Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
Genitourinary (Kidney and Bladder)
27: Impact of cytodiagnosis on triaging of patients with renal lesions: An eleven-year retrospective study
Israh Akhtar, MD, Anwer Siddiqi, MD, Rhyne Flowers, MD, Mithra Baliga, MD
Department of Cytopathology, University of Mississippi Medical Center, Jackson, Mississippi
Introduction: The use of image-guided fine needle aspiration (FNA) and core biopsy (CB) in the diagnosis of renal lesions has a considerable impact on clinical management. We undertook a retrospective study to evaluate the treatment approach based on the cytological diagnoses of these lesions.
Materials and Methods: A retrospective review of the renal FNAs and CBs performed at our institution during the past 11 years (from 2000 to present) was conducted. The accuracy of the cytological diagnoses and treatment approach based upon the follow-up data was then evaluated.
Results: Eighty-two FNAs and / or core biopsies were performed on suspected renal lesions during this time period. These were performed on 81 patients, 49 males and 32 females, ranging in age from 4 to 87 years. The most common indication for performing these procedures was the presence of a renal mass, either solid or cystic. The diagnoses were broadly classified into five main categories: Positive for malignancy, suspicious / suggestive of malignancy, benign neoplasm, negative for malignancy, and non-diagnostic. Forty-four cases were positive for malignancy, seven cases suspicious / suggestive of malignancy, one benign neoplasm, 28 negative for malignancy, and two non-diagnostic. The most common malignant neoplasm was renal cell carcinoma (RCC) and its variants, that is, clear cell type (n = 22), papillary RCC (n = 4), sarcomatoid RCC (n = 1), and collecting duct / medullary carcinoma (n = 1). Other malignant neoplasms were Non-Hodgkin's Lymphoma (n = 4), leiomyosarcoma (n = 1), small round blue cell tumor (n = 1), and metastatic malignancies (n = 10). One Non-Hodgkin's Lymphoma case was false positive, with the follow up of the resected transplanted kidney showing chronic rejection and no evidence of lymphoma. In the suspicious category, one case, suspicious for RCC, was positive for RCC on follow up. Five cases were suspicious / suggestive of oncocytoma, two were suggestive of angiomyolipoma and a differential was provided in these cases with no available follow-up. The most common cause of negative diagnosis was a renal cyst. A majority of these patients were not re-biopsied and were routinely followed up as per clinical protocol. However, one case that was negative by cytology, but highly suspicious by imaging, was resected and the histopathological diagnosis was cystic RCC. Out of the two non-diagnostic cases, one was re-biopsied and diagnosed as RCC. In two RCC cases, the previous cytology specimen of voided urine was highly suspicious for malignancy. Tumors metastatic to the kidney most commonly originated from the lung (n = 5, four non-small cell and one small cell), one from the cervix, one metastatic osteosarcoma, one metastatic urothelial carcinoma, and two poorly differentiated carcinomas, which could not be further classified. Thirty out of 81 patients had either a histopathological correlation or previously confirmed diagnoses. Only 17 patients had surgical resection and two had open biopsy.
Conclusions: From the study undertaken, we conclude that image-guided FNA / CB is a safe, cost-effective, and a fairly accurate diagnostic mode for triaging suspicious renal lesions. Based on the cytological diagnoses, out of 81 patients, only 17 (20.9%) had a major surgical intervention, two (2.4%) had biopsy confirmation, and 62 (76.5%) were followed up as per clinical protocol.
28: Concurrent polyoma virus infection is common in allograft transplant patients with urothelial carcinoma
Ramneesh Bhatnagar, MD, Cinthia Drachenberg, MD, Paul Staats, MD
Pathology, University of Maryland, Baltimore, Maryland
Introduction: Polyoma virus infection is a frequent finding in the urine cytology of immunocompromised patients, especially renal transplant patients. The presence of polyoma virus infection with concurrent high-grade urothelial carcinoma is uncommon, but has been reported in rare cases. The distinction between degenerated polyoma virus infected cells and those of high-grade urothelial carcinoma can be challenging, and the possibility that a patient with a history of polyoma infection may develop urothelial carcinoma should not be overlooked.
