Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
Lymph Node / Hematopoietic
107: The cytomorphological and clinicopathological spectrum of pleuropulmonary extranodal marginal zone lymphoma
Hyang Mi Ko, MD, PhD, Gilda da Cunha Santos, MD, PhD, FRCPC, Scott Boerner, MD, FRCPC, Denis Bailey, MD, PhD, FRCPC, William Geddie, MD, FRCPC
Laboratory Medicine and Pathobiology, University of Toronto, University Health Network, Toronto, Ontario, Canada
Introduction: Extranodal marginal zone lymphoma (EMZL) of mucosa-associated lymphoid tissue (MALT) is the most common primary lung lymphoma and may also be seen in the pleura. Fine needle aspirates (FNA) and bronchoalveolar lavage (BAL) samples are frequently the first materials presented for the diagnosis of pleuropulmonary EMZL (PP EMZL). Histopathological findings have been well-described, but the spectrum of cytomorphological findings in FNA and BAL has not been fully explored. We investigated the utility of cytomorphological examination in a combination with ancillary tests in the specific diagnosis of PP EMZL, as defined by the 2008 revised World Health Organization (WHO) classification.
Materials and Methods: Cases of PP EMZL diagnosed cytologically from 2003 to 2010 were retrieved. All Romanowsky and Papanicolaou stained slides were reviewed by three cytopathologists. Immunophenotyping, interphase FISH, molecular assays, and imaging data were collated from the original reports. Clinical information was obtained from electronic patient records. Concurrent surgical biopsies were also retrieved.
Results: Eleven transthoracic FNA (10 lung, 1 pleura) and one BAL from five male and seven female patients with a median age of 66 years were identified. Two patients had a history of pulmonary lymphoma and one had a history of peripheral blood lymphoproliferative disorder. Six cases were incidentally discovered on radiologic examination (5 respiratory symptoms and 1 chest pain). The radiologic lesions varied from small ground glass opacities (GGO) to mass-like consolidations, which included unilateral solitary (5) and unilateral or bilateral multiple lesions (7). The radiologic differential diagnosis included lymphoma, bronchioloalveolar carcinoma (BAC), and infection in 11 cases. In two cases an inflammatory process was initially favored. Prior chronic infection (tuberculosis) was documented in only one case (FNA pleura). All samples were composed predominantly of small centrocyte-like cells. Three cases showed follicular dendritic cell meshworks and marked plasma cell differentiation. All cases showed occasional lymphoid tangles with entrapped epithelial cells, but no classical lymphoepithelial lesions. Multinucleated giant cells were present in seven cases of which two showed granulomas. Granulomas prompted submission of the sample for culture in one case. Immunophenotyping by laser scanning cytometry (10 cases) and immunohistochemistry (2 cases) confirmed B cell clonality and CD5-, CD10- immunophenotype typical of MZL in all cases. PCR showed B cell clonality in three samples (2 FNA, 1 BAL). FISH confirmed a MALT1 translocation in four out of eight cases tested, and trisomy 3 in two out of two cases. Concurrent surgical biopsies were diagnosed independently as EMZL in seven cases. Clinical management was undertaken only on the basis of the combined cytomorphological and molecular findings in five cases.
Conclusions: Recognition of a lymphoid infiltrate composed predominantly of small centrocyte-like cells and occasional lymphoid tangles with entrapped epithelial cells at rapid onsite assessment of transthoracic FNA or lymphocytosis in a BAL, in the context of a mass lesion or GGO on imaging, should prompt cell surface marker immunophenotyping, even if granulomas are identified. Specific diagnosis of PP EMZL could also be confirmed by demonstration of MALT1 translocations or trisomy 3 by FISH.
108: Extramedullary hematopoiesis: Cytomorphological, histological, and radiological findings in 12 cases
Nemanja Rodic, MD, PhD, Zahra Maleki, MD
Pathology, The Johns Hopkins Hospital, Baltimore, Maryland
Introduction: Extramedullary Hematopoiesis (EMH) is a tumor-like mass commonly seen in the liver, spleen, and lymph nodes. EMH is a physiologica; response to chronic anemia, observed in various hematological disorders such as myelofibrosis. Unanticipatted EMH is a very rare diagnosis that typically presents as a solitary mass of undetermined significance. As such, knowledge of the cytopathological characteristics as well as the clinical and radiological correlates of EMH is paramount. We share the salient clinical and radiological findings, as also the diagnostic cytopathological features of EMH in 12 cases, diagnosed with fine needle aspiration (FNA), in an effort to accustom the cytopathological community with this fascinating, albeit rare, entity.
