Translate this page into:
Fine needle aspiration cytology finding of a parotid mass with chondromyxoid matrix and variable epithelial cytological atypia
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 52-year-old male patient was admitted with a left parotid mass (2.4 cm) [Figure 1a], first noticed a year ago. The patient reported that it was painless and slowly growing. A fine needle aspiration biopsy was performed [Figures 1b–e].
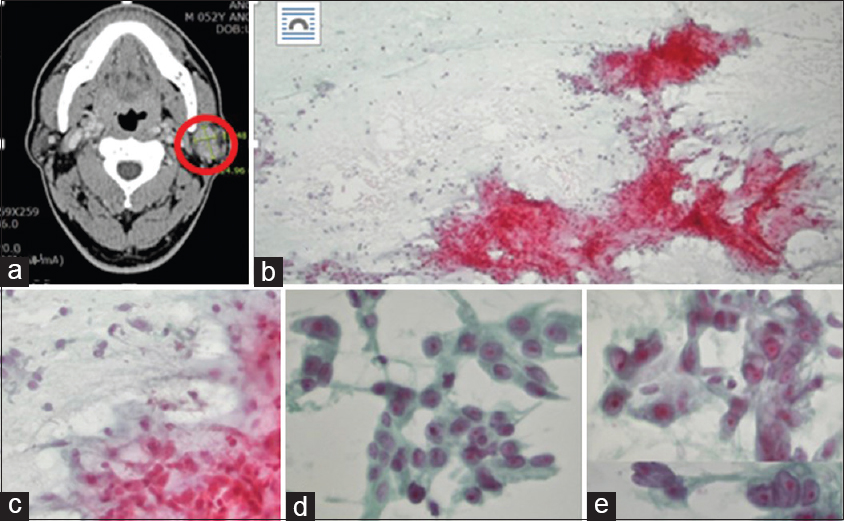
- (a) A neck computed tomography showing a bilobular heterogeneous mass (red circle) in the left parotid gland with progressive enhancement, most probably a pleomorphic adenoma. (b) Aspiration cytology showing moderate cellularity with chondromyxoid matrix (Pap, ×100). (c) The periphery of the myxoid stroma includes attached bland-looking ovoid epithelial cells (Pap, ×200). (d) Some clusters of the epithelial cells containing more plump epithelial cells with abundant oncocytic cytoplasm (Pap, ×400). (e) Other clusters of the epithelial cells exhibiting more severe cytologic atypia; a higher nuclear-/cytoplasmic ratio, hyperchromatic nuclei, irregular nuclear membrane, prominent nucleoli, and abundant vacuolated cytoplasm (Pap, ×400)
WHAT IS YOUR INTERPRETATION?
-
Benign pleomorphic adenoma (PA)
-
Malignant neoplasm
-
PA, but cannot excluded malignant potential, such as CXPA
-
Carcinoma ex pleomorphic adenoma (CXPA).
ANSWER
The correct cytologic interpretation is C:
C. PA, but cannot exclude malignant potential, such as CXPA
BRIEF FOLLOW-UP
The patient underwent a superficial parotidectomy and is alive and well without additional treatment.
ADDITIONAL QUIZ QUESTIONS
Q1. Considering the patient's age, sex, location of the tumor, and radiologic findings, what is the most relevant cytodiagnosis?
-
Benign mixed tumor (PA)
-
Malignant salivary gland tumor
-
Most likely pleomorphic adenoma, but not exclusion of CEPA
-
Widely invasive CXPA.
Q2. What is the most important tip for cytological diagnosis?
-
Recognition of chondromyxoid matrix
-
Recognition of cytologic atypia
-
Oncocytic epithelial cytomorphology
-
Recognition of two different components.
Q3. Considering the histologic findings, what is the final diagnosis of this lesion?
-
Intratubular (intraductal) CXPA
-
Extratubular CXPA
-
Intracapsular CXPA
-
Extracapsular CXPA.
