Translate this page into:
Cytodiagnosis of scalp swelling: An uncommon presentation of a common neoplasm

*Corresponding author: Garima Rakheja, MD, DNB Department of Pathology, Government Medical College and Hospital, Sector 32, Chandigarh, Punjab, India. garima.rakheja@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rakheja G, Agrawal N, Handa U, Palta A. Cytodiagnosis of scalp swelling: An uncommon presentation of a common neoplasm. CytoJournal 2020;17:26.
CLINICAL HISTORY
A 56-year-old male presented with complaint of swellings on the scalp for a month. On examination, two swellings were identified in the left parietal and the occipital region, measuring 5 × 4 cm and 3 × 3 cm, respectively. The contrast-enhanced computed tomography scan revealed soft-tissue densities in relation to the calvarium, with underlying bone erosion and intracranial extension [Figure 1c]. Smears from the fine-needle aspirate cytology (FNAC) procedure performed are shown [Figure 1a and b].
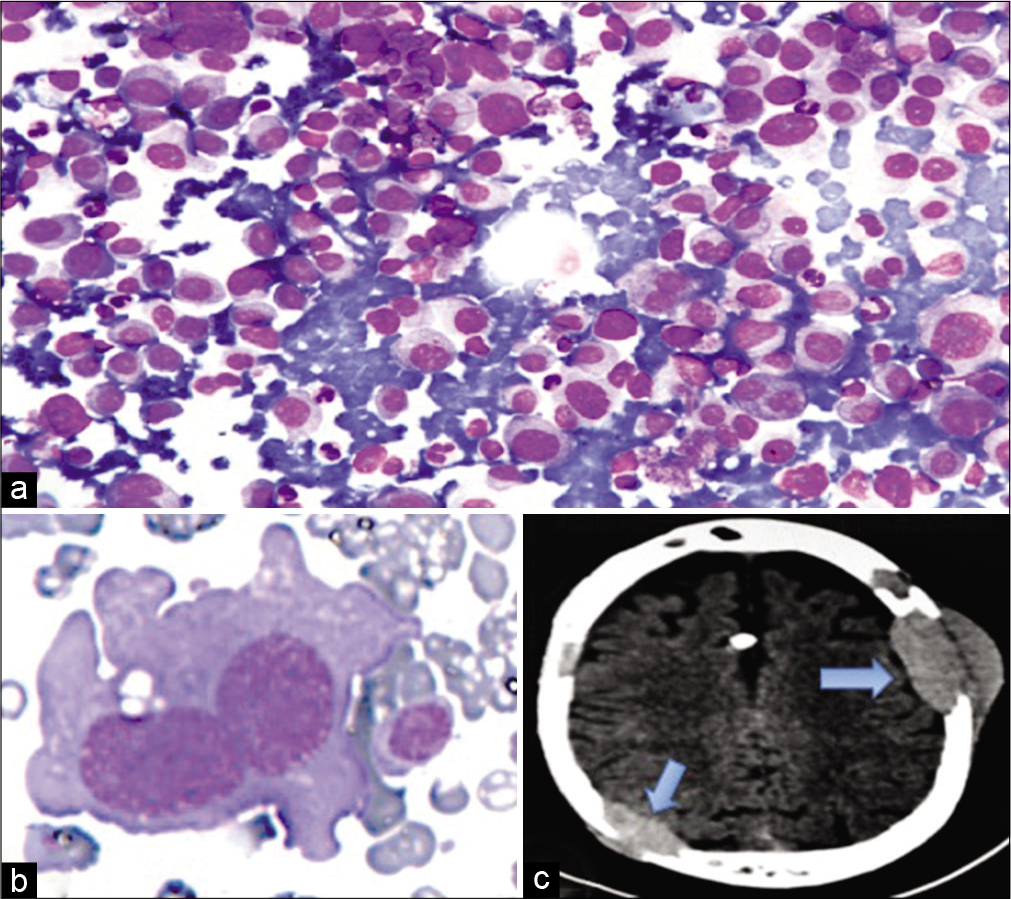
- (a) Fine-needle aspirate cytology smear shows numerous mature plasma cells, few immature form, lymphocytes, and bare nuclei (MGG stain, ×400). (b) Flame cell (MGG stain, ×1000). (c) Axial cranial CT reveals osteolytic extradural soft-tissue masses (arrowhead) involving the diploe of the calvarium, with cortical defects and intracranial extension.
