraffin-embedded cell block sections was subjected for somatic mutation analysis in a 50 gene panel. An amino acid substitution at position 600 from valine (V) to a lysine (K) was detected in the BRAF gene (V600K). In addition, a mutation of unknown clinical significance was found in the MET gene. The tumor cells were normal for c-KIT, GNAQ, NRAS, CTNNB1, and hotspots in 44 other genes.[7]
Follow-up
The patient was diagnosed with malignant melanoma with brain, lungs, liver, chest, retroperitoneal, intra-abdominal lymph nodes, and subcutaneous metastases. She completed whole brain radiation therapy for the central nervous system metastatic disease. She subsequently received a targeted therapy for a BRAF V600E/K-mutant metastatic melanoma with the BRAF inhibitor combined with the MEK inhibitor and cancer immunotherapy targeting programmed cell death 1 receptor. The patient is currently alive 5 months after the diagnosis, and clinically, her symptoms have improved.
DISCUSSION
Malignant melanoma is one of the greatest mimickers in pathology owing to its inherent variation in its histological patterns. Although histologic examination of the surgical biopsies plays a major role in the diagnosis of primary cutaneous melanomas, FNAC is widely employed to confirm metastatic or recurrent lesions, with a sensitivity and specificity of 96.3% and 98.9%, respectively.[123] Despite the considerable current knowledge on the cytomorphology of melanoma, a cytologic diagnosis is often difficult, especially with amelanotic lesions. The hallmark cytomorphologic features include high cell - yield with a predominant population of dissociated cells with plasmacytoid, polygonal or spindle cells, nuclear pleomorphism, prominent nucleoli, intranuclear cytoplasmic inclusions, and a variable number of bi- and multinucleated cells. Nevertheless, melanoma may display features common to any of other malignant lesions such as an increase in nuclear-to-cytoplasmic ratio, irregular nuclear outlines, or coarse chromatin and can therefore be indistinguishable from other poorly differentiated tumors. In cytologic samples obtained by fine needle aspiration, melanoma may appear in more cohesive clusters mimicking carcinoma;[8] but melanoma cells tend to grow in syncytial sheets with poorly defined cell borders in contrast to well-defined cells in the tridimensional groups that characterize carcinomas.[123]
The diagnosis of metastatic melanoma is further complicated by its ability to metastasize to any site with metastases occurring during any time interval from a primary diagnosis. Although metastases may present in unusual locations, generally they initially involve regional lymph nodes with the development of distant metastases occurring later. The most often affected sites include the skin, lungs, liver, brain, and bone; however a wide variety of other locations including the adrenals, kidney, omentum, pancreas, parotid, soft tissue, breast, and thyroid have been reported. Metastatic spread of malignant melanoma to the skin is common and ranges from satellitosis to in-transit regional metastases.[9]