Q4. What are the useful markers for the adenoma-carcinoma sequence in CEPA?
-
PLAG1, HMGA2
-
P53, Ki-67
-
ER, PR
-
HER2, ER
ANSWERS TO ADDITIONAL QUIZ QUESTIONS
A1; C, A2; D, A3; A, A4; B
A1. PA is the most common salivary gland tumor in both children and adults, accounting for the majority of all salivary gland neoplasms. Some cytologic findings in this case (chondromyxoid matrix, bland-looking epithelial cells around the myxoid stroma) are compatible with PA. However, other worrisome cytologic features are reminiscent of carcinomatous transformation (CXPA). A diagnosis of malignant salivary tumor or widely invasive CEPA should not be made due to a possibility of overtreatment
A2. The most important tip for cytologic diagnosis is the recognition of two different components: bland looking epithelial cells and clusters of atypical cytology [Figures 2a–c].
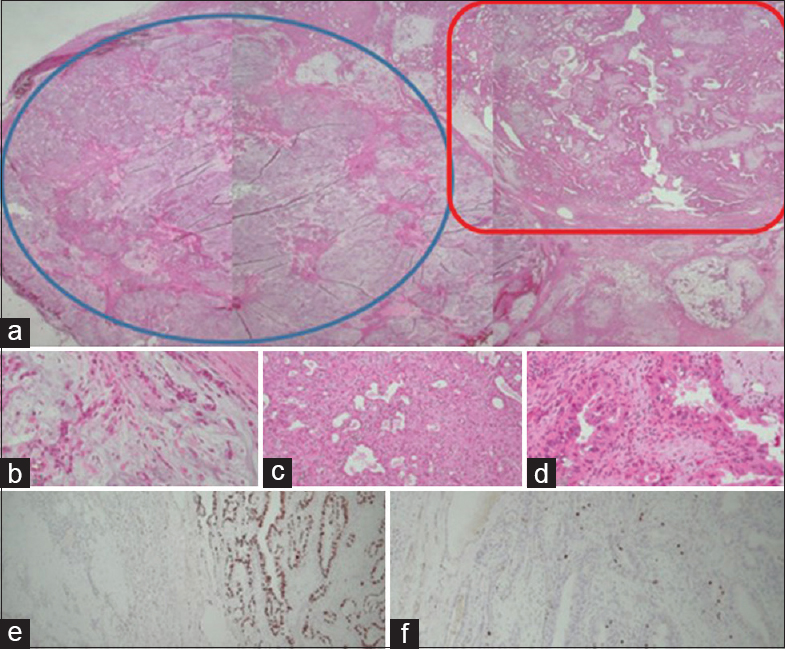
- (a) The histology of the tumor showing two different nodules; myxoid hypocellular in one (blue circle) and another cellular mass with scanty myxoid stroma (red rectangle) (H and E, ×10). (b) This section showing a part of the chondromyxoid stroma and attenuated epithelial component (H and E, ×40). (c) This portion showing cellular proliferation composed of abundant eosinophilic epithelial cells with oncocytic changes (H and E, ×40). (d) The epithelial cells reveal distinct cytologic atypia with enlarged hyperchromatic nuclei and moderate pleomorphism (H and E, ×40). (e) p53 immunohistochemical staining showing different expressions between the two parts: very low expression in the chondromyxoid nodule and high expression in the atypical portion (p53, ×40). (f). The Ki-67 proliferation index is also significantly higher in the atypical portion (Ki-67, ×40)
A3. Considering the histologic findings, the final diagnosis of this lesion is PA with atypical features or early CXPA (intratubular/intraductal) type. The most atypical epithelial cells are confined to tubules or ducts [Figure 2d]
A4. The useful markers for adenoma-carcinoma sequence in CXPA are P53, Ki-67, and Her-2neu. PLAG1 and HMGA2 are transcription factors in both PA and CXPA [Figures 2e–f].