QUESTION
What is your interpretation?
Plasma cell granuloma
Non-Hodgkin’s lymphoma
Plasmacytoma
Syringocystadenoma papilliferum
Answer
The correct cytopathological interpretation is:
(c) Plasmacytoma
The cytology smears show a dispersed population of cells having round, eccentric nucleus, with coarsely clumped chromatin, inconspicuous nucleolus, and dense cytoplasm with perinuclear hof, conforming to the morphology of mature plasma cells [Figure 1a]. Also observed were immature plasma cells having a single large nucleus and prominent nucleolus. Apart from these, binucleate, multinucleate forms, and flame cells were noteworthy [Figure 1b].
Non-neoplastic proliferation of plasma cells is usually seen in association with mixed inflammatory cells such as lymphocytes and neutrophils. Plasma cell granuloma, also known as inflammatory pseudotumor, is a fibroblastic/ myofibroblastic lesion cytologically characterized by the presence of spindle cells accompanied by an inflammatory infiltrate of numerous plasma cells, lymphocytes, and few eosinophils. Although rare in soft tissue, it has been reported most commonly in lungs, oral cavity, gingival mucosa, etc.
Some non-Hodgkin lymphomas, in particular, high-grade malignant immunoblastic lymphoma and marginal zone B-cell lymphoma may depict plasmacytoid morphology, posing a morphological dilemma. However, possibility of non-Hodgkin’s lymphoma is excluded by a characteristic absence of lymphoglandular bodies in the background.
Some cutaneous adnexal tumors, such as syringocystadenoma papilliferum, show numerous plasma cells on FNA smears. This entity is superficial, limited to the skin, and presents clinically as a nodular, warty tumor or as ulcerated lesion of the scalp, neck, and face. In addition to the plasma cells, the smears also show cohesive aggregates of epithelial cells, with focal papillary configuration.
FOLLOW-UP OF THE PRESENT CASE
Further investigations revealed mild anemia (Hb 8.7 g/dL), hypercalcemia (11.3 mg/dL), and deranged renal function (creatinine 11 mg/dL and urea 45 mg/dL). Bone marrow (BM) aspiration and trephine biopsy showed the presence of 17% plasma cells [Figure 2a-c]. Plasma protein electrophoresis revealed a prominent “M band” in the gamma globulin region [Figure 2d]. Unfortunately, the disease had an aggressive course, and the patient subsequently expired before a therapeutic intervention could be attempted.
