Translate this page into:
Cytodiagnosis of extramedullary hematopoiesis in serous effusion: A rare presentation unfolding the underlying etiology
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Extramedullary hematopoiesis (EMH) usually involves reticuloendothelial system. However, it rarely may be present in the serous body effusions. In our case, the fluid cytology of both peritoneal and pleural fluid was diagnostic of the EMH in a patient with an undiagnosed underlying etiology.
Keywords
Cytology
effusion
extramedullary hematopoiesis
peritoneal fluid
pleural fluid
serous
INTRODUCTION
Extramedullary hematopoiesis (EMH) is defined as the presence of normal hematopoietic marrow elements outside the bone marrow. It occurs most often due to hemolytic anemias; it may be seen in prolonged iron deficiency anemia, chronic myeloproliferative disorders, leukemia, and lymphoma.[12] EMH predominantly involves reticuloendothelial system. EMH rarely involves the serous body fluids. We report a rare case of EMH diagnosed primarily on fluid cytological examination, involving both peritoneal and pleural fluids, which eventually led to unraveling of an underlying chronic myeloproliferative disorder.
CASE REPORT
A 58-year-old male presented to medicine outpatient department with complaints of abdominal distension, loss of appetite, and weight loss for the last 2–3 months. The patient had midline neck swelling for the last 15 years which approximately measured 4 cm × 4 cm and was firm, nodular, and nontender. There was no history of fever, cough with or without expectoration, hematemesis, melena, loss of consciousness, or altered sensorium. The patient was not a known case of diabetes mellitus, hypertension, or any other chronic systemic illness. He had no history of tuberculosis or any history of contact for the same. On general examination, the patient was conscious and well oriented. His blood pressure and pulse rate were within normal limits as per his age. However, pallor was noted. He did not have icterus, clubbing, cyanosis, pedal edema, peripheral palpable lymphadenopathy, and his jugular venous pressure was also not raised.
Per abdominal examination revealed moderate hepatosplenomegaly and ascites. Rest of the systems examined did not reveal any abnormality.
Thyroid function tests showed elevated levels of thyroid-stimulating hormone: 21.005 pg/ml (normal - 0.55–4.78 pg/ml) and decreased levels of free-T3: 1.3 pg/ml (normal: 2.3–4.2 pg/ml) and T4: 0.58 ng/dl (normal: 0.89–1.76 ng/dl). Other routine biochemical parameters were within normal limits.
Hemogram of the patient showed hemoglobin - 8.8 g/dl, total leukocyte count - 16,200/μL, and platelets - 2.6 lakhs/μL. Peripheral blood smear examination showed leukocytosis with the presence of immature cells of myeloid series (differential leukocyte count as: myelocytes - 17%, metamyelocytes - 10%, polymorphs - 46%, lymphocytes - 21%, monocytes - 02%, basophils - 02%, eosinophils - 02%). Five nucleated red blood cells were noted per 100 white blood cells. Red blood cells showed mild anisocytosis with the presence normocytic normochromic to microcytic hypochromic cells. Few tear drop cells and polychromasia were also noted. Overall findings were of leukoerythroblastic blood picture.
Bone marrow aspiration examination was done. However, bone marrow smears were markedly diluted with peripheral blood showing few maturing cells of myeloid and erythroid series. Bone marrow biopsy obtained was inadequate.
Ultrasound of neck and abdomen was done. Thyroid was diffusely enlarged with multiple heteroechoic nodules (largest measuring 39 mm × 36 mm) seen scattered diffusely in the thyroid with peripheral calcification, suggestive of multinodular goiter. Ultrasound of the abdomen revealed hepatosplenomegaly and gross ascites with omental caking and peritoneal thickening which was suggestive of tubercular etiology keeping in with the high incidence of tuberculosis in India [Figure 1a]. Hence, the patient was further investigated for tuberculosis with ancillary tests but showed negative results (ascitic fluid adenosine deaminase level - 10.0 [normal <40 U] and negative Montaux test). Chest X-ray showed evidence of bilateral pleural effusion with focal consolidation.