Materials and Methods: We retrospectively reviewed the reports of all voided urine cytology cases that were interpreted as ‘Positive for Malignancy’ or ‘Suspicious for Malignancy’ at our institution over a six-year period, from 2005 to 2011, to identify cases of urothelial carcinoma. These patients’ medical records were reviewed for evidence of prior organ transplantation or immunosuppression and prior evidence of polyoma virus infection. The cytological features of all cases of high-grade urothelial carcinoma with reported concurrent polyoma virus infection were reviewed by two pathologists, to confirm the interpretation.
Results: During a six-year interval, 33 cases of high-grade urothelial carcinoma were diagnosed on urine cytology, 22 of which were confirmed by tissue histology. Five of the 22 patients were renal allograft recipients. Four patients with high-grade carcinoma also had concurrent polyoma virus infection; and all had a history of renal transplant (4 / 5; 80%). In two of the cases, immunostain for SV-40 confirmed the cytological impression of a coexistent polyoma virus infection. Distinction of polyoma virus infected cells from malignant cells, on cytology, could be challenging. Features that favored the polyoma virus included: Single cells, round nuclei with smooth to slightly irregular nuclear membranes, and granular or homogenous cytoplasm. The presence of a single large, smooth, granular or vesicular nuclear inclusion was the most specific finding. Features that favored urothelial carcinoma included clusters of cells, marked size variation, coarse chromatin texture, marked nuclear contour irregularities, prominent nucleoli, and cytoplasmic vacuolization.
Conclusions: Even as concurrent urothelial carcinoma and polyoma virus infection have been reported only rarely in literature, it has been a relatively common finding in our study population, particularly among renal transplant recipients. Awareness of this overlap is important to avoid underdiagnosis of either entity, particularly urothelial carcinoma, in immunocompromised patients. Due to the significant overlap in the morphological features, the recognition of both components may be challenging, but there are several features in addition to the intranuclear inclusions of polyoma virus that can aid in making the diagnosis. Polyoma virus infection has demonstrated oncogenic potential by inactivating p53; however, its specific role in urothelial carcinoma is not well known. Although a causative relationship between polyoma virus and high-grade urothelial carcinoma cannot be inferred from our data, our results indicate that the polyoma virus may be present in high-grade carcinoma more frequently than previously proposed. It may be appropriate in certain circumstances to exclude the coexisting polyoma virus with SV-40 immunohistochemical staining and / or PCR viral load.
29: Clinical outcome of patients with trisomy fluorescence in-situ hybridization results using UroVysion™
Shannon Brankley, CG(ASCP)CM, Jesse Voss, CT(ASCP), MB(ASCP), Michael Campion, BS, Emily Barr Fritcher, CT(ASCP), MB(ASCP), Kevin Halling, MD, PhD
Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota
Introduction: Fluorescence in-situ hybridization (FISH) with the UroVysion™ probe-set (consisting of chromosome enumeration probes to 3, 7, and 17 and a locus-specific identifier probe to 9p21) has been shown to have a high sensitivity for the detection of bladder cancer in patients with hematuria. Even as several studies have shown that a polysomy (i.e., ≥ 3 copies of ≥ 2 probes) FISH result is highly predictive of malignancy, very little data has been published showing a clinical correlation of patients with a trisomy FISH result (i.e., exhibiting three copies of a single probe). The aim of this study is to examine the clinical outcome of patients with a trisomy result on urine specimens analyzed by UroVysion™ FISH.
Materials and Methods: Electronic medical records were utilized to identify patients with a urine specimen diagnosed as the trisomy of chromosome 3, 7, or 17 (containing ≥ 10 cells) in the absence of multiple gains (i.e., polysomy or tetrasomy) that was analyzed by UroVysion™ FISH, as part of the clinical practice. Forty-five patient specimens, obtained between February 2001 and May 2008, were identified. Of the 45 patients, 18 patients (16 males and 2 females; median age, 71 years; range, 44 – 86 years) had follow-up data, including cytology and / or biopsy results. A positive cytology result and / or a histopathological diagnosis of carcinoma were considered to be evidence of malignancy.