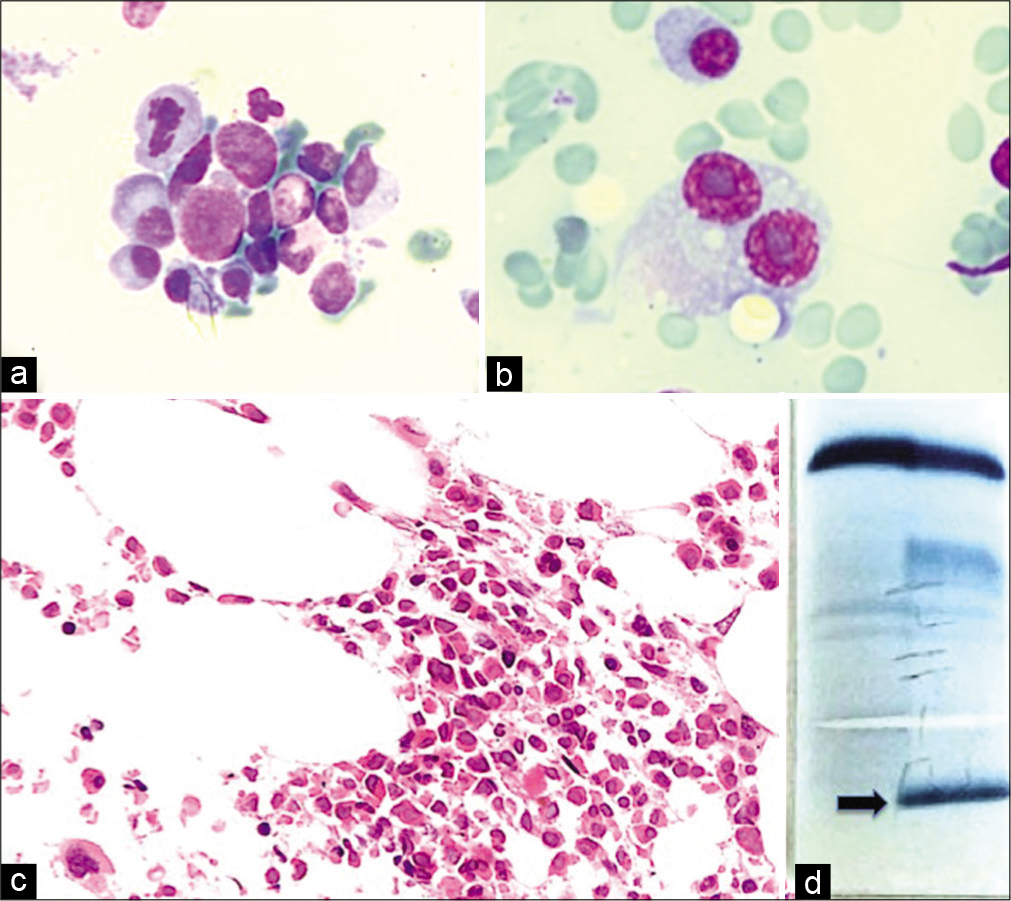
- (a) Bone marrow aspirate smear shows aggregates of plasma cells showing eccentrically placed nucleus and cytoplasmic perinuclear hof (MGG stain, ×400). (b) A giant binucleate myeloma cell showing coarse nuclear chromatin and prominent nucleoli. A mature plasma cell is seen in the background (MGG stain, ×400). (c) Bone marrow biopsy shows increased plasma cells, seen as singly scattered cells (H and E, ×400). (d) Serum electrophoresis shows a prominent M band in the gamma globulin region (arrowhead).
ADDITIONAL QUIZ QUESTIONS
Q1. What is your final diagnosis after cytological and hematological, biochemical, and serological evaluation [Figure 2]?
Solitary bone plasmacytoma
Solitary extramedullary plasmacytoma
Solitary plasmacytoma with minimal marrow involvement
Multiple myeloma
Q2. Which of the following is not considered a myeloma defining event in patients without CRAB features? (Hypercalcemia [C], renal impairment [R], anemia [A], and bone lesions [B])
BM plasma cells ≥60%
Monoclonal globulin spike on serum protein electrophoresis, with an immunoglobulin (Ig) G peak of >3.5 g/dL or an IgA peak of >2 g/dL, or urine protein electrophoresis (in the presence of amyloidosis) result of greater than 1 g/24 h
Abnormal MRI with more than 1 focal lesion, with each lesion being >5 mm in size
Involved/uninvolved serum free light chain ratio ≥100
Q3. Which of the following cytogenetic abnormality is most commonly associated with extramedullary manifestations in multiple myeloma?
del(17p13)
t(4;14)
t(13;14)
t(14;16)
Answers to the additional quiz questions
1 (d); 2 (b); 3 (a)
(d). Solitary plasmacytoma is defined by the presence of a single biopsy-proven lesion (either bony or extramedullary) and a normal BM examination.[1] Extramedullary plasmacytoma (EMP) is a plasma cell neoplasm of soft tissue without BM involvement or other systemic characteristics of multiple myeloma. Patients with solitary plasmacytoma who have limited (<10%) clonal BM plasma cells are considered to have solitary plasmacytoma with minimal marrow involvement.[1] The present case shows 17% plasma cells in the BM. Hence, a diagnosis of multiple myeloma (MM) is appropriate.