When evaluating a new mass lesion in patients with a known prior history of malignant melanoma, the differential diagnosis is already narrowed, and a panel focused to include melanocytic-associated markers is usually being applied up front in a diagnostic workup. In addition, a comparison of cytomorphology and immunoprofile of metastatic to a primary tumor usually reveal similarities and facilitate the diagnosis.[9]
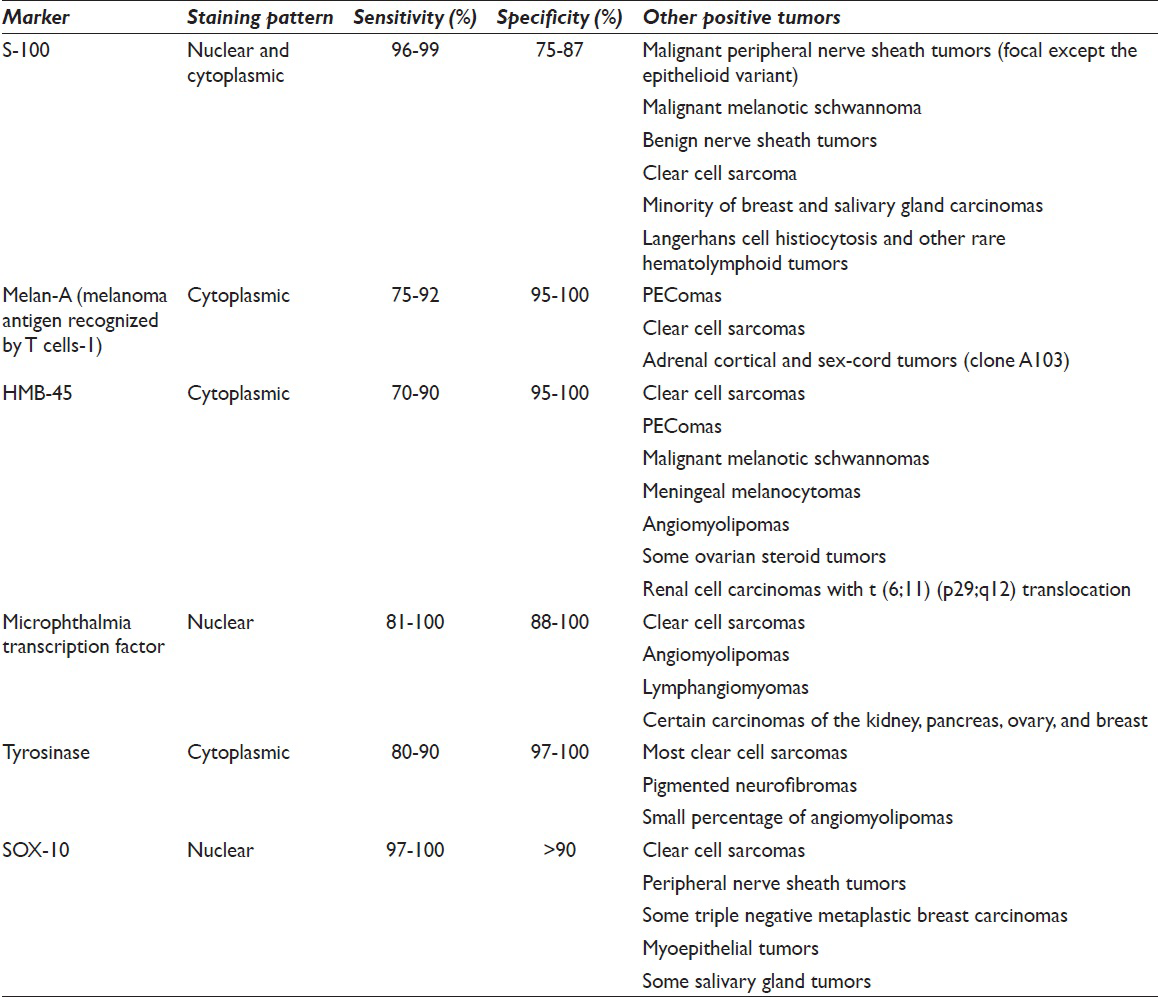
A much more challenging scenario is one where the patient initially presents with metastasis from an unknown primary site. In the absence of a known history or striking cytomorphologic features of melanoma, accurate diagnosis is difficult and always requires a battery of immunostains. Negative workup for carcinoma, lymphoma, and sarcoma coupled with a positive melanoma marker allows prompt and proper triage of the patient's sample and further workup to confirm melanoma. The most useful positive markers for melanoma include S-100, Melan-A/melanoma antigen recognized by T cells-1 (MART-1), and HMB-45 as well as the newly emerging melanoma markers, such as SOX-10, MITF, and tyrosinase[101112] [Table 1].
S-100, named for its solubility in 100% saturated ammonium sulfate solution, belongs to a family of low-molecular-weight calcium-binding proteins[13] involved in the regulation of diverse cellular functions.[14] Aside from the diagnostic importance of S-100 protein expression, its relationship with melanoma pathogenesis is unclear.[15]
The S-100 stains almost all melanomas variants, usually with strong, diffuse nuclear and cytoplasmic staining.[6] Therefore, S-100 immunostain is highly sensitive with an immunoreactivity of approximately 96–99% and is used as a first-line melanocytic marker to evaluate poorly differentiated malignant tumors. However, in up to 4% of metastatic melanomas, the S-100 immunostain is negative.[16] Interestingly, S-100 negative melanoma metastases have been described in cases where the primary tumor was positive, indicating a possible link between tumor progression and loss of immunoreactivity for S-100.[17] Moreover, the overall proportion of S-100 negative melanomas is disproportionately high in ocular melanoma. This phenotype may reflect inherent differences in uveal versus cutaneous melanocytes.[18]
There are many variables affecting the quality of IHC staining. Some biomarkers have been affected differently by the use of different fixatives.[19] The loss of S-100 expression in tissue fixed in alcohol compared with the same tissue fixed in formalin has been reported, resulting in false negative results. While 10% neutral buffered formalin is a preferred fixative for S-100 immunostaining, cytology specimens in many laboratories including our own are fixed in alcohol-based fixative media. Use of such media is acceptable if appropriate validation studies have been performed. In our laboratory, we follow a validated S-100 IHC protocol for alcohol fixed samples that skips an antigen retrieval step. In fact, we have never encountered S-100 negative melanoma cytology in our institution since implementation of this staining technique.