Results: Trisomy of chromosome 7 was observed more often (67%; 12 / 18) than the trisomy of chromosome 3 (33%; 6 / 18). Four of the 12 (33%) patients with trisomy 7 and 2 / 6 (33%) patients with trisomy 3 were found to have malignancy at the time of FISH or on follow-up. All six patients presented with a histopathological diagnosis of superficial urothelial carcinoma (median, 26.5 days to diagnosis; range, 0 – 378 days), while 3 / 6 patients also had a positive cytology result on follow-up. One patient was diagnosed with superficial urothelial carcinoma 52 days after FISH and was later found to have invasive grade 2 (of 3) papillary urothelial carcinoma (389 days). Patients without evidence of malignancy were followed for a median of 580.5 days (range, 26 – 2014 days).
Conclusions: Even as the findings of this study indicate a positive predictive value of a trisomy FISH result, in the urine specimens it is low (33%). Our data also suggests that patients with a trisomy FISH result are unlikely to present with muscle invasive bladder cancer. Due to the infrequency of trisomy FISH results using the UroVysion™ probe-set, further studies are needed to fully understand the nature of this anomaly.
30: Fine needle aspiration of renal lesions in adults: A five-year retrospective study of 101 cases
Shaoxiong Chen, Harvey Cramer, Howard Wu
Pathology, Indiana University, Indianapolis, Indiana
Introduction: Fine needle aspiration (FNA) is a useful diagnostic tool for the assessment of patients presenting with renal tumors. With advances in neoadjuvant targeted therapy, the accurate subclassification of renal cell carcinoma by FNA is critical for selecting the appropriate treatment and for devising optimal strategies for patient follow-up. The aim of this study is to determine the accuracy of the subclassification of renal neoplasms by FNA.
Materials and Methods: A computerized search of our laboratory information system was performed for the five-year period, extending from January 2006 through March 2011, to identify all the FNA cases of renal lesions. The cytology reports, correlating the surgical pathology reports and related clinical histories were reviewed. The slides from all cases in which there was a discrepancy between the initial FNA diagnosis and the final histopathology were re-examined.
Results: A total of 101 renal lesions diagnosed by FNA were identified. The age of the patients ranged from 22 to 96 years (mean, 63 years). The male to female ratio was 1.2:1. The size of the renal lesions ranged from 1.2 cm to 20.8 cm (mean, 4.9 cm). The FNA diagnoses were classified as follows: Clear cell renal cell carcinoma (RCC) (15), papillary RCC (8), RCC, type not specified (21), urothelial carcinoma (9), angiomyolipoma (3), oncocytic neoplasms (8), other diagnoses (7), negative (14), and nondiagnostic (16). Histological correlation was available in 65 cases (64%), of which, eight of eight cases of clear cell RCC, six of six cases of papillary RCC, and seven of seven cases of urothelial carcinoma were confirmed histologically. Of the 20 cases of RCC, type not specified, the histological follow-up revealed clear cell RCC (nine), papillary RCC (four), unclassified RCC (four), chromophobe RCC (two), and non-diagnostic (one). Of the two cases of angiomyolipoma diagnosed by FNA, only one was confirmed histologically and the other revealed only benign renal parenchyma. All four cases of oncocytic neoplasms diagnosed by FNA revealed a discrepancy with the final histology including one case of carcinoid tumor, one case of unclassified RCC, and two cases of normal renal parenchyma. In one case, diagnosed as leiomyoma by FNA, the follow-up histology was angiomyolipoma. In two cases, the FNA diagnosis was poorly differentiated carcinoma and the correlating tissue showed renal cell carcinoma. In four cases, the FNA diagnosis was spindle cell neoplasm and the follow-up histology revealed one case of angiomyolipoma, two cases of sarcoma, and one case of sarcomatoid RCC. There were two false negative FNA cases that proved to be clear cell RCC by histology.
Conclusions: Overall, 72% (47 / 65) of the cases with histology follow-up were diagnosed correctly by FNA. A correct subclassification of the renal neoplasm was rendered in 21 cases (32%) including clear cell RCC (eight), papillary RCC (six), and urothelial carcinoma (seven). The false negative and nondiagnostic cases were attributed to sampling error. In two cases, misinterpretation of the proximal tubular epithelial cells contributed to the false positive diagnoses of oncocytic neoplasm. The cytological diagnosis of angiomyolipoma was challenging, with only one of the four cases being accurately diagnosed by FNA. To maintain the clinical relevance of this diagnostic technique in the era of modern targeted therapy, further improvements in the accuracy of the cytological diagnosis and classification of renal tumors by FNA will be necessary.