-
(b). The International Myeloma Working Group updated the criteria for diagnosis MM to allow, in addition to the classic CRAB features, three “myeloma-defining biomarkers.” The new definition of MM is:[1]
Clonal BM plasma cells >10% or biopsy-proven bony or EMP in addition to any one or more of the CRAB features and myeloma-defining events:
Evidence of end-organ damage that can be attributed to the underlying plasma cell proliferative disorder, specifically
Hypercalcemia: Serum calcium >0.25 mmol/L (>1 mg/dL) higher than the upper limit of normal or >2.75 mmol/L (>11 mg/dL)
Renal insufficiency: Creatinine clearance <40 mL per minute or serum creatinine >177 mol/L (>2 mg/dL)
Anemia: Hemoglobin value of >20 g/L below the lowest limit of normal or a hemoglobin value <100 g/L
Bone lesions: One or more osteolytic lesion on skeletal radiography, CT, or PET/CT. If BW has <10% clonal plasma cells, more than 1 bone lesion is required to distinguish from solitary plasmacytoma with minimal marrow involvement
Any one or more of the three biomarkers of malignancy or myeloma defining events
60% or greater clonal BM plasma cells
Serum involved/uninvolved free light chain ratio of 100 or greater (provided the absolute level of the involved light chain is at least 100 mg/L)
More than 1 focal lesion on MRI that is at least 5 mm or greater in size.[1]
(a). MM with extramedullary involvement appears to be an uncommon phenomenon. Studies have shown extramedullary manifestations in MM to confer higher incidence of poor cytogenetic aberrations and resistance to novel therapeutic agents. These patients are known to show higher incidence of del(17p13) and amp(1q21) and pose potential therapeutic difficulties.[2]
BRIEF REVIEW OF THE TOPIC
MM is one of the most frequently encountered hematological malignancies, occurring as a result of uncontrolled expansion of clonal plasma cells.[1] It is a multifocal neoplasm, with presenting complaints of anemia, infections, hypercalcemia, renal failure, neurological manifestations, punched out lytic lesions of bone, and osteoporosis. However, occasionally, it may present with extramedullary manifestations in the form of tumor masses in the bone, soft tissue, or viscera. EMP has an incidence of 6–8% at the time of diagnosis of MM.[3] The EMP is found most commonly in the head-and-neck region (80%), especially the nasopharynx and paranasal sinuses and to a lesser extent in the gastrointestinal tract, central nervous system, lymph nodes, etc.[4] MM presenting as localized soft-tissue swelling in the scalp, with intracranial extension is rare, with few cases published so far.[4-7]
A pathologically diagnosed plasmacytoma of the soft tissue may be the only presentation of MM in the initial phase or can be a late extramedullary manifestation seen in the aggressive phase of the disease. It can also be a direct extension or metastasis from underlying solitary plasmacytoma of the bone. The case discussed here, probably arose from the plasmacytoma of the underlying calvarium, with the mass causing bony erosion, cortical breach, and extension into the overlying soft tissue of the scalp.
Literature discussing utilizing cytology for the diagnosis of EMP is further limited.[8-10] Depending on the site of the EMP, different types of cytological specimen may be obtained. FNAC is usually the first line of investigation for any palpable swelling such as EMP of soft tissue and lymph nodes. Rarely, lesions may also present in lung and gastrointestinal tract, where a guided FNA from the mass, scrape smears, bronchoscopic, or endoscopy-guided brushings may be useful.[10] The case discussed here illustrated the classical morphology of malignant plasma cells on FNAC smears. The diagnosis is usually straightforward in the presence of numerous mature plasma cells, with limited differentials. Nevertheless, the cells may occasionally show marked anaplasia and pleomorphism, accompanied by giant myeloma cells posing a cytological diagnostic dilemma. The larger cells with a centrally placed nucleus, prominent nucleoli, and sometimes associated with multinucleation may be misinterpreted as Reed-Sternberg cells or as megakaryocytes.[8-10] The plasmablastic morphology may further be confused with atypical lymphoid cells, immunoblasts, and centroblasts seen in high-grade nonHodgkin’s lymphoma. However, the presence of at least few mature plasma and a characteristic lack of lymphoglandular bodies in the background act as diagnostic clues to plasmacytoma. The EMP also needs to be distinguished from other extranodal marginal B-cell lymphomas and MALTomas with plasmacytic differentiation. Furthermore, site-specific differentials may be considered at varied locations. For example, in FNAC from neuroendocrine tumor of the liver, spleen, and pancreas, differentiating tumor cells from plasma cells are a challenge. In breast, plasmacytoma may be mistaken as lobular carcinoma to the unsuspecting eyes. Immunohistochemistry on cell block preparation and flow cytometry of the aspirated fluid provides a valuable adjunct in these scenarios. The diagnosis is further simplified when protein electrophoresis, BM evaluation, and skeletal survey are evaluated.[9]
Differentiating solitary plasmacytoma from a case of MM is of paramount importance, as the therapeutic approach and prognosis differ. The prognosis of plasmacytoma concurrent with newly diagnosed MM is dismal, with a median survival of less than 3 years.[11] It may further indicate failure to respond in cases already on therapy. Studies have shown a satisfactory role of surgical removal of the tumor in combination with post-operative radiotherapy and chemotherapy for systemic involvement.[4,6]
SUMMARY
The present case describes the rare presentation of MM as scalp swellings. FNAC is a simple, first-line investigation for the diagnosis of extramedullary manifestation of MM, which helps in the early diagnosis and management of these patients.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The author(s) declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that they qualify for authorship as defined by ICMJE http://www.icmje.org/#author. Each author has participated sufficiently in the work and take public responsibility for appropriate portions of the content of this article.
