Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
Quality Assurance
116: FNA rapid onsite assessment of adequacy: The experience of an academic institution
Nariman Gobara, MS, MBChB, Li Liang, MD, Nora Morgenstern, MD, Patricia Wasserman, MD, Chiara Sugrue, MS, SCT(ASCP)
Cytopathology Division, North Shore LIJ Health System, Lake Success, New York
Introduction: Cytotechnologists and cytopathology Fellows often perform rapid onsite assessment (ROSA) of a fine needle aspirate (FNA) to provide immediate feedback regarding the adequacy of the material and to triage the specimens for additional ancillary studies. The current study was designed to assess the concordance of onsite adequacy assessment of FNA as correlated with the final cytology diagnosis.
Materials and Methods: A retrospective search of all FNA ROSA between 1 January 2009 and 31 December 2010 yielded a total of 1,520 cases. The FNA ROSA was correlated with final cytology diagnosis and classified as either ‘concordant’ or ‘discordant’. An ‘adequate’ FNA ROSA was considered ‘concordant’ if a definitive final cytology diagnosis was reached and ‘discordant’ if no definitive final diagnosis was reached or was reached based on limited material. An ‘inadequate’ FNA ROSA was considered ‘concordant’ if no definitive final diagnosis was reached and ‘discordant’ if a definitive final diagnosis was possible. Special consideration was given to inherently hypocellular lesions (e.g., cysts, colloid nodules, abscesses, etc.) as well as to diagnoses limited by the nature of the lesion rather than the sample (e.g., follicular neoplasm of the thyroid).
Results: Out of the total of 1,520 FNA ROSA analyzed, 1,230 cases were considered adequate and 290 cases were considered inadequate. Out of the 1,230 adequate FNA ROSA, 1,180 (96%) were considered concordant with final diagnosis, for a discordance rate of 4%. Out of the 290 inadequate FNA ROSA, 275 (95%) were considered concordant with final diagnosis, for a discordance rate of 5%. FNA of the salivary glands yielded the highest discordance rates (6%), while liver FNA showed the lowest discordance rates (1%). Two hundred and twenty cases of FNA ROSA were performed without image-guidance and showed a 5% discordance rate, a value similar to that of image-guided FNA ROSA. Finally, the number of passes for the discordant cases was analyzed and it revealed that 23% of the discordant cases had less than two passes, 64% had three to five passes, and 13% had more than six passes.
Conclusions: Cytotechnologist and cytopatholology Fellows are, overall, highly competent in providing rapid onsite assessment of adequacy. Salivary gland FNA showed the highest discordance rate, while liver FNAs showed the lowest. The number of passes and location of the lesions did not significantly influence the discordance rates. The focus review and study of these discordant cases may improve ROSA accuracy. A maximum discrepancy ROSA rate of 5% could be used as a quality assurance benchmark in FNA cytology.
117: Additional levels are not an effective way to reconcile discrepancies between reported cytological and histological diagnoses in cervicovaginal biopsies
Julie Kunkel, MD, Hannah Krigman, MD
Pathology and Immunology, Washington University, St. Louis, Missouri
Introduction: Colposcopic cervical biopsies for reported cytological abnormalities do not always show intraepithelial neoplasia on the three levels routinely performed at our institution. We examined the utility of the three additional tissue levels in biopsies for detection of epithelial lesions, because the current ASCCP guidelines treat biopsy-confirmed epithelial abnormalities more aggressively. We examined the discordance rate for Paps and biopsies with and without additional levels. Endometrial lesions were not included.
Materials and Methods: The Pathology database from January 2009 to July 2010 was searched for all patients with abnormal cervicovaginal cytology diagnoses and any surgical pathology within three months of Pap smears. All cases with concurrent cervicovaginal smears and biopsies were recorded. The paired samples were categorized as concordant (195 cases), discordant (200), or atypical on Pap ((ASCUS (145) or AGUS (83), ASC-H (35)). Concordant biopsies and paps were within one degree of the diagnosis.