31: Urothelial cell carcinoma cytology-histology correlation: Are we missing hypochromatic high grade urothelial carcinomas?
Ghada Aramouni, CT(ASCP), Debbie Sabo, CT(ASCP), Deborah Chute, MD
Department of Anatomic Pathology, Cleveland Clinic Foundation, Cleveland, Ohio
Introduction: Urine cytology is the primary screening test for urothelial carcinoma. It has a high sensitivity for high-grade urothelial carcinomas, but is less useful in the diagnosis of low-grade urothelial carcinoma. This is due to the improved criteria for the diagnosis of high-grade urothelial carcinoma: High nuclear to cytoplasmic ratio, hyperchromasia, coarse chromatin, and nuclear membrane irregularities. However, some cases of biopsy-proven high-grade urothelial carcinoma are not identified by urine cytology.
Materials and Methods: A cytological-histological correlation search was performed over five years for all urine cytology specimens (voided, instrumented, or washing) with a urothelial tract biopsy accessioned within three days of the index urine. Only cases with biopsy-proven high-grade urothelial carcinoma were included. The original cytology slides (all ThinPrep®) were reviewed by two cytotechnologists, for the presence or absence of atypical urothelial cells and acute inflammation. The number of atypical urothelial cells was quantified as < 5 or ≥ 5. The atypical urothelial cells were qualitatively assessed for nuclear chromatin quality and considered as either hyperchromatic [Figure 1] or hypochromatic [Figure 2]. Photomicrographs of examples of hyperchromatic and hypochromatic atypical cells were provided to the reviewers for comparison and standardization. For statistical analysis, suspicious and positive urine cytology cases were combined into a ‘positive’ category, as this would trigger further management at our institution. All other diagnoses were combined into a ‘negative’ category.
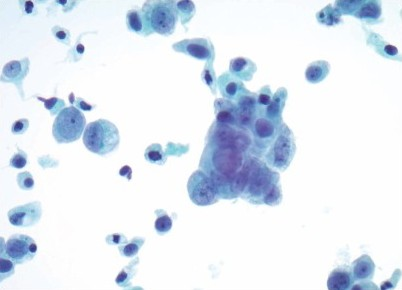
- Hyperchromatic atypical urothelial cell
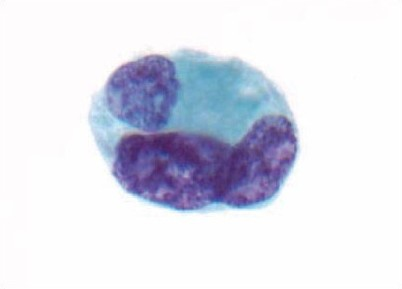
- Hypochromatic atypical urothelial cells
Results: A total of 132 urine cytology cases with a concurrent positive biopsy were available for review. The breakdown of original cytology diagnosis was: Negative 25%, atypical 25%, cannot exclude urothelial carcinoma 5%, suspicious 14%, and positive 30%. Twelve cases (9%) lacked atypical cells, all of which were originally interpreted as negative, and excluded from further analysis. There was no significant association of cytology diagnosis with the method of collection or the presence of inflammation. Thirty-eight cases (31%) lacked hyperchromatic atypical cells (hypochromatic only), of which 10 cases were originally called suspicious or positive. The absence of hyperchromatic atypical cells was significantly associated with a ‘negative’ diagnosis (P < 0.001) [Table 1]. Twenty-two cases (18%) had < 5 atypical urothelial cells present, none of which were originally called suspicious or positive. The presence of > 5 atypical urothelial cells was significantly associated with a ‘positive’ diagnosis (P < 0.001) [Table 2]. When all cases with < 5 atypical urothelial cells were excluded from the analysis, the absence of hyperchromatic atypical cells trended toward a significance for association with a ‘negative diagnosis (P = 0.07).
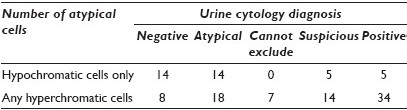
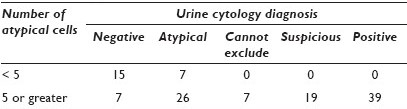
Conclusions: In patients with known high-grade urothelial carcinoma, at the time of urine cytology sampling, low numbers of atypical cells are the strongest predictors of a ‘negative’ urine cytology diagnosis. However, a significant number of high cellularity samples contain atypical urothelial cells with hypochromatic chromatin. We propose that a subset of urothelial cell carcinomas exfoliate hypochromatic cells, which may be missed out on urine cytology.