Materials and Methods: Twelve cases of EMH were retrospectively retrieved from the cytopathology archives of a teaching hospital over the past 22 years. The cytological material was obtained by ultrasound-guided FNA. Smears were stained with Diff-Quik® (air-dried smears) and Papanicolaou stains (alcohol-fixed smears). Radiological images, medical records, and the available histology (12 cases) were reviewed.
Results: A total of 13 EMH cytopathological cases were seen. The median age at diagnosis was 63 years (40 – 88 years) and there was no gender bias (male-to-female ratio, 1 : 1.15). The presenting signs and symptoms varied widely, from incidental radiographic findings to right hemiparesis, chronic back pain, lower extremity pain, bloating, pleural effusion, and a lung mass. Likewise, presumptive clinical diagnoses in five of the thirteen cases were benign, while five of thirteen were considered malignant prior to the diagnostic FNA. The most common anatomic site for EMH was the liver (n = 4), followed by the presacral soft tissue (n = 3), and the pleura. Even as most EMH nodules were singular, few presented as up to three radiographically distinct nodules. An average EMH nodule measured 2.8 cm, whereas, EMH liver nodules were larger and measured 4.3 cm on an average (P = 0.0043). Cytological smears revealed trilineage hematopoeitic cells including megakaryocytes. The cytological findings were correlated with the histological findings in available cases. No immunohistochemical stains were performed.
Conclusions: Extramedullary hematopoiesis most commonly presents as a mass lesion, which can mimic a neoplasm radiologically. Megakaryocytes may cause diagnostic pitfalls as a poorly differentiated carcinoma or a high-grade sarcoma. EMH might also be misinterpreted as bone marrow contamination. FNA may provide accurate diagnosis and may prevent more aggressive procedures.
109: Fine needle aspiration / core biopsy of retroperitoneal lesions: Diagnostic advantages and pitfalls
Manisha Mishra, MD, Yurong Wheeler, MD
Pathology, East Tennessee State University, Johnson City, Tennessee
Introduction: Fine needle aspiration (FNA) / core biopsy appears to be an attractive method for diagnosing lesions at surgically inaccessible or difficult-to-access regions of the body, including the retroperitoneum. However, the role of FNA in the diagnosis of these lesions, especially lymphoma, is still debatable. The small sample size, triage, and representativeness issues as well as lack of tissue architecture contribute to the challenges of interpretation of these cases. We did a retrospective analysis of FNA / core biopsy cases of retroperitoneal lesions at our institute over a seven-year period. The diagnostic advantages and pitfalls are discussed.
Materials and Methods: Sixty-nine cases of FNA / core biopsy cases were retrieved from the archive of a teaching hospital (from the year 2004 to 2011). The FNA material and touch prep specimen from the core biopsy were prepared mostly by the Diff-Quik® stain method for onsite evaluations. On most occasions, a needle core biopsy was obtained for H and E stain and other ancillary studies. All slides and ancillary studies were reviewed and clinical correlation was performed.
Results: Of the 69 cases, 34 were male and 35 were female (male : female = 0.97 : 1), and the age ranged from 30 to 81 years (average = 62.2 years). The initial FNA / core biopsy diagnoses were separated into three arbitrary classes: lymphoproliferative lesions (n = 27), metastases (n = 25), and miscellaneous (n = 17) classes. The lymphoproliferative lesions included Hodgkin lymphoma (n = 2), non-Hodgkin lymphoma (n = 14), atypical lymphoproliferation (n = 5), and benign lymphoid hyperplasia (n = 6). In the fourteen non-Hodgkin lymphoma cases, nine were diffuse large B-cell lymphoma, three were follicular lymphoma, one was small lymphocytic lymphoma, and one was unclassified. The primary sites for the metastases were the female reproductive tract (n = 7), gastrointestinal (n = 6), genitourinary (n = 3), and other primaries (n = 9).The miscellaneous group included primary neoplasms, like myelolipoma, sarcoma and germ cell tumor, as well as non-neoplastic entities like fibrosis. The metastatic lesions, especially those with a known primary, were relatively easy to diagnose, with the use of immunohistochemical studies. The lymphoid neoplasms were challenging to diagnose, due to the small tissue size and sample representativeness issues. Morphologically, the neoplastic lymphocytes were present as monotonous dyshesive small or large cells with a peripheral membrane of blue hue. In our experience, with core biopsy, a majority of the lymphoproliferative lesions could be subclassified (81%) with the correlation of clinicoradiological findings and ancillary studies, such as a battery of immunohistochemical stains, flow cytometry, cytogenetics or molecular studies. About 19% of the cases were placed in the atypical category mainly due to sampling issues.