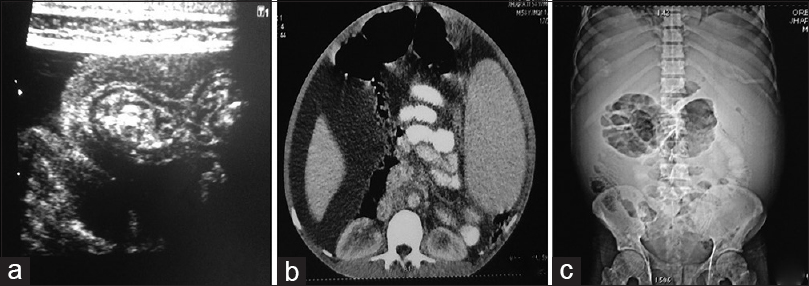
- (a) Ultrasonography abdomen showing omental caking and peritoneal thickening. (b) Computed tomography image revealing ascites, hepatosplenomegaly, and thickened peritoneum. (c) Contrast-enhanced computed tomography image shows ascites, bilateral pleural, and mild pericardial effusion
Further, contrast-enhanced computed tomography (CECT) abdomen and chest showed evidence of chronic liver disease with portal hypertension (portal vein pressure 20 mm Hg), hepatosplenomegaly, and few retroperitoneal lymph nodes. Gross ascites along with thickened peritoneum were also noted [Figure 1b]. CECT chest revealed bilateral moderate pleural effusion with underlying segmental lung collapse and consolidation. Moderate pericardial effusion was also found [Figure 1c].
Fine-needle aspiration cytology of thyroid swelling was revealed benign cytology with calcified material and debris in a background of thin colloid. Ascitic fluid was sent for the cytological examination. Grossly, 2 ml of thin blood mixed fluid was received. Multiple smears prepared after cytocentrifugation and were air dried and fixed in 95% ethyl alcohol and subsequently stained with Giemsa and Papanicolaou stain, respectively. Smears were highly cellular and revealed all the three lineages of hematopoietic cells with a predominance of myeloid series cells which were seen in all stages of maturation along with occasional cells of erythroid series and many megakaryocytes [Figure 2a]. The morphology of megakaryocytes was clearer in Papanicolaou-stained smears revealing multiple distinct nuclei [Figure 2b]. Furthermore seen were many mature lymphocytes, few reactive forms, plasma cells, and histiocytes in a thin hemorrhagic background. Few of the histiocytes showed evidence of emperipolesis. Cell block was prepared from the peritoneal fluid which also showed evidence of EMH [Figure 2c]. Based on the cytomorphological findings, a diagnosis of EMH in peritoneal fluid was given. Cytological examination of pleural fluid was also consistent with EMH.
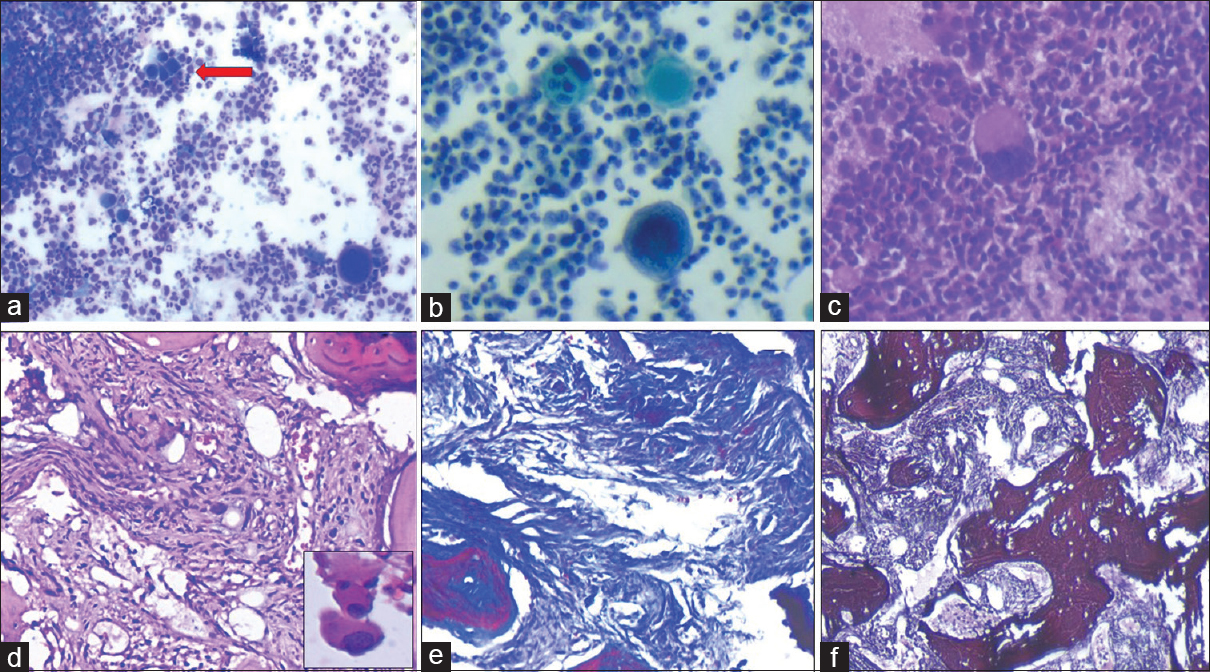
- (a) Cellular smear showing numerous myeloid cells in various stages of maturation, occasional group of erythroid cells (red arrow), and scattered megakaryocytes (Giemsa, ×200). (b) Large multinucleated and multilobulated megakaryocytes (Pap, ×400). (c) Cell block section revealing scattered megakaryocytes along with numerous myeloid series cells (H and E, ×200). (d) Bone marrow biopsy shows markedly hypocellular marrow with diffuse fibrosis of marrow spaces (H and E, ×200). Inset shows megakaryocytes. (e) Fibrotic areas show increase in reticulin with extensive intersection (reticulin, ×200). (f) Masson's trichrome stain showing diffuse blue-stained coarse bundles of collagen (MT, ×200)
