Translate this page into:
Cytomorphological features of papillary cystadenocarcinoma of parotid gland: A case report with review of literature
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Papillary cystadenocarcinoma is a very rare slow growing malignant neoplasm characterized by cysts and intraluminal papillary projections. It is defined by WHO as a separate entity. On FNA, cytological features can mimic with various papillary and cystic neoplasms of salivary gland. It is also difficult to distinguish from benign salivary gland neoplasms as it has bland nuclear features. Thus we present cytomorphological features and discuss its differential diagnosis with neoplasms having prominent papillary architecture with review of literature.
Keywords
Cytology
fine needle aspiration
papillary cystadenocarcinoma
parotid
salivary gland
INTRODUCTION
Papillary cystadenocarcinoma (PCA), also known as mucin-producing adenopapillary carcinoma, is a rare, slow-growing, malignant neoplasm of the salivary glands. Major locations in decreasing order of frequency include minor salivary gland, parotid gland, and submandibular gland.[1] It accounts for 2% of all malignant salivary gland tumors.[2] The cytological features can overlap with various benign and malignant neoplasms having papillary pattern. Most of these neoplasms are cystic in nature. The diagnostic accuracy of these cystic neoplasms is low as compared to other solid neoplasms of the salivary glands. Besides this, sometimes, cystic degeneration can lead to sampling error.[34] Thus, here, we present the diagnostic cytomorphological features of this rare cystic-papillary neoplasm along with differential diagnosis.
CASE REPORT