Results: Eighteen concordant cases (9%), 14 atypical cases (7%), and 19 discordant cases (10%) were further evaluated by additional levels. The eighteen concordant cases were nine low-grade squamous intraepithelial lesions (LSIL), eight high-grade in squamous intraepithelial lesions (HSIL), and one case of invasive carcinoma, arising from the HSIL. In the concordant cases, most levels were obtained to exclude higher grade lesions. Only in two of the concordant cases (1% of sampled cases) did the additional levels change the diagnosis. The atypical cases with levels examined were ASC-H (3) or ASCUS positive for HPV (11). The discordant cases had diagnoses of HSIL (7) and LSIL (11). Of the ASC-H cases, one had denuded stroma, one was CIN-1, and one was benign. No diagnoses changed after the levels were obtained. In case of the ASCUS cases, six were benign even after six levels. Two ASCUS cases were diagnosed as CIN1 after six levels; while three cases were CIN2-3. Of the LSIL Pap cases, 10 were benign after extensive levels. One case changed from benign to CIN2 after six levels. In one HSIL and one LSIL case, the reorientation and levels found the CIN that was present on other biopsy fragments, so no additional data were obtained.
Conclusions: At our institution, additional levels did not provide significant information in the majority of cases, regardless of the category. For this reason, additional levels were not considered as a cost-effective or time-effective mean for reconciling differences in the diagnoses. Resampling, re-examination, and follow-up provide more effective means of reconciliation. Roughly a third of the biopsies are concordant with the diagnosis rendered on cervicovaginal cytology. Additonal levels were examined on a few of these to exclude higher grade lesions; diagnoses did not change significantly. A third of the biopsies were discordant. A third of the cases represented biopsies after an atypical Pap (ASCUS or AGUS). Of those 50 cervicovaginal biopsies, examination of additional levels changed the diagnosis in each of the three cases with Pap diagnosis of LSIL. In two of those cases, a diagnosis of CIN1 was made and in the other CIN 2, after the levels. This series suggests that additional levels are not an effective way to reconcile discordance between Pap smear and biopsy in these patients, who will already be followed for abnormal Pap.
118: Cytology-histology correlations in gynecological pathology, trends and results
Debora Smith, CT(ASCP), Mary Schwartz, MD, Subhendu Chakraborty, MS, Todd Fairley, CT(ASCP), Dina Mody, MD
Pathology, The Methodist Hospital, Houston, Texas
Introduction: Cytohistological correlation of high-grade squamous intraepithelial lesions and malignant cases is mandated for gynecological cytology under the Clinical Laboratory Improvement Amendments of 1988. However, details as to how this is done and timelines are not specified. The results of and statistics derived from these correlations are mandated to be a part of the laboratory's quality improvement data and are reviewed by accrediting agencies as part of the cytology laboratory inspections. We reviewed our laboratory's cytohistological correlations over a ten-year period. The case mix includes Pap tests and biopsies obtained in private practice ob-gyn offices, charity clinics including a dysplasia clinic, and gynecological oncologists’ offices.
Materials and Methods: Data derived from gynecological cytohistological correlations performed at our institution between 2000 and 2009 was reviewed for trends. All cervical and vaginal biopsies with previous abnormal cytology in the HSIL / carcinoma and adenocarcinoma in-situ categories were included. Between 2000 and September 2004, the biopsies were interpreted by the general surgical pathology service. Beginning in Fall 2004, that practice changed and all gynecological cytology as well as all cervical and vaginal biopsies with previous abnormal cytology in our files were interpreted by pathologists on the gynecological (gyn) cytology service. The pathologists on the gyn cytology service were all Board-certified cytopathologists who practiced both gynecological cytology and surgical pathology. Not all surgical pathologists who signed out cervical and vaginal biopsies during 2000 to 2004, signed out gynecological cytology or had subspeciality expertise in gyn pathology. During that same time period, gynecological cytology was signed out by anatomical pathologists who signed out cytology and not all had subspeciality expertise in cytopathology. The Pap tests included ThinPrep® and SurePath®, both manually screened and imager screened. The data was viewed in aggregate for 2000 – 2009 and a comparison of the earlier years (2000 – 2003) to the later years (2005 – 2009) was also performed. Data from 2004 was excluded from the comparison as it was the transition year.