32: Lymphoepithelioma-like carcinoma of the urinary bladder: Cytopathological findings and differential diagnosis on urinary cytology
Hui Guan, MD, PhD1, Syed Ali, MD2
1Pathology, The Johns Hopkins Hospital, Baltimore, Maryland; 2Pathology and Radiology, The Johns Hopkins Hospital, Baltimore, Maryland
Introduction: Lymphoepithelioma-like carcinoma (LELC) of the urinary bladder is a rare variant of high-grade urothelial carcinoma (UC) accounting for less than 1.3% of all bladder carcinomas. As the name suggests, LELC displays phenotypic resemblance to nasopharyngeal lymphoepithelioma. There are only rare published accounts of the cytopathological features of LELC of the bladder.
Materials and Methods: All urinary cytology cases of biopsy / resection-proven LELC from a 14-year period (1997 – 2011) were retrieved from the archives of a large university hospital. Slides were prepared by SurePath® methodology. Both the cytological and histological material was reviewed and the morphological characteristics were analyzed.
Results: A total of eight patients were identified with an age range of 63 to 88 years (mean age, 77) with a male : Female ratio of 2 : 1. None of the cases was diagnosed on cytology as LELC. Retrospectively, in six of eight cases, the lesional cells were identified. The cytological diagnoses were ‘atypical cells’ (5) and ‘suspicious for urothelial carcinoma’ (1). The salient cytomorphological features included rare large, pleomorphic cells with high N / C ratios and nuclei with an open / vesicular chromatin pattern containing single prominent nucleoli. The predominant pattern was single cells with only two cases showing cellular fragments. All cases showed a variable presence of intermingled lymphocytes. Necrosis was not seen.
Conclusions: A definitive urinary cytology diagnosis of LELC is not possible and most of the cases are interpreted as ‘atypical’. LELC shows only rare malignant cells and a variably increased lymphocytic population. A definitive diagnosis is only established on histological material. LELC may be included in the differential diagnosis of atypical urothelial cells with vesicular chromatin and prominent nucleoli, particularly when these cells are intermixed with lymphocytes.
33: Cytological and cystoscopic predictors of recurrence and progression in patients with low- grade urothelial carcinoma
Julie Jackson, MD, Güliz Barkan, MD, Umesh Kapur, MD, FASCP, Eva Wojcik, MD, MIAC
Pathology, Loyola University Medical Center, Maywood, Illinois
Introduction: Patients with low-grade urothelial carcinoma (LGUC) are at risk of recurrence and must undergo lifelong surveillance. To date, cytology and cystoscopy are the gold standard for the detection of de novo and recurrent urothelial carcinoma (UC). Our aim is to further characterize the role of cytology and cystoscopy in determining the risk of recurrence and progression in these patients.
Materials and Methods: Patients with a diagnosis of LGUC on bladder biopsy specimens or transurethral resection of bladder tumor (TURBT) specimens with corresponding urine cytology performed within two months prior to diagnosis were identified between 2006 and 2010 at our institution. Electronic medical records were reviewed for cystoscopic findings, and histological and cytological follow-up data, from the time of biopsy to the present. Chi-square and Fisher Exact tests were used for statistical analysis as appropriate.