A 33-year-old female presented with a left parotid swelling which had progressively increased in size in the last 5 months. The clinical examination revealed a well-defined, firm to hard tender swelling, measuring 4 cm × 3 cm, which was fixed to the underlying structure.
Cytology
Fine needle aspiration was done with a 22 G needle. The aspiration yielded 8 ml of hemorrhagic fluid following which the swelling regressed but did not disappear completely. The fluid so obtained was cytocentrifuged and smears were prepared. The second aspiration was performed from the residual swelling. All the smears thus prepared were stained with May-Grunwald-Giemsa, hematoxylin and eosin, and Papanicolaou stain.
Microscopy showed cellular smears which were comprised of neoplastic cells arranged in groups, solid nests, and complex branching papillary fragments. Most of these cells were cuboidal to columnar with eccentrically placed bland appearing nuclei exhibiting mild pleomorphism with minimal mitotic activity. Some of these cells also revealed oncocytic changes. Amidst, these cells were the cyst macrophages. Most of the cells had dense cytoplasm with a fair number of them displaying small vacuolated, soap bubble-like appearance of the cytoplasm [Figure 1]. Occasional univacuolated signet ring cells and mucin vacuoles were also noted. These cells were positive for periodic acid–Schiff with acid digestion (PAS-AD) [Figure 2]. Features were suggestive of low-grade PCA (LGPCA). The patient underwent surgery with wide excision of the uninvolved tissue.
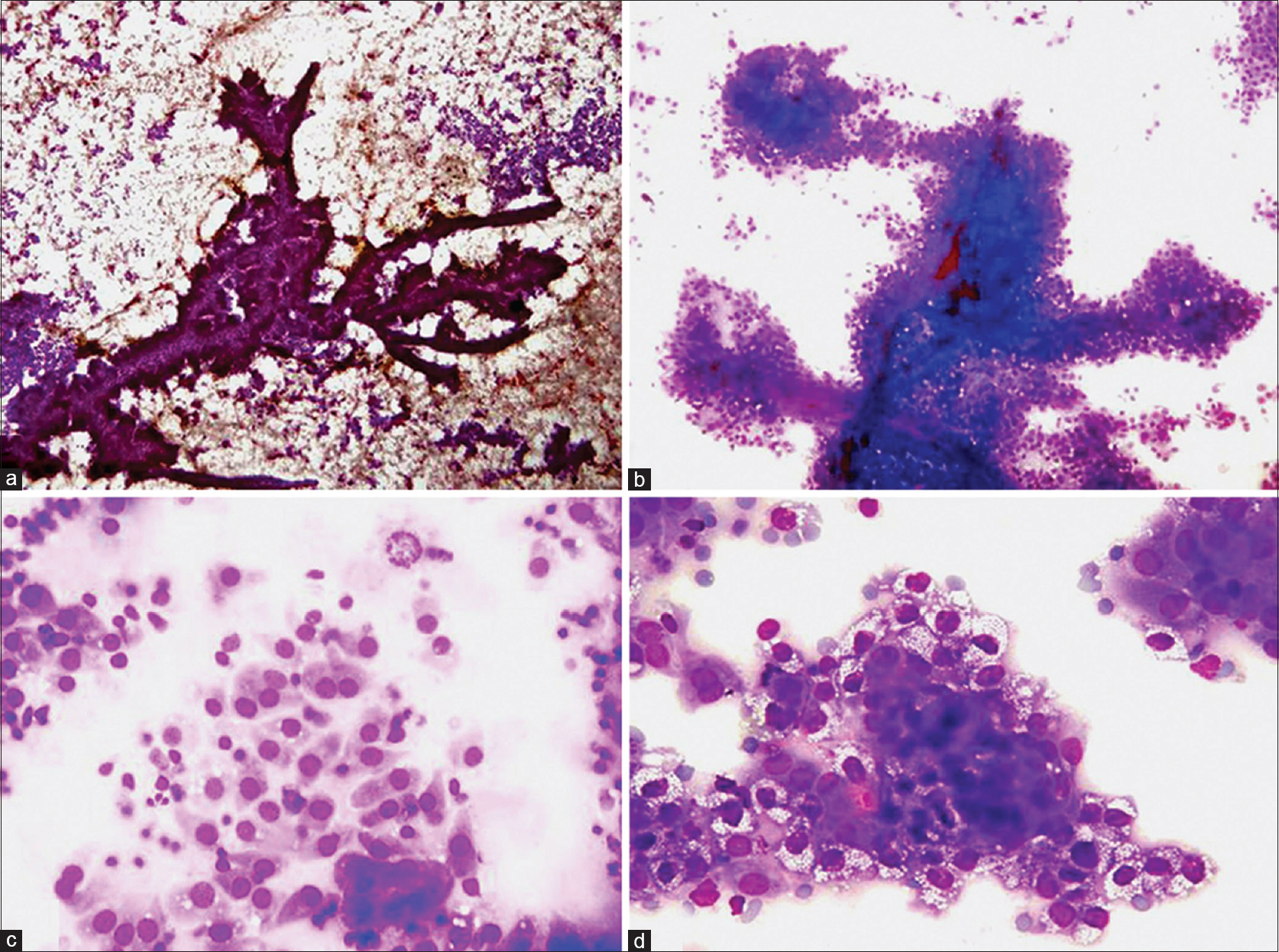
- (a and b) Complex papillary pattern along with singly scattered cells (a: Papanicolaou, ×40). Fibrovascular cores are also visible (b: May-Grunwald-Giemsa, ×100). (c) Dispersed cells displaying cuboidal to columnar cells with eccentrically placed nuclei exhibiting mild pleomorphism. An occasional mitotic figure is also seen at the top of the field (May-Grunwald-Giemsa, ×400). (d) Cells showing vacuolated cytoplasm with soap bubble appearance (May-Grunwald-Giemsa, ×400)
