Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
Soft Tissue / Bone
121: Is fine needle aspiration cytology a sensitive diagnostic tool for granular cell tumors? A cytohistological review with emphasis on pitfalls
Susan Haley, MD, Vicki Schnadig, MD, Ranjana Nawgiri, MD
Pathology, The University of Texas Medical Branch, Galveston, Texas
Introduction: Granular cell tumors (GCT) are relatively uncommon neoplasms thought to be of neural origin. Although they may appear as cellular smears of cohesive and single cells with bland nuclei and abundant granular cytoplasm, the cytological appearance on fine needle aspiration (FNA) is variable. The differential diagnoses are many and include infections, benign, and malignant neoplasms. The polygonal cells and granular cytoplasm can be mistaken for necrosis and histiocytes; therefore, atypical infections, granulomatous inflammation, and histiocytic tumors are considered in the differential diagnoses. In the breast, GCT may resemble fibrocystic changes, including apocrine metaplasia; and in thyroid, cells can resemble oncocytic Hürthle cells. CGT presenting as a fragile bare nuclei with prominent nucleoli may also resemble renal cell carcinoma, alveolar soft parts sarcoma, or melanoma.
Materials and Methods: All cases of suspected GCT on cytology within the previous ten years were identified, and nine cases were retrieved. Three patients had been lost to follow-up. The medical records of the remaining six patients were then reviewed for histopathological and clinical findings.
Results: Two painful neck masses in a 65-year-old woman and 29-year-old man were confirmed by histology as GCT. A thyroid nodule in a 40-year-old woman was later diagnosed as Hürthle cell adenoma; a lung mass in a 44-year-old man was ruled as poorly-differentiated carcinoma; and a breast mass in a 78-year-old woman was ruled as a fibrocystic change. One case of suspected malignant GCT was later diagnosed as unclassified sarcoma.
Conclusions: Granular cell tumor is a rarely encountered entity on FNA preparations and may closely mimic other conditions, and the cases presented highlight the often unusual cytology findings seen in entities that resemble GCT. Awareness of this entity and its differential diagnoses, along with careful clinical correlation is critical in the accurate interpretation of the findings.
122: Giant cell tumor of tendon sheath: Cytomorphological, histological, and radiological findings in fourteen cases
Cheng-Ying Ho, MD, PhD, Zahra Maleki, MD
Pathology, The Johns Hopkins Hospital, Baltimore, Maryland
Introduction: Giant cell tumor of tendon sheath (GCTTS), also known as pigmented nodular tenosynovitis and fibrous xanthoma of synovium, is a common soft tissue lesion. The lesion occurs in young adults with a peak incidence in the age group of 40 to 50 year olds. It most commonly affects small joints of hands and is known to be associated with degenerative joint disease. It presents as a firm, multilobular, slow-growing, nontender mass located adjacent to the synovium of the tendon sheath. Radiological features include a well-defined, round, soft tissue mass, eccentric to or enveloping the tendon sheath, with or without osseous erosion. Bone involvement is considered to be more aggressive. Complete excision is the treatment of choice. The incidence of local recurrence is high, ranging from 4 – 45%. Herein, we describe the cytomorphological features of GCTTS and the usefulness of ultrasound-guided FNA as an initial diagnostic modality.
Materials and Methods: Fourteen cases of GCTTS were retrospectively retrieved from the cytopathology archives of a teaching hospital. The cytological material was obtained by ultrasound-guided FNA. Smears were stained with Diff-Quik® and Papanicolaou stains. Radiological images, medical records, ancillary studies, and available histology (12 cases) were reviewed.