Although very sensitive, S-100 protein is not specific to melanoma as it also stains most peripheral nerve sheath tumors (albeit focal except the epithelioid variant) and some other sarcomas, as well as a minority of breast and salivary gland carcinomas, Langerhans cell histiocytosis, and other rare hematolymphoid tumors. Its specificity is therefore lower and estimated at approximately 75–87%.[1011]
All other melanoma markers are less sensitive but more specific; hence, they not only stain fewer melanomas but also stain fewer nonmelanoma malignancies.[20]
Melanoma-specific protein: Clone A103, referred to as Melan-A, and clone M2-7C10, referred to as MART-1, both yield cytoplasmic staining and are positive in 75–92% of melanomas, including almost all epithelioid melanomas, but are usually absent in desmoplastic melanomas. Melanoma-specific proteins have a high specificity of 95–100% and show essentially no staining in most carcinomas or lymphomas; however, they may be expressed in PEComas and clear cell sarcomas. In addition, clone A103 also stains adrenal cortical and sex-cord tumors.[101112]
The antihuman melanosome antibody, HMB-45, which detects a cytoplasmic glycoprotein GP100, is present in immature melanosomes and therefore indicates active melanosome formation and melanocytic differentiation. The sensitivity of HMB-45 is similar to Melan-A/MART-1 as the staining is usually lacking in desmoplastic melanoma. The staining is absent from carcinomas or lymphomas, adrenal or otherwise; yet clear cell sarcomas, PEComas, melanocytic schwannomas, meningeal melanocytomas, angiomyolipomas, some ovarian steroid tumors, and renal cell carcinomas with the t (6;11) (p29;q12) translocation express this marker.[101112]
MITF is a nuclear protein regulating melanocyte development. The sensitivity of MITF is 81–100% and it is expressed in most melanoma subtypes including desmoplastic melanoma. Its specificity is low because it is present in a wide variety of neoplasms, especially spindle cell mesenchymal and lymphoid neoplasms, as well as in some carcinomas.[101121]
Tyrosinase is an emerging melanoma marker. It is a cytoplasmic enzyme along the pathway of melanin production. Approximately, 80–90% of melanomas express this marker; however, only a small percentage (~6%) of desmoplastic melanomas is positive. The specificity of tyrosinase is high (97–100%) although most clear cell sarcomas, pigmented neurofibromas, and a small percentage of angiomyolipomas (~20%) also express this marker.[101112]
SOX-10, also known as sex determinant region Y box 10, belongs to a family of transcription factors essential for peripheral nervous system development and the formation of melanocytes. SOX-10 is one of the most recent markers that has been recognized as being useful in the diagnosis of melanoma.[22] Although the number of studies of this marker is limited, they indicate a high sensitivity of 97–100% for both primary and metastatic melanomas. It is expressed in all melanoma subtypes including desmoplastic melanomas and produces a nuclear staining pattern. It is also positive in clear cell sarcomas, peripheral nerve sheath tumors, some triple negative metaplastic breast carcinomas, myoepithelial tumors, and some salivary gland tumors.[1011]
CONCLUSION
Melanomas are known for their propensity to metastasize to any organ and exhibit diverse cytomorphologic features, and can present with metastasis after regression at the primary site. Therefore, melanoma should always be in the differential diagnosis of metastatic lesions.[12323]
IHC is the most useful ancillary test used in the classification of poorly differentiated malignancies. The initial panel of immunostains should cover a broad spectrum of markers in an effort to establish cell lineage (epithelial, mesenchymal, lymphoid, and melanocytic). The immunomarkers for melanoma include S-100, HMB-45, Melan-A, MITF, tyrosinase, and SOX-10. Although S-100 is the least specific marker, it is of great practical importance because it exhibits the highest sensitivity. The S-100 negative melanomas occur in up to 4% of cases and present a diagnostic pitfall as was demonstrated by this case. We emphasize that in a case of metastatic high-grade malignancy with S-100 negativity, negative IHC workup for carcinoma, lymphoma, sarcoma and the absence of a known prior history, S-100 negative melanoma should be included in the differential diagnosis, and further workup with more specific melanocytic markers should be employed.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE, http://www.icmje.org/#author.