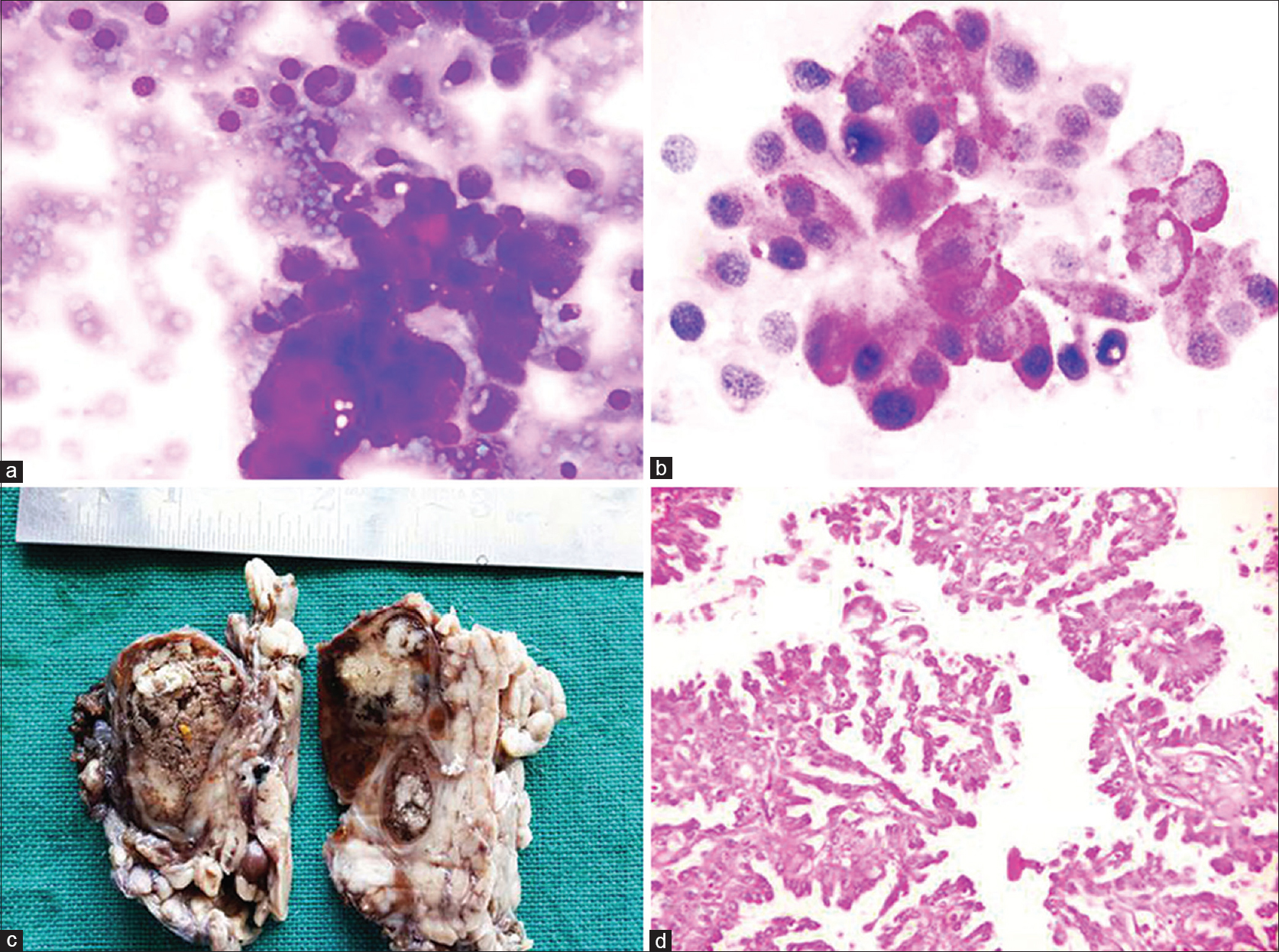
- (a) Some cells show eccentric nuclei with bright eosinophilic mucin vacuole (May-Grunwald-Giemsa, ×400). (b) Vacuolated cells showing periodic acid–Schiff with acid digestion positivity (PAS-AD, ×400). (c) A partially cystic and partially solid mass with friable papillary projections. (d) Sections showing cuboidal to columnar cells with mild cellular atypia displaying pseudostratification (H and E, ×100)
Histopathology
Grossly, a partially cystic and partially solid mass was received measuring 3.5 cm × 3.0 cm × 2.0 cm with many friable papillary projections [Figure 2c].
Microscopy revealed multiple cystic spaces with intraluminal papillary projections, which were lined by cuboidal to columnar cells displaying mild cellular atypia. At places, pseudostratification with mitosis was also seen [Figure 2d]. There was invasion of the underlying muscle.
DISCUSSION
PCA is a rare slow-growing malignant neoplasm characterized by cysts and intraluminal papillary projections. It is conceptually the malignant counterpart of benign cystadenoma and the histological diagnosis rests on actual infiltration of surrounding parenchyma and underlying connective tissue.[1] There are a few reports describing its cytological features.
The cytological findings observed were in accordance with Mardi et al.,[1] Kawahara et al.,[2] Kapila and Verma,[5] and Aloudah et al.[6] A prominent papillary architecture, single cells, sheets of cells in varying proportion along with individual cuboidal to columnar cells having eccentrically placed bland appearing nuclei were the common findings. There was presence of an occasional mitotic figure, but anaplasia was absent [Figure 1a-c].