Results: The 14 cases selected included three males and 11 females ranging in age from 11 to 63 years (mean = 32 years). GCTTS involved the lower extremity in 11 cases and upper extremity in three cases. The site of involvement included knee (n = 3), toe (n = 3), ankle (n = 2), leg (n = 2), foot, wrist, palm, and finger (one case each). Small joint involvement was seen in five cases. The entire 14 cases presented with a unifocal lesion. The majority (8 cases) of the lesions were immobile. Bone involvement was seen in three cases. The tumor size ranged from 1.5 cm to 9.5 cm (Mean = 3.6 cm). Three cases had bone involvement. One case had subcutaneous involvement. Six cases had a painful presentation. Two cases had a known history of trauma. Only one case was a recurrence. Microscopic examination revealed hypercellular smears with abundant polygonal, round or spindle stromal cells. Multinucleated giant cells, hemosiderin-laden macrophages, and foamy histiocytes were noted. The stromal cells lacked pleomorphism and displayed occasional nuclear grooves or intranuclear inclusions. Mitosis was absent. The stromal cells were immunoreactive for CD68 and negative for cytokeratin, CD34, and desmin. Cytomorphological findings were correlated with the histological findings in all 12 cases. Histological sections demonstrated a round-to-oval mass surrounded by a thin layer of fibroconnective tissue. The mass consisted of sheets of stromal cells varying in morphology from small oval shaped with minimal cytoplasm to large polygonal with abundant vacuolated cytoplasm. Numerous multinucleated giant cells were seen, the majority of which were in clusters. Extracellular hemosiderin deposition was most prominent at the periphery of the stromal cells. Occasional hemosiderin-laden macrophages were noted. Mitotic figures were rare.
Conclusions: Our study demonstrates that ultrasound-guided FNA is a useful method to obtain diagnostic material for GCTTS. Awareness of the cytomorphological features of GCTTS and the typical clinical setting will permit an accurate diagnosis and eliminate the need for preoperative biopsy.
123: Fine needle aspiration of epithelial tumors and tumor-like lesions of the skin: A single institute experience
Manisha Mishra, MD1, Surendra Verma, MD2, George Youngberg, MD1, Neelaiah Siddaraju, MD2, Tamar Giorgadze, MD3
1Pathology, Quillen College of Medicine, East Tennessee State University, Johnson City, Tennessee; 2Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India; 3Pathology, Wayne State University, Detroit, Michigan
Introduction: Although fine needle aspiration (FNA is widely practiced as a diagnostic method for superficial and deep lesions, it has not enjoyed as much popularity for the diagnosis of skin nodules. Its advantages include low cost, simplicity of technique, and minimal trauma. In spite of its obvious advantages in its use for the diagnosis of skin lesions, few large studies have been published about the role of FNA as a primary method of diagnosing epithelial lesions presenting as skin nodules. We encountered 47 cases at a tertiary care institute in India over a 22-month period.
Materials and Methods: All patients presenting with non-inflammatory skin nodules between August 2003 and June 2005 underwent FNA before incisional / excisional biopsy. A diagnosis was rendered on FNA and the forty-seven cases that received a subsequent histological diagnosis of an epithelial lesion were included in this study.
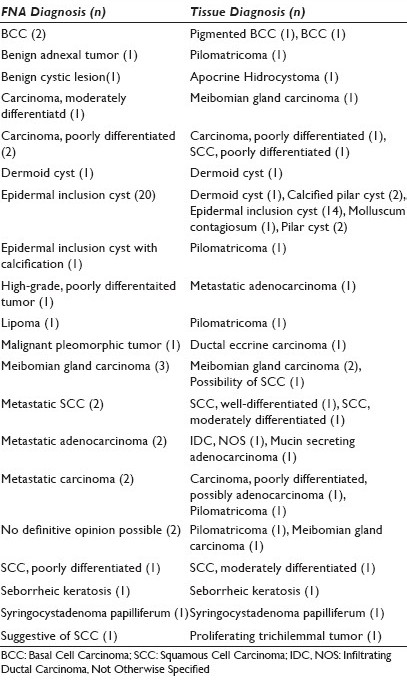
Results: Cyto–histo correlation was performed and a statistical analysis was done [Tables 1–3]. Sensitivity was 78.9%, specificity was 96.2%, and diagnostic accuracy was 88.8% for FNA as a primary diagnostic modality for the diagnosis of epithelial skin lesions.


Conclusions: FNA is a highly specific and moderately sensitive method of diagnosis for epithelial lesions of the skin. It has a high diagnostic accuracy for such lesions and is very safe and cost-effective as a diagnostic technique.
124: Role of fine needle aspiration as a primary diagnostic method for mesenchymal tumors and tumor-like skin nodules: Twenty-two months’ experience at a single institute
Manisha Mishra, MD1, Surendra Verma, MD2, George Youngberg, MD1, Neelaiah Siddaraju, MD2, Tamar Giorgadze, MD3
1Pathology, East Tennessee State University, Johnson City, Tennessee; 2Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India; 3Pathology, Wayne State University, Detroit, Michigan
Introduction: Fine needle aspiration (FNA) is a widely used diagnostic procedure in the current medical milieu. It is inexpensive, simple to perform, and is a relatively less invasive diagnostic modality. However, few large studies have been done to evaluate the role of FNA as a primary method of diagnosing mesenchymal lesions presenting as skin nodules. We intend to present our study of 49 cases of skin nodules, which we encountered during a 22-month period at a tertiary care institute in India.