Results: The study was comprised of 106 cases from 86 patients (mean age, 71; range, 27 – 89; 57 males, 29 females). Cytology was negative in 68 (64%), positive for UC in 10 (9%), atypical in 20 (19%), suspicious in six (6%), and unsatisfactory in two (2%) cases. On cystoscopy, a single lesion was found in 55 (52%) cases, multiple lesions in 48 (45%), and no lesions were seen in three (3%). In 58 cases with documented lesion sizes in a cystoscopy report, 22 (38%) showed lesions ≥ 2 cm. Of 94 cases with follow-up histological data, recurrence of UC (either high-grade or low-grade UC) was demonstrated in 51 (54%), recurrence of LGUC in 40 (42%), progression to high-grade urothelial carcinoma (HGUC) in 28 (29%), and no histological recurrence was demonstrated in 40 (42%) cases, during the study period. The initial urine cytology tended to be positive / suspicious when cystoscopic lesions were ≥ 2 cm rather than < 2 cm (5 / 22 (23%) cases, versus 2 / 36 (6%), respectively, P = 0.092). Of 96 cases with cytological follow-up data available, patients tended to have abnormal cytology (atypical or above) on future surveillance when > 1 lesion rather than when ≤ 1 lesions were present (28 / 42 (67%), versus 26 / 54 (48%), respectively, P = 0.070). Patients more often developed recurrent UC (either HGUC or LGUC) when > 1 lesions rather than ≤ 1 lesions were seen on cystoscopy (30 / 42 (71%), versus 21 / 52 (40%), respectively, P = 0.003). Finally, recurrence of UC (either HGUC or LGUC) was more likely when initial urine cytology was positive / suspicious rather than negative or atypical (12 / 15 (80%), versus 40 / 79 (51%), P = 0.048). More specifically, development of HGUC was more likely during the follow-up period when initial cytology was positive / suspicious rather than negative or atypical (8 / 15 (53%), versus 20 / 79 (25%), P = 0.030).
Conclusions: In conclusion, our data shows that the cystoscopic findings, including size of bladder lesions ≥ 2 cm, presence of multiple lesions, as well as positive urine cytology, at or shortly prior to the time of diagnosis of LGUC, predict recurrence or progression of the disease.
34: Correlation of UroVysion® FISH test results with histological findings
Dorota Rudomina, MBA, CT(ASCP), Oscar Lin, MD, PhD
Cytology, Memorial Sloan-Kettering Cancer Center, New York
Introduction: UroVysion® is a fluorescent in-situ hybridization (FISH) probe set, which has been approved by the FDA for use in monitoring tumor recurrence in patients with a history of urothelial carcinoma (UC) and screening for UC in patients with hematuria. The UroVysion® test probe set contains fluorescent labeled DNA probes to the centromeres of chromosomes 3, 7, and 17, and a locus-specific probe to the 9p21 band. The probes for the centromeres of chromosomes 3, 7, and 17 detect the hyperploidy of these chromosomes, a common feature of high-grade UC, in-situ and invasive; while homozygous deletion of the p16 gene at 9p21 is believed to be one of the most common alterations in UC and occurs early in the development of papillary UC and UC in-situ. The test has a reported sensitivity ranging from 65 to 73% for pTa and 95 to 100% for pT1-T4 urothelial carcinomas. The objective of this study is to evaluate the correlation of the cytogenetic abnormalities found in the cytology specimens that have positive UroVysion® results with UC grade and invasion in the surgical specimens.
Materials and Methods: The cases selected for this study included cases with positive UroVysion® tests and a positive biopsy within six months of the UroVysion® test. This cohort consisted of 159 cases represented by 15 low-grade UC and 144 high-grade UC (71 invasive and 73 in-situ). The UroVysion® results were considered positive according to the manufacturer's guidelines. A quantitative analysis correlating 9p21 deletions and CEP 3, 7, 17 gains in low-grade papillary UC (LGPUC), in-situ high-grade UC, and invasive UC was performed.
Results: The prevalence of 9p21 homozygous / heterozygous deletions and CEP 3, 7, 17 gains in low-grade papillary UC, in-situ high grade UC, and invasive UC are summarized in Table 1.
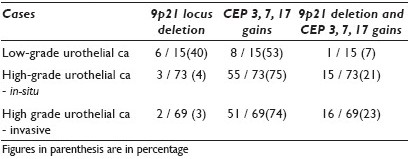
Conclusions: Deletion of 9 p21 is noted in approximately 40% of the cases of LGPUC, while gains in chromosomes 3, 7 or 17 are present in approximately half the cases of LGPUC. Deletion of 9p21 is rarely seen simultaneously with gains in chromosomes 3, 7 or 17 in LGPUC. Furthermore, the presence of 9p21 deletion in the absence of gains in chromosomes 3, 7 or 17 suggests LGPUC. The presence of gains for chromosomes 3, 7 and 17 does not predict UC grade or invasion status. High-grade UC, either in-situ or invasive, is cytogenetically similar when using the UroVysion® test probe set.