Conclusions: FNA / core biopsy provides a less invasive and minimally traumatic diagnostic method for retroperitoneal lesions. It is an accurate diagnostic tool in patients with metastatic tumors. However, when dealing with a lymphoproliferative disorder, it is important to exercise caution in using this method, especially in view of the limitations of the procedure in sampling the lesion adequately and obtaining the representative material. Therefore, correlation with clinical information and ancillary studies is very important.
110: Sub-classification of lymphoproliferative disorders in effusions, a ten-year experience (2001 – 2010)
Leung Tong, MD1, Hyang Ko, MD2, Mauro Saieg, PhD, MD2, Scott Boerner, MD2, William Geddie, MD2, Gilda da Cunha Santos, PhD, MD2
1Departments of Laboratory Medicine and Pathobiology, University of Toronto, 2Laboratory Medicine Program, University Health Network, Toronto, Ontario, Canada
Introduction: The incidence of a lymphoproliferative disorder involving body cavities is well-documented. However, with the new WHO classification and advances in personalized therapies, there is an increasing need for lymphoma sub-classification and standardization on the use of ancillary techniques, such as, immunophenotyping (IP) and molecular tests in cytological samples. The aims of the present study are to evaluate the effectiveness of our laboratory in the diagnosis and sub-classification of lymphoma in serous effusions and to assess the impact of the contribution of ancillary studies to achieve a more specific diagnosis.
Materials and Methods: Reports from the cytological fluid specimens were retrospectively collected from 2001 to 2010. Cases with a diagnosis of lymphoproliferative disorder or were suspicious for lymphoma were included in the study. The following clinicopathological characteristics were extracted from the pathology report or electronic medical record: Age at the time of the diagnosis, gender, previous clinical history of lymphoma, site, gross volume, and final diagnosis. The use of ancillary tests including IP, either flow cytometry or laser scanning cytometry, immunohistochemistry (IHC), and molecular tests, which included PCR for B-cell or T-cell monoclonality, PCR for HHV-8, and FISH for translocations were also recorded.
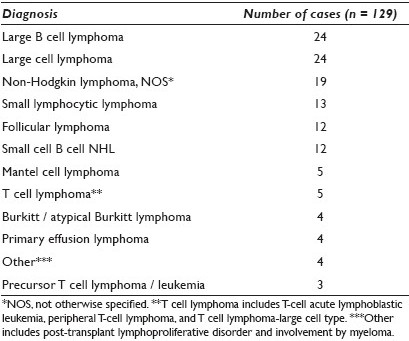
Results: One hundred and sixty-eight cytological specimens from 110 patients were included in the study. Their mean age was 58.7 (ranged 19 – 92) years. Seventy-two patients were male and 38 female. Sixty-five patients (59%) had a previous clinical history of lymphoma. The specimen site included 133 pleural, 30 peritoneal, and five pericardial fluids. The specimens’ mean volume was 238 ml with a minimum of 2 ml to a maximum of 1 liter. There were 129 cases (77%) with a morphological diagnosis of lymphoma, while 39 cases (23%) were diagnosed as suspicious for lymphoma. The distribution of lymphoproliferative disorder diagnoses is shown in Table 1. Overall, 106 cases were submitted for ancillary tests, while 62 were not submitted for any ancillary tests. IP was performed in 96 cases and immunohistochemistry in 22 cases. Molecular tests were completed in 20 cases. Among the lymphoma cases, 83 out of 129 cases (64%) underwent IP. Sixteen out of 129 (12%) lymphoma cases were also submitted for molecular tests, of which five showed B-cell or T-cell monoclonality by PCR, three cases showed MYC rearrangement, two cases showed IGH / BCL2 translocation, and six cases had negative results. Ancillary tests helped to establish a specific lymphoproliferative disorder diagnosis in 54 out of the 106 cases (51%) submitted for ancillary tests. Among the suspicious cases, 13 out of 39 cases (33%) underwent IP, of which three showed clonality, one showed a non-clonal B-cell population, six cases showed reactive T lymphocytes and three were non-contributory due to degeneration or non-specific binding.
Conclusions: The use of immunophenotyping and molecular tests in fluid samples has proven to refine the diagnosis of lymphoproliferative disorders and can be performed in a substantial number of cases, as the mean volume of these samples is sufficient to run multiple analyses. In the effusion samples, a specific lymphoma sub-type can be achieved in over 50% of the cases, by using a combination of cytomorphology and ancillary techniques.