Materials and Methods: All patients presenting with skin nodules between August 2003 and June 2005 underwent FNA before incisional / excisional biopsy. Inflammatory lesions were excluded from the study. A cytological diagnosis was rendered. Only forty-nine cases in which a subsequent histological diagnosis was available and revealed a mesenchymal lesion were included in this study.
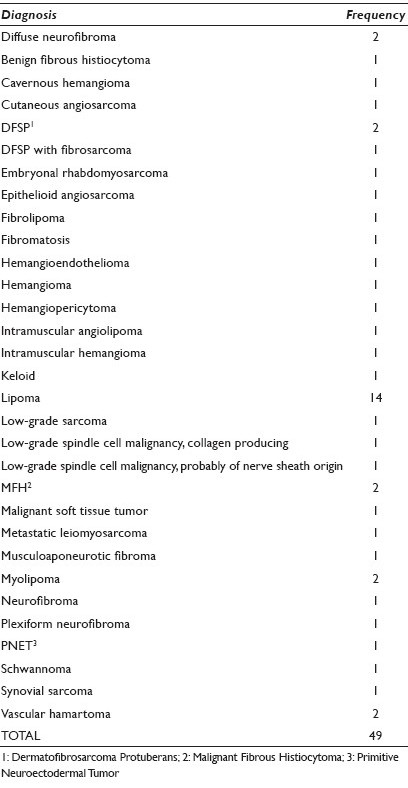
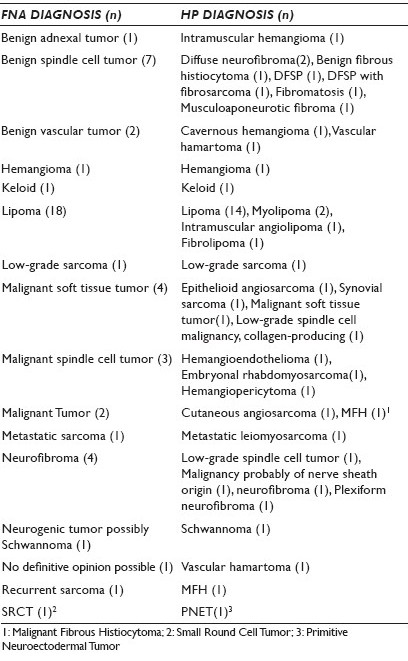
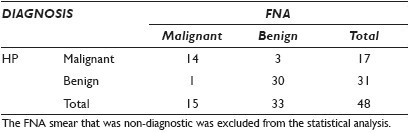
Results: The results of our study are outlined in Tables 1–3. Statistical analysis showed that the sensitivity was 93.3%, specificity was 90.9%, and diagnostic accuracy was 91.7% when FNA was used as a primary diagnostic modality for the diagnosis of mesenchymal skin lesions.
Conclusions: Our study showed high diagnostic accuracy of FNA as a primary diagnostic modality in the diagnosis of mesenchymal lesions of the skin. The sensitivity was higher than the specificity for diagnosing mesenchymal lesions, but both values were above 90%, which made FNA a very valuable diagnostic procedure for such lesions, because it was also an inexpensive and minimally invasive diagnostic technique.
125: Utility of fluorescence in-situ hybridization in bone and soft tissue cytopathology: A seven-year experience at an academic medical center
Fay Jia, PhD, Walid Khalbuss, MD, PhD, Sara Monaco, MD, Urvashi Surti, PhD, Kathleen Cieply, BSc, Liron Pantanowitz, MD
Pathology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Introduction: Fluorescence in-situ hybridization (FISH) is a sensitive and highly specific method that can be used for diagnostic purposes, as well as for the evaluation of predictive biomarkers for therapeutic decision-making. There has accordingly been a greater demand to perform FISH tests on cytology specimens. The aim of this study is to report our experience by utilizing FISH in a large series of non-gynecological cytology samples.
Materials and Methods: A retrospective study was performed evaluating all bone and soft tissue cytopathology cases in which ancillary FISH testing was performed over a seven-year period. In all cases the final cytology diagnosis, FISH test results, and other ancillary studies (immunocytochemistry, flow cytometry) were recorded. The additive value of FISH for each case was determined. Data were captured and analyzed using descriptive statistics (Excel).