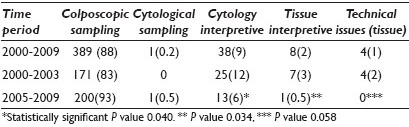
Results: The most frequent cause of noncorrelation between the Pap test and biopsy was a colposcopic biopsy sampling variance followed by cytology interpretive variance. When comparing the earlier time period with the later period, the number and percent of cases due to cytological and histological interpretive variances dropped and this difference was statistically significant [Table 1]. Technical issues related to tissues were resolved in the later period by deeper levels, reorientation of blocks or immunohistochemical staining for biomarkers. While technical issues were eliminated in the later time period, this difference did not reach statistical significance with a P value of 0.058 on Fisher's exact chi square test.
Conclusions: Gynecological–cytohistological correlation is a quality indicator and the results of this correlation are critical for optimal patient management. This study demonstrates the benefit to patient care by changes in pathology practice where real-time correlation by the same group of individuals with subspecialty expertise can decrease interpretive variances and variances due to tissue-related technical issues.
119: More frequent use of p16 / Ki67 on cervical biopsy specimens improves cervical cytohistological agreement rates
Tetyana Mettler, MD1, Charanjeet Singh, MD1, Arbaz Samad, MD1, Kay Savik, MS2, Samy Amrouche, CT(ASCP)3, Jana Holler, CT(ASCP)3, Bharat Thyagarajan, MD1, Evin Gulbahce, MD1, Stefan Pambuccian, MD1
1Laboratory Medicine and Pathology, University of Minnesota, Minneapolis, Minnesota; 2School of Nursing, University of Minnesota, Minneapolis, Minnesota; 3Cytology Laboratory, University of Minnesota Medical Center, Fairview, Minneapolis, Minnesota
Introduction: Cervical cytohistological correlations are routinely performed in cytology laboratories as a measure of quality assurance. However, the ‘gold standard’ against which the cytological (Pap test) diagnosis is judged, the histological (biopsy) diagnosis is itself marred by subjectivity. Studies have shown high inter-pathologist variability of cervical biopsy diagnoses and that p16 and Ki67 stains performed on cervical biopsies improved the diagnostic agreement between pathologists and their diagnostic accuracy. The aim of this study was to determine the impact of different pathologists’ frequency of use of p16 / Ki67 stains on cervical biopsies on cervical cytohistological correlations.
Materials and Methods: We identified all cervical biopsies on which p16 / Ki67 stains were performed (or not) in our institution from 1 January, 2005 to 30 September, 2010. The following data were recorded for each biopsy: (1) patient age, (2) preceding Pap test, and when available, HPV result obtained within six months of the biopsy, (3) the most severe grade of dysplasia on biopsy, dichotomized as CIN0 / 1 or CIN2 / 3+ and (4) biopsy pathologist. Minor and major cytohistological discrepancy rates (One- and respectively two-step differences between Pap test and biopsy result) were determined for each biopsy. The frequency of use of p16 / Ki67 in cervical biopsies was calculated for each pathologist. The pathologists were then classified as ‘high users’ of p16 / Ki67 when their frequency of use of p16 / Ki67 was above the unweighted mean of all pathologists, or ‘low users’ when it was below. Immunostains for p16INK4a (clone E6H4™, CINtec® ) and Ki67 (clone 30-9, Ventana) were performed on Ventana NexES.