35: Dysplastic squamous cells in urine predict malignancy in the absence of urothelial atypia
Beatriz Sanchez, MD, Umesh Kapur, MD, Güliz Barkan, MD, Grazina Chatt, CT(ASCP), Eva Wojcik, MD
Cytopathology, Loyola University Medical Center, Maywood, Illinois
Introduction: The presence of dysplastic squamous cells (DSCs) in the urine in the absence of urothelial cells, although an uncommon finding, may indicate an underlying malignant process either in the urinary or gynecological tract. Finding DSCs in the urine may precede a de novo histological diagnosis of malignancy or be the first sign of a recurrence. The aim of our study is to demonstrate the clinical significance of urine cytology with dysplastic squamous cells.
Materials and Methods: Cytology specimens with diagnoses of dysplastic squamous cells, without urothelial atypia, were identified over a period of four years (2007 – 2010). Electronic medical records (EMR) were examined for clinical follow-up, age, gender, follow-up biopsy or cytology (if applicable), and the time interval between the diagnosis of DSCs and biopsy.
Results: Thirty-eight cases of DSCs were identified (voided urine-18, bladder barbotage-19, and neobladder-1). The male : female ratio was equal and the age ranged from 21 to 81 years (mean, 53 years). Hematuria (n = 36 / 38) was the most common presenting symptom. Surgical biopsy diagnosis was available in 17 / 38 (45%) of the patients. Fifteen of the seventeen had a urinary bladder biopsy that showed a wide spectrum of squamous lesions, including squamous metaplasia with low-grade dysplasia (5), infiltrating squamous cell carcinoma of urinary bladder (3), and high-grade papillary urothelial carcinoma with squamous differentiation (3). In addition, infiltrating squamous cell carcinoma was identified in three other patients (vulva-1, penile-1, and anus-1). The remaining two patients had a benign diagnosis. Twelve patients who followed up with repeat urine cytology alone (two weeks up to one year) had a benign diagnosis. Nine of 38 (24%) patients who only received clinical follow-up had negative cystoscopy and negative fluorescence in-situ hybridization.
Conclusions: Dysplastic squamous cells, even in the absence of atypical urothelial cells, are a strong predictor of urinary tract malignancy. Follow-up of DSCs should include genitourinary tract examination.
36: The significance of cellular clusters in urine cytology after cystectomy
Leah Schultz, CT(ASCP)CM, Jamie Covell, CT(ASCP), Kristen Atkins, MD
Pathology, University of Virginia Medical Center, Charlottesville, Virginia
Introduction: Cystectomy for bladder cancer is typically done for invasive high-grade urothelial carcinoma. Routine surveillance by urine cytology from the neobladder or ileal conduit usually demonstrates numerous degenerating glandular cells and histiocytes. Occasionally larger papillary-like clusters of low-grade cells are seen, but the significance of these findings as an indicator of recurrent disease in this setting is uncertain.
Materials and Methods: A computer search of the Cytology Laboratory records (July 1998 – February 2010) identified 424 post cystectomy urine specimens: 351 (83%) were interpreted as negative for malignancy, 56 (13%) were with clusters of atypical cells, and 17 (4%) were diagnosed as recurrent carcinoma. This study focused on urine specimens from the atypical and malignant categories, which were reviewed for cytomorphological features and follow-up. Records of the original tumor diagnoses for these cases were noted. Immunohistochemistry was performed on some recent cases in an attempt to identify the origin of the clusters of atypical cells.
Results: Review of the pathology reports of primary tumors showed high-grade invasive urothelial carcinoma in all patients; however, a few patients also had concurrent low-grade papillary urothelial carcinoma. Sixteen of the seventeen urine samples classified as malignant had high-grade cytology: Enlarged nuclei, high N : C ratios, hyperchromasia, and marked anisonucleosis. One specimen showed numerous papillary-like clusters of cells with a more bland cytological appearance. This case had no follow-up confirmation of malignancy and could represent a false-positive interpretation. Specimens reported with atypical clusters showed two patterns. The most frequently seen pattern was clusters of cells characterized by cells with relatively low N : C ratios, eccentrically-placed nuclei, crinkled nuclear contours, and cytoplasmic vacuoles. The second, less common pattern, contained rare atypical cells with some features similar to the overtly malignant cells, but the findings were insufficient for a definitive interpretation of recurrence. Two cases from the atypical group had documented recurrent carcinoma. Review of their cytology showed clusters of cells with minimal nuclear atypia in one case and rare markedly atypical single cells in the second case. The remaining cases had benign follow-up and / or negative imaging. Immunohistochemistry performed in four recent cases demonstrated strong CK 20 and CD 68 positivity in the papillary-like cell clusters.