GR: Conceptualization, drafting of the manuscript, revising it critically for important intellectual content, literature review.
NA: Writing of the original draft, data acquisition, revising it critically for important intellectual content, literature review.
UH: Critical review, finalization of the manuscript, revising it critically for important intellectual content, cytological workup.
AP: Critical review, finalization of the manuscript, hematological workup and revising it critically for important intellectual content.
Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
As this is a quiz case without identifiers, our institution does not require approval from Institutional Review Board (IRB) (or its equivalent).
LIST OF ABBREVIATIONS (In alphabetic order)
BM: Bone Marrow
CECT: Contrast Enhanced Computed Tomography
CRAB: Hypercalcaemia (C), Renal impairment (R),Anaemia (A), and Bone lesions (B)
EMP: Extramedullary Plasmacytoma
FNAC: Fine needle aspiration cytology
MM: Multiple myeloma
MRI: Magnetic Resonance Imaging
WBC: White Blood Cell.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (the authors are blinded for reviewers and vice versa) through automatic online system.
References
- Updated diagnostic criteria and staging system for multiple myeloma. Am Soc Clin Oncol Educ Book. 2016;35:e418-23.
- [CrossRef] [PubMed] [Google Scholar]
- Extramedullary manifestation in multiple myeloma bears high incidence of poor cytogenetic aberration and novel agents resistance. Biomed Res Int. 2015;2015:787809.
- [CrossRef] [PubMed] [Google Scholar]
- Extraosseous multiple myeloma: Case report of presentation in the lower extremity soft tissues with literature review. Case Rep Radiol. 2017;2017:9159035.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple myeloma with pathologically proven skull plasmacytoma after a mild head injury: Case report. Medicine (Baltimore). 2018;97:e12327.
- [CrossRef] [PubMed] [Google Scholar]
- A case of multiple myeloma presenting as scalp swelling with intracranial extension. J Neurosci Rural Pract. 2013;4:445-8.
- [CrossRef] [PubMed] [Google Scholar]
- POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, multiple myeloma and skin changes) with cranial vault plasmocytoma and the role of surgery in its management: A case report. J Med Case Rep. 2013;7:245.
- [CrossRef] [PubMed] [Google Scholar]
- A hole in the skull: CT manifestations of a solitary plasmacytoma in skull. Quant Imaging Med Surg. 2012;2:61-2.
- [Google Scholar]
- Cytodiagnosis of extramedullary plasmacytomas. Acta Cytol. 2010;54:255-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cytodiagnosis of multiple myeloma presenting as orbital involvement: A case report. Cytojournal. 2006;3:19.
- [CrossRef] [PubMed] [Google Scholar]
- Fine needle aspiration cytology in extramedullary plasmacytoma. Acta Cytol. 2000;44:287-91.
- [CrossRef] [PubMed] [Google Scholar]
- Extramedullary plasmacytoma in the presence of multiple myeloma: Clinical correlates and prognostic relevance. Onco Targets Ther. 2012;5:329-34.
- [CrossRef] [PubMed] [Google Scholar]