Results: During the study period, 23 pathologists interpreted cervical biopsies from 11,850 women aged 14 to 83 (mean 33 ± 11.8) years. Prior Pap test results showed NILM (2,302, 19.4%), ASC-US (3,161, 26.7%), LSIL (3,458, 29.2%), ASC-H (837, 7.1%), LSIL-H (710, 6.0%), AGC (367, 3.1%), and HSIL+ (1015, 8.6%). The biopsy diagnoses included 2,240 (18.9%) CIN2 / 3+. p16 / Ki67 staining was used in 1201 / 11850 (10.14%) cases. p16 / Ki67 stains were ordered for biopsies following Pap tests diagnosed as NILM (8.08%), ASC-US (31.39%), LSIL (26.23%), ASC-H (12.57%), LSIL-H (7.33%), HSIL+ (12.03%). p16 was used the most when the prior Pap test result was ASC-H (18.04%), followed by HSIL (14.39%), LSIL-H (12.39%), ASC-US (11.93%), and least when the prior Pap test diagnosis was LSIL (9.11%) or NILM (4.21%). The 23 pathologists included in the study diagnosed 59 – 1811 (mean 518 ± 543) cervical biopsies and used p16 / Ki67 in 0 – 21.31% of these biopsies (unweighted mean 7.83%). Individual pathologists diagnosed 6 – 413 (mean 97 ± 115) cases as CIN 2 / 3+, which represented 9.49 – 24.12% of their cervical biopsy diagnoses. The 11 ‘high users’ of p16 / Ki67 had a lower rate of major cytohistological disagreements than the 12 ‘low-users’ (1059 / 8391, 12.62% vs. 516 / 2943, 14.92%, P < 0.0001). ‘High users’ of p16 / Ki67 also had a lower rate of biopsy diagnoses of less than CIN2 / 3 in women with prior Pap test diagnoses of ASC-H, AGC or HSIL+ (1146 / 8391, 13.66% vs. 570 / 3459, 16.48%, P < 0.0001).
Conclusions: Our results show a high variability of use of p16 / Ki67 in cervical biopsies by pathologists practicing within the same institution. We also found that more frequent use of p16 / Ki67 by biopsy pathologists improved cervical cytohistological correlation rates, by lowering the rates of major discrepancies.
120: Does immunohistochemical subtyping of non-small cell lung carcinoma in fine needle aspiration play a similar role as in surgical resection tissue?
Brooke Koltz, Zachary Sletten, Donna Russell, Thomas Bonfiglio, Haodong Xu, Zhongren Zhou
Pathology and Laboratory Medicine, University of Rochester, Rochester, New York
Introduction: Personalized therapies require subtyping of non-small cell lung carcinomas (NSCLCs) into adenocarcinoma and squamous cell carcinoma. A four antibody (p63, CK5 / 6, TTF-1, and napsin A) immunohistochemical (IHC) panel is widely applied for subtyping NSCLSs in fine needle aspiration (FNA), biopsy, and surgical resection tissue (SRT). However, the IHC study is unreliable in some FNA cell blocks. A quality control study in matched lung FNA and surgical resected lung cancer has rarely been done.
Materials and Methods: Three hundred and ninety-eight lung resections were performed at our institution during 2008 – 2011, of which 24 cases had the diagnosis of adenocarcinoma or squamous carcinoma with matched FNA and satisfactory cell blocks. The immunohistochemical studies for TTF-1, napsin A, cytokeratin 5 / 6 and p63 were used for both SRT and FNA cell blocks in 12 cases (five adenocarcinomas and seven squamous carcinomas). The results were evaluated independently by three pathologists.
Results: Six (86%) of seven squamous cell carcinomas in SRT showed both p63 and CK5 / 6 positive IHC staining. One case was positive for CK5 / 6, but negative for p63 stain. The identical IHC staining pattern was observed in the matched FNA cases. Four (80%) of five adenocarcinoma cases in SRT exhibited both TTF-1 and napsin A positive IHC staining. One case only showed positive TTF-1. All five FNA cases showed both TTF-1 and napsin A positive IHC staining. Two (40%) of the five adenocarcinoma cases in SRT showed a focal p63 IHC stain, which was not identified in all the five adenocarcinoma FNA cases.
Conclusions: The IHC studies on FNA cell blocks and SRT showed similar staining patterns. The IHC subtyping of non-small cell lung carcinomas in the FNA specimen played an important role similar to that in the SRT specimen. Focal p63 positivity found in a portion of surgically resected adenocarcinomas, but not in matched FNA indicated that the p63 positive cells were not sampled by FNA.