Cytological diagnosis urgently prompted a relook in the radiological and the hematological workup and a repeat bone marrow aspiration and biopsy was done. Smears were again markedly diluted with blood with sparse myeloid and erythroid cells. However, megakaryocytes were easily noted. However, bone marrow biopsy showed markedly hypocellular marrow with diffuse fibrosis of marrow spaces and focal vascular proliferation [Figure 2d]. Few megakaryocytes were seen [Figure 2d; inset]. Reticulin stain showed diffuse and dense increase in reticulin with extensive intersection [Figure 2e]. Coarse bundles of collagen were seen diffusely staining blue on Masson's trichrome stain [Figure 2f]. A diagnosis of primary myelofibrosis (PMF) was given.
A radiologic relook also was consistent with the possibility of EMH mimicking tuberculosis. Liver biopsy was done to evaluate the patient, based on the CECT findings for any association with cirrhosis. Histology showed evidence of EMH and no evidence of cirrhosis was noted. Simultaneously, molecular testing for BCR-ABL rearrangement (polymerase chain reaction quantitative) and for JAK2 V617F mutation showed negative results. Finally, a diagnosis of PMF with EMH was made.
The patient was mainly given supportive treatment, the drug Carvedilol (3.125 mg twice a day) for the portal hypertension and the patient was referred to a higher oncology center for further management.
DISCUSSION
EMH has been noted in association with chronic anemias, more with hemolytic anemias such as sickle cell disease and thalassemia, rarely with prolonged iron deficiency anemia.[12] It may also be seen with chronic myeloproliferative disorders such as chronic myeloid leukemia, PMF with myeloid metaplasia, or secondarily with leukemia/lymphoma infiltration in the bone marrow.[12]
EMH is usually noted in reticuloendothelial organs such as spleen, liver, and lymph nodes and may also involve other sites such as kidneys, adrenals, gastrointestinal tract, lung, breast, skin, joints, posterior mediastinum, pleura, pericardium, and brain.[123] Very rarely, EMH can present as gastrointestinal masses which may adhere to adjacent structure resulting in obstructive and neurological symptoms.[3]
EMH in serous fluids has been reported rarely with few case reports in literature.[34567] EMH in pleural fluid is more rare than in peritoneal fluid. In our case, both peritoneal and pleural fluid involvement was seen with EMH.