Results: In 128 cases FISH was ordered as an ancillary test. FISH was performed for four diagnostic categories, including 51 hematolymphoid cases (40%), 44 soft tissue tumors (34%), 30 metastatic carinomas (24%), and three miscellaneous cases (mesothelioma, neuroendocrine carcinoma, benign bone lesion). FISH was unsuccessful in six cases (5%) due to insufficient material procured from five soft tissue neoplasms and one metastatic breast carcinoma. For lymphomas, FISH was helpful in 46 (90%) cases used to evaluate clonality (IgH), specific translocations (MYC, BCL1, BCL2, BCL6, MALT1), and ALK rearrangement. In five cases (10%) diagnostic of lymphoma (1 Hodgkin, 4 non-Hodgkin), FISH was not deemed additive as IgH rearrangement was inconclusive (n = 1) or negative (n = 4). Among soft tissue tumor cases, FISH proved helpful in the diagnosis of 41 cases (93%), specifically for liposarcomas (CHOP, FUS, MDM2), alveolar rhabdomyosarcoma (FKHR), synovial sarcoma (SYT), and EWSR1 positive sarcomas. FISH in one case of recurrent synovial sarcoma (SYT negative) and two cases of PNET (EWSR1 negative) was not additive. In all adenocarcinoma cases, FISH provided Her2 / neu (28 breast carcinomas) and EGFR (two lung tumors) results.
Conclusions: These data show that at our institution FISH can be successfully performed on the majority (95%) of bone and soft tissue cytology specimens. FISH is especially helpful in diagnosing lymphomas and soft tissue sarcomas, as well as in evaluating therapeutic biomarkers (like Her2 / neu and EGFR) in cytology samples containing breast or lung adenocarcinoma.
126: Nodular fasciitis: Cytomorphological findings and diagnostic issues on fine needle aspiration
Gang Zheng, MD, PhD, Matthew Olson, MD, Syed Ali, MD
Pathology, The Johns Hopkins Hospital, Baltimore, Maryland
Introduction: Nodular fasciitis (NF) is a common benign mimicker of sarcoma on fine needle aspiration (FNA). The cytomorphological characteristics have rarely been described in published series in the literature. We retrospectively analyzed 13 cases of NF from a single institution with elaboration of the morphological features and differential diagnosis.
Materials and Methods: A retrospective search of the pathology archives of a large tertiary care center identified 13 cases of NF in a 12-year period (1999 – 2011). Of these, eight cases had tissue confirmation (biopsy and / or resection). Material was obtained by ultrasound-guided FNA and direct smears were stained with Diff Quik® and Papanicolaou stains.
Results: The patients ranged in age from 7 to 63 years (median: 38) with a M : F ratio of 1 : 1.7. The cytopathological diagnoses included ‘NF’ (9) and ‘Spindle cell proliferation or neoplasm, NOS’ (3). One case was deemed non-diagnostic. The lesions ranged in size from 2 to 5.5 cm (mean: 3.5 cm). These were located in the lower extremity (37.5%), upper extremity (25%), face (12.5%), parotid (12.5%), and trunk (12.5%). The patients presented with pain in 63% of the cases. No prior history of injury or trauma was available in any of the cases. Salient cytomorphological features included hypercellularity with mostly single cells arranged haphazardly, ‘tissue culture appearance’, few tissue fragments with cells embedded in the myxoid matrix, variable amount of loose myxoid stroma, bipolar spindled cells with oval nuclei, and pale blue wispy cytoplasm. Four cases showed few multinucleated giant cells and large ganglion-like cells. Focal significant atypia (pleomorphism, high N / C ratios, macronucleoli) was present in half of the cases. Mitosis and necrosis were absent. Immunostaining with smooth muscle actin performed in few cases was diffusely positive.
Conclusions: The cytomorphological characteristics of NF often overlap with a number of benign and malignant spindle cell neoplasms, resulting in a broad differential diagnosis on FNA. In the right clinicoradiological context, the presence of cytomorphological features, as mentioned earlier, may support the diagnosis of NF. Immunostaining with muscle cell actin may help narrow the list of differential diagnosis. A conservative diagnostic approach is recommended when cytological atypia is encountered in NF, to avoid false positive diagnoses.