BRIEF REVIEW OF THE TOPIC
CXPA is a broad category of cancers of the salivary glands, including at least two clinically relevant categories: early CXPA (ECXPA) and widely invasive CXPA.[1] In the 2017 World Health Oraganization (WHO)'s classification, early CXPA was more subdivided.[2] ECXPA included non-invasive (in situ, intraductal, or intratubular) and early invasive (extratubular, intracapsular, or extracapsular; <6 mm) and it showed an excellent prognosis, very different from widely invasive CXPA. Therefore, we should try to differentiate cases of ECXPA among benign PA.[34]
Although treatments for both PA and CXPA are complete excision, the extent of resection and the necessary safety margin are different. Therefore, cytological detection on aspiration samples can be an important key to management.
The cytological findings of CXPA have been reported in only a few case reports. The incidence of mild atypia in PA causing diagnostic problems has been reported to be as high as 50%.[5] The authors think that even moderate atypia should be tolerated and that malignancy should be suspected only in the presence of numerous atypical cells and the absence of chondromyxoid stroma. Many cytological variations have been reported, which are not correlated with tumor behavior and prognosis.[4]
The cytomorphologic spectrum of CXPA has been studied.[678] Nigam et al. analyzed aspiration cytological findings of 14 CXPA cases. The significant features were a loose; cohesive cluster; adenoid and papillary patterns; and dissociated cells. The tumor cells showed moderate to marked pleomorphic; and prominent nucleoli.
Very ECXPAs or composite tumors of benign and malignant nodules as this quiz case show distinct benign PA findings and focal moderate epithelial atypia, which can be misdiagnosed as benign PA.
In conclusion, a cytological diagnosis of CXPA can be possible if both components are properly recognized and unequivocal malignant cells in the background of biphasic components of PA. An erroneous diagnosis is possible due to misinterpretation, lack of experience, and sampling errors, compounded by the clinical overlap of the conditions.
SUMMARY
-
Although rare, CXPA can occur among pleomorphic adenomas
-
In cases with a strong clinical suspicion, multiple fine needle aspirations should be attempted
-
In hypercellular smears with predominant epithelial components and any degree of atypia, a suspicion of CXPA should be raised.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
HK designed this quiz case.
ETHICS STATEMENT BY ALL AUTHORS
As this is a quiz case without patient identifiers, our institution does not require approval from the institutional Review Board.
LIST OF ABBREVIATIONS (In alphabetic order)
CXPA - Carcinoma ex pleomorphic adenoma.
PA - Pleomorphic adenoma.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Carcinoma ex pleomorphic adenoma, with particular emphasis on early lesions. Head and Neck Pathol. 2013;7(Suppl 1):S68-76.
- [Google Scholar]
- Carcinoma ex pleomorphia adenoma. In: El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ, eds. WHO Classification of Head and Neck Tumors. Lyon: IARC Press; 2017. p. :p176-7.
- [Google Scholar]
- HER-2/neu gene amplification in carcinoma ex pleomorphic adenoma in relation to progression and prognosis: A chromogenic in- situ hybridization study. Histopathol. 2012;60:E131-42.
- [Google Scholar]
- Intracapsular (in situ) carcinoma ex pleomorphic adenoma with unusual clinical and histological features. Eur Arch Otorhinolaryngol. 2008;265:1563-6.
- [Google Scholar]
- Minimally invasive carcinosarcoma ex pleomorphic adenoma: A case report and literature review with cytohistological correlation. Head Neck. 2016;38:E2483-9.
- [Google Scholar]
- Fine needle sampling of salivary gland lesion: I. Cytology and histology correlation of 412 cases of pleomorphic adenoma. Diagn Cytopathol. 1996;14:195-200.
- [Google Scholar]
- Pleomorphic adenoma: Cytologic variation and potential diagnostic pitfalls. Diagn Cytopathol. 2009;37:11-5.
- [Google Scholar]
- Cytomorphologic spectrum of carcinoma ex pleomorphic adenoma. Acta Cytol. 2004;48:309-14.
- [Google Scholar]