The omental thickening noted on ultrasonography of abdomen in our patient pointed toward tubercular etiology. However, ancillary investigations done excluded the diagnosis of tuberculosis. It was possibly the omental implants of EMH. Luo et al.[5] reported similar case of bilateral pleural effusion in a patient with extensive EMH where the clinical presentation mimicked tuberculosis.
The pathogenesis of ascites can be due to portal hypertension or peritoneal and ectopic hematopoiesis.[67] EMH may occur either by rupture of myeloid nodules from liver/spleen or other abdominal organs or by myeloid metaplastic process involving the peritoneal surface.[67] Exfoliation of megakaryocytes and myeloid cells into the peritoneal and pleural space from their respective deposits is the most likely mechanism for cytological findings in the fluid.
The presence of ascites and pleural effusion is not frequently seen with myelofibrosis which was possibly the cause for not suspecting a myeloproliferative disorder primarily.[5] Very few cases have been reported in literature which describe the cytologic findings of EMH in patients with myelofibrosis and having both peritoneal and pleural effusion.[5678]
It is important to evaluate to rule out the presence of any reactive/malignant mesothelial cells, histiocytes, metastatic carcinoma, metastatic sarcoma, and other hematopoietic disease including Hodgkin disease and multiple myeloma.[3] Immunohistochemistry can be useful in differentiating these in cases with morphological dilemma. Usually, JAK2 V617F mutation is present in 60% of PMF. In our case, JAK 2V 617F mutation was negative adding to the rarity of our case.
The mainstay of treatment of PMF is administration of steroids.[8910] In spite of recent advances in management of PMF, there has been no overall improvement in the survival of these patients. However, palliative measures, such as splenectomy or radiotherapy, can be provided to the young symptomatic patients. Sometimes, allogenic stem cell transplantation can be useful.
CONCLUSION
The present case reiterates the importance of diagnostic cytomorphological features of EMH in peritoneal and pleural fluid. The presence of EMH in serous fluids may be an initial pointer toward a primary hematological pathology. Further, the case also highlights the uncommon presentation of peritoneal and pleural fluid effusion in JAK2 V617F mutation negative PMF.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interest.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE. Each author has participated sufficiently in work and takes public responsibility for appropriateness of content of this article.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from institutional Review Board (IRB).
LIST OF ABBREVIATIONS (In alphabetic order)
CECT - Contrast-enhanced Computed Tomography
EMH - Extramedullary Hematopoiesis
PMF - Primary Myelofibrosis
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Extramedullary hematopoiesis in the adrenal: Case report and review of literature. Can Urol Assoc J. 2013;7:E436-8.
- [Google Scholar]
- Cutaneous extramedullary hematopoiesis in a patient with idiopathic myelofibrosis. J Dermatol. 2008;35:456-61.
- [Google Scholar]
- Intestinal obstruction caused by extramedullary hematopoiesis and ascites in primary myelofibrosis. World J Gastroenterol. 2014;20:11921-6.
- [Google Scholar]
- Ascites and pleural effusion secondary to extramedullary hematopoiesis. Am J Med Sci. 1999;318:286-8.
- [Google Scholar]
- Bilateral pleural effusion in a patient with an extensive extramedullary hematopoietic mass. Case Rep Hematol. 2013;2013:857610.
- [Google Scholar]
- A 62-year-old woman with bilateral pleural effusions and pulmonary infiltrates caused by extramedullary hematopoiesis. Respiration. 2009;78:110-3.
- [Google Scholar]
- Pleural fluid extramedullary hematopoiesis case report with review of the literature. Diagn Cytopathol. 2016;44:41-4.
- [Google Scholar]
- A patient with myelofibrosis complicated by refractory ascites and portal hypertension: To tips or not to tips?. A case report with discussion of the mechanism of ascites formation. Scand J Gastroenterol. 2004;39:389-94.
- [Google Scholar]
- New prognostic scoring system for primary myelofibrosis based on a study of the international working group for myelofibrosis research and treatment. Blood. 2009;113:2895-901.
- [Google Scholar]
- Idiopathic myelofibrosis with refractory massive ascites. Intern Med. 2003;42:525-8.
- [Google Scholar]