Each author has participated sufficiently in the work. AB, KL, and XL provided substantial contributions to conception and design; AB and KL drafted the manuscript and provided the images. KL, PD, AAS, VP, and XL revised it critically for important intellectual content. All authors read and approved the final version to be published.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from the Institutional Review Board (or its equivalent).
LIST OF ABBREVIATIONS (In alphabetic order)
FNAC - Fine Needle Aspiration Cytology
IHC - Immunohistochemistry
LCA - Leukocyte Common Antigen
MITF - Microphthalmia Transcription Factor
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through automatic online system.
ACKNOWLEDGMENTS
We would like to acknowledge Zahra Shajani Yi, who critically proofread the article.
REFERENCES
- Fine-needle aspiration cytology for the diagnosis of metastatic melanoma: Systematic review and meta-analysis. Am J Clin Pathol. 2013;140:635-42.
- [Google Scholar]
- Diagnosis of metastatic melanoma by fine-needle biopsy: Analysis of 2,204 cases. Am J Clin Pathol. 2007;127:385-97.
- [Google Scholar]
- Fine needle aspiration in the diagnosis of metastatic melanoma. J Am Acad Dermatol. 2000;42(5 Pt 1):735-40.
- [Google Scholar]
- Diagnosis of metastatic neoplasms: A clinicopathologic and morphologic approach. Arch Pathol Lab Med. 2010;134:194-206.
- [Google Scholar]
- Routine use of the Ion Torrent AmpliSeq™ Cancer Hotspot Panel for identification of clinically actionable somatic mutations. Clin Chem Lab Med. 2014;52:707-14.
- [Google Scholar]
- Cytopathology of malignant melanoma in conventional and liquid-based smears. Am J Clin Pathol. 2002;118:435-41.
- [Google Scholar]
- Progress in melanoma histopathology and diagnosis. Hematol Oncol Clin North Am. 2009;23:467-80. viii
- [Google Scholar]
- Value of melanocytic-associated immunohistochemical markers in the diagnosis of malignant melanoma: A review and update. Hum Pathol. 2014;45:191-205.
- [Google Scholar]
- Expression of gp100, MART-1, tyrosinase, and S100 in paraffin-embedded primary melanomas and locoregional, lymph node, and visceral metastases: Implications for diagnosis and immunotherapy. A study conducted by the EORTC Melanoma Cooperative Group. J Pathol. 2001;193:13-20.
- [Google Scholar]
- A soluble protein characteristic of the nervous system. Biochem Biophys Res Commun. 1965;19:739-44.
- [Google Scholar]
- Calcium-dependent and -independent interactions of the S100 protein family. Biochem J. 2006;396:201-14.
- [Google Scholar]
- Inhibiting S100B restores p53 levels in primary malignant melanoma cancer cells. J Biol Chem. 2004;279:34071-7.
- [Google Scholar]
- S-100 protein-negative malignant melanoma: Fact or fiction? A light-microscopic and immunohistochemical study. Am J Dermatopathol. 1994;16:233-40.
- [Google Scholar]
- S100 immunophenotypes of uveal melanomas. Invest Ophthalmol Vis Sci. 1990;31:1492-6.
- [Google Scholar]
- Application of alternative fixatives to formalin in diagnostic pathology. Eur J Histochem. 2012;56:e12.
- [Google Scholar]
- Comparison of five antibodies as markers in the diagnosis of melanoma in cytologic preparations. Am J Clin Pathol. 2002;118:930-6.
- [Google Scholar]
- Diagnostic utility of microphthalmia transcription factor in malignant melanoma and other tumors. Adv Anat Pathol. 2001;8:273-5.
- [Google Scholar]
- A newly developed mouse monoclonal SOX10 antibody is a highly sensitive and specific marker for malignant melanoma, including spindle cell and desmoplastic melanomas. Arch Pathol Lab Med. 2015;139:530-6.
- [Google Scholar]
- Fine-needle biopsy of metastatic melanoma: Clinical use and new applications. Lancet Oncol. 2010;11:391-400.
- [Google Scholar]