Conclusions: Papillary-like clusters of cells with relatively low N : C ratios, crinkled nuclear contours and vacuolated cytoplasm most commonly represent degenerated small bowel glandular cells rather than neoplastic urothelial cells. These cell clusters are potential pitfalls in the overdiagnosis of atypical urothelial cells and can lead to increased unnecessary screening. Most cystectomy procedures are performed for high-grade urothelial carcinoma and recurrences are typically similar high-grade lesions, which present with high-grade cytological features in urine specimens.
37: Category performance and morphological criteria of atypical urothelial cells, cannot exclude high-grade urothelial carcinoma
Christopher VandenBussche, MD, PhD1, Christopher Owens, MD2, Frances Burroughs, SCT(ASCP)1, Douglas Clark, MD1, Dorothy Rosenthal, MD1
1Pathology, The Johns Hopkins Hospital, Baltimore, Maryland; 2Pathology, UMass Memorial Medical Center, Worcester, Massachusetts
Introduction: In most cytopathology laboratories, urinary tract (UT) samples are second only to Pap tests in annual volume. We previously designed a template in order to standardize our UT diagnostic categories to enable our clinicians to uniformly manage their patients. We now examine the clinical utility of one of the two atypical categories, atypical urothelial cells, suspicious for high-grade urinary carcinoma (AUC-H), as well as specific cytological features found in these specimens that are most predictive of high-grade urothelial carcinoma (HGUC).
Materials and Methods: Of the 725 patients diagnosed with atypical cells (atypical urothelial cells of uncertain significance (AUC-US or AUC-H) on urine cytology, between July 2007 and June 2009, 58 were diagnosed by our faculty as having at least one sample with AUC-H; eight patients had two samples. A total of 62 specimens were available for review. A junior and senior pathologist blindly and separately evaluated each of the specimens for individual cytological criteria and predicted whether each sample represented HGUC. Nine cytological; criteria were selected, which were thought to be the most predictive. The predictions were then matched with the follow-up biopsy outcomes, which were tracked over 18 months following the July 2009 cutoff, for inclusion in the study. The hospital laboratory information system was searched for cases that met the following criteria for the period from July 1, 2007 to June 30, 2009: (1) All cytological specimens with a diagnosis of AUC-US or AUC-H; (2) any follow-up surgical specimens resulting from the diagnosis rendered in (1); the specimens in (1) and (2) were then matched following a blind review of the cytological specimens; (3) all surgical pathology specimens with a diagnosis of high-grade urothelial carcinoma, regardless of invasion status; (4) all preceding cytological specimens from patients identified in (3); and (5) total urinary cytology samples for the same period.
Results: Of the nine cytological criteria that were selected, the four most commonly seen in AUC-H specimens were: Hyperchromatic nuclei (71%), irregular nuclear borders (66%), increased N / C ratio (56%), and anisonucleosis (55%). A large proportion of specimens (74%) contained abnormal cells meeting these multiple criteria. Enlarged nuclear size, a characteristic feature of HGUC specimens, was not a common feature in AUC-H specimens. Once the follow-up data were unmasked, all but two patients (97%) with AUC-H specimens were ultimately diagnosed with HGUC in the corresponding surgical pathology material. The small number (n = 2) of AUC-H patients with a benign follow-up diagnosis did not allow for statistical comparison of how predictive the selected criteria were for HGUC at this stage in our study.
Conclusions: Patients with an AUC-H diagnosis had a high rate (97%) of having HGUC on follow-up biopsy. The AUC-US category has a much lower predictive value of HGUC than AUC-H, but is a more common diagnosis. We are currently examining how the cytologic criteria identified in the AUC-H cohort will perform in this larger group (n = 667) of patients with an AUC-US diagnosis, to predict an outcome diagnosis of HGUC.