Soap bubble appearance of the cytoplasm seen in this case study was similar to the findings of Kawahara et al.[2] Kapila and Verma[5] also observed this feature in one out of four cases of PCA [Figure 1d].
Mucin-secreting goblet cells were noted by Mardi et al.[1] and Kapila and Verma.[5] These cells were also present focally in this case study [Figure 2].
Papillary pattern is not an uncommon finding in aspirates from cystic as well as noncystic salivary gland swellings. The cystic neoplasms include papillary cystadenoma, Warthin tumor (WT), PCA, acinic cell carcinoma papillary cystic variant (ACC-PCV), and rarely in low-grade mucoepidermoid carcinoma (LGMEC). The noncystic neoplasms displaying papillary pattern are inverted ductal papilloma and intraductal papillomas (IDPs), sialadenoma papilliferum (SP), polymorphous low-grade adenocarcinoma (PLGA), salivary duct carcinoma (SDC), oncocytoma, and epithelial and myoepithelial carcinoma (EMC).[7]
Differential diagnosis
As benign appearing cells are seen in PCA, benign neoplasms having prominent papillary architecture are included in the differential diagnosis. Large, complex, and branching papillary structures as compared to small and simple papillary groups along with occasional mitosis can be a helpful feature in differentiating this malignant neoplasm from benign neoplasms.
IDPs and SP affect minor salivary gland. They have simple papillary architecture with bland nuclear features. In addition, inverted ductal papillomas have squamous and basaloid appearing epithelium.[7]
Papillary cystadenoma has almost similar features to LGPCA, but the papillary architecture is somewhat simple rather than complex and there is lack of mitosis.[78] However, its differentiation from PCA is almost impossible based on cytomorphology alone.
Smears from WT show monolayered sheets of oncocytic cells, many lymphocytes in the background of amorphous granular debris, and rarely squamous metaplastic cells.[789]
ACC-PCV is the closest differential diagnosis of PCA after papillary cystadenoma as they have overlapping features. The specimens are cellular, arranged in tightly cohesive fragments as well as monolayered sheets, often with a prominent papillary architecture. The polymorphous population of the cells includes granular cells, vacuolated cells, nondescript small cuboidal cells, and ductal type epithelium displaying high nuclear, cytoplasmic ratio along with the presence of squamoid and metaplastic oncocytic epithelium, which can help in differentiating this entity from PCA.[410] Although tumor cells with small vacuoles having soap bubble-like appearance of cytoplasm, they are common findings of both PCA and ACC-PCV.[2] Special stains for mucin are negative in ACC-PCV.[1]
PLGA, a common salivary gland neoplasm of oral cavity, palate, and upper lips, occurs mostly in older females. Cytological smears can have a prominent papillary architecture, but the papillae are composed of both epithelial and connective tissue components. Its differentiation from PCA is based on the presence of eosinophilic magenta-colored stromal red cores that branches with the associated epithelial papillary structures.[8] Stromal fragments may also be seen in the form of hyaline globules.[1] Hyaline globules were absent in both the epithelial sheets and cores of the papillae in PCA.
SDC occurs predominantly in the parotid. Smears show tubules, glands with occasional presence of the papillary architecture. The individual cells display features of overt malignancy including nuclear enlargement, high nuclear, cytoplasmic ratio, and prominent nucleoli as compared to the bland nuclear morphology in PCA. The background contains some necrosis, apoptotic bodies, and macrophages.[7]
Smears from LGMEC rarely have papillary architecture, but the presence of all the three cellular components comprising of mucous cells, intermediate cells, and squamous cells is the most helpful feature in differentiating it from PCA.[78]
EMC is another salivary gland neoplasm rarely associated with a papillary architecture. A combination of three dimensional well-defined cell clusters surrounded by homogenous acellular material, clear cytoplasm in peripheral cells, and fragments of acellular nonfibrillar material are sufficient to confirm EMC.[11]
Thus, we suggest diagnostic cytomorphological features of this great imitator of salivary gland neoplasms having papillary architecture:
-
Aspiration of cyst fluid
-
A complex branching papillary pattern, single cells, and sheets of cells
-
The cells lining the papillary structures are cuboidal to columnar with basally located nuclei
-
Cells with dense to finely vacuolated cytoplasm (soap bubble appearance)
-
Individual dispersed cells with eccentrically placed nuclei
-
Nuclei are bland appearing with low nuclear cytoplasmic ratio
-
Minimal anaplasia and occasional mitosis
-
Mucin vacuoles positive for mucin stain
-
Hyaline globules are absent
-
Proteinaceous to mucoid background with cystic macrophages.
CONCLUSION
This case report conducts cytomorphological analysis of a rare entity called PCA which practicing cytopathologists should be aware of while reporting the salivary gland aspirates. A careful look at the architecture and individual cytomorphology can identify PCA and rule out various benign and malignant papillary neoplasms of the parotid gland. In addition, cytopathologists can alert the clinician regarding the possibility of PCA rather than a benign neoplasm so that decision can be made preoperatively for its proper clinical management.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All the authors of this article declare that we qualify for authorship as defined by ICMJE UJ contributed to conception, design, defining intellectual content, preparation of manuscript, editing and review of manuscript. SSC contributed to conception, design, literature search, preparation, editing and review of manuscript. NT contributed to conception, design, editing and review of manuscript. HK contributed to conception design, helped in preparation of manuscript, literature search, editing and review of manuscript.
ETHICS STATEMENT BY ALL AUTHORS
As this is a case report without identifiers, approval from Institutional Review Board (IRB) was not required.
LIST OF ABBREVIATIONS (In alphabetic order)
ACC-PCV - Acinic Cell Carcinoma Papillary Cystic Variant
EMC - Myoepithelial Carcinoma
IDPs - Intraductal Papillomas
IRB - Institutional Review Board
LGMEC - Low-Grade Mucoepidermoid Carcinoma
LGPCA - Low-grade PCA
PAS-AD - Periodic Acid–Schiff with Acid Digestion
PCA - Papillary Cystadenocarcinoma
PLGA - Polymorphous Low-Grade Adenocarcinoma
SDC - Salivary Duct Carcinoma
SP - Sialadenoma Papilliferum
WT - Warthin Tumor.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Papillary cystadenocarcinoma of submandibular salivary gland: A rare case report. J Cancer Res Ther. 2010;6:330-2.
- [Google Scholar]
- Cytological features of cystadenocarcinoma in cyst fluid of the parotid gland: Diagnostic pitfalls and literature review. Diagn Cytopathol. 2010;38:377-81.
- [Google Scholar]
- Fine needle aspiration cytology in diagnosis of salivary gland lesions: A study with histologic comparison. Cytojournal. 2013;10:5.
- [Google Scholar]
- Acinic cell carcinoma-papillary cystic variant. Pitfalls of fine needle aspiration diagnosis: Study of five cases and review of literature. Cytopathology. 2009;20:96-102.
- [Google Scholar]
- Cytomorphologic features of papillary cystadenocarcinoma of parotid gland. Diagn Cytopathol. 2002;26:392-7.
- [Google Scholar]
- Low-grade papillary cystadenocarcinoma of the parotid gland: Presentation of a case with cytological, histopathological, and immunohistochemical features and pertinent literature review. Diagn Cytopathol. 2009;37:128-31.
- [Google Scholar]
- Salivary Gland Cytology: A Color Atlas. (1st ed). New Jersey: Wiley Blackwell; 2011. p. :69-240.
- [Google Scholar]
- Salivary gland. In: Cytology Diagnostic Principles and Clinical Correlate (4th ed). Philadelphia: Elsevier Saunders; 2014. p. :301-32.
- [Google Scholar]
- Cystic lesions of the salivary glands: Cytologic features in fine-needle aspiration biopsies. Diagn Cytopathol. 2002;27:197-204.
- [Google Scholar]
- Acinic-cell carcinoma, papillary-cystic variant: A diagnostic dilemma in salivary gland aspiration. Diagn Cytopathol. 2002;27:244-50.
- [Google Scholar]
- Epithelial-myoepithelial carcinoma of the salivary gland. Fine needle aspiration cytologic findings. Acta Cytol. 1990;34:243-7.
- [Google Scholar]








