Translate this page into:
Fine-needle aspiration cytology of pilomatrixoma: A short series of three cases
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pilomatrixoma (PMX) (pilomatricoma, calcifying epithelioma of Malherbe) is a benign tumor with differentiation toward the hair matrix cells and is common in head and neck region. It is most commonly seen in the first two decades of life and presents as a subcutaneous, small, asymptomatic firm solitary nodule. Fine-needle aspiration cytology (FNAC) has been described as an important preoperative diagnostic investigation though on cytology the diagnosis of PMX is sometimes difficult and misdiagnosed. We describe two patients with gradually increasing asymptomatic swelling on pinna and middle finger. FNAC was done and a diagnosis of PMX was given, further confirmed by histopathological examination. The present cases highlight the importance of FNAC in considering PMX as differential diagnosis of dermal or subcutaneous nodules in locations other than head and neck. Cytopathologists who play an important role in the preliminary diagnosis should keep in mind the variability of the cellular composition of these types of lesions to avoid misdiagnosis.
Keywords
Adnexal tumor
fine-needle aspiration cytology
hair
pilomatrixoma
skin
INTRODUCTION
Pilomatrixoma (PMX) (pilomatricoma, calcifying epithelioma of Malherbe) is a benign tumor with differentiation toward the hair matrix cells, common in head and neck region, accounts 20% of pilar tumors and commonly seen in the first two decades of life.[1] PMX usually presents as subcutaneous, small, asymptomatic, firm, solitary, nodule, with overlying skin showing bluish discoloration at times.[2] Few patients may experience pain on palpation, discomfort, itching, and episodes of infection, discharge, or even ulceration.[2] The histological features are well recognized and characteristic but now a day's fine-needle aspiration cytology (FNAC) has been described as an important preoperative diagnostic investigation. On cytology diagnosis of PMX is sometimes difficult and misdiagnosed.[3] Many authors’ described the FNA findings of PMX but still difficult and misdiagnosed especially by young pathologist.[4] We described FNA findings of a case of PMX with review of the literature.
CASE REPORTS
Case 1
A 19-year-old female presented to FNAC clinic with a history of gradually increasing swelling on right pinna for the last 2-3 years [Figure 1a]. There was no associated pain or history of trauma prior to the appearance of the swelling. Local examination showed a firm to hard, freely mobile subcutaneous swelling measuring 1.5 cm × 1.5 cm in size. The overlying skin showed slight reddish discoloration.
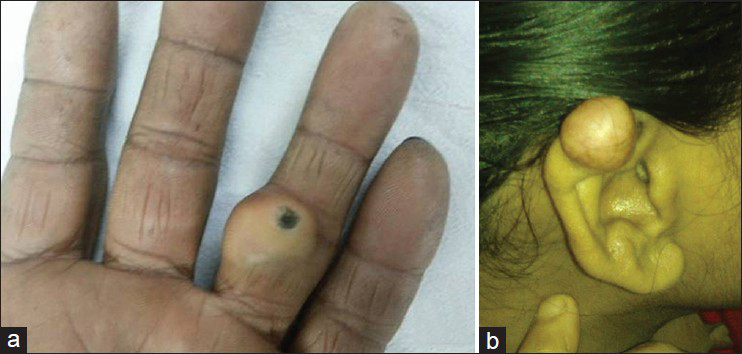
- (a) Case 1 with a firm swelling on the middle finger of right hand measuring 2.0 cm × 2.0 cm. The overlying skin showed no discoloration except a black self-needling mark. (b) Case 2 with a subcutaneous swelling on right pinna measuring 1.5 cm × 1.5 cm with slight reddish discoloration
Case 2
A 16-year-old male presented with a gradually increasing swelling on the middle finger of the right hand with associated pain since 3 years [Figure 1b]. There was no history of trauma, and local examination showed a firm, freely mobile subcutaneous swelling measuring 2.0 cm × 2.0 cm in size. The overlying skin was normal.
Case 3
A 9-year-old male presented with a swelling on right side neck of 2 years duration. There was no associated pain or history of trauma prior to appearance of the swelling. On examination, it was a firm, freely mobile swelling in the posterior triangle of the neck measuring 1 cm × 1 cm. The overlying skin was normal. Clinical figure is not available. Clinically inclusion cyst was the diagnosis in case 1 and case 2 and in case 3 clinical suspicion of an enlarged lymph node was considered. FNAC was performed using 23G needle and 10 mL syringe. Wet fixed and air dried smears were stained with H and E and Giemsa respectively. FNAC was done followed by surgical resection in all the three cases for histological confirmation of diagnosis.
Microscopy of case 1 and case 2 show moderately cellular smears comprising of sheets of degenerated anucleated and keratinized squamous cells (ghost cells). Few cluster of basaloid cells having large, round, regular basophilic nuclei with evenly dispersed chromatin and large nucleoli with ill-defined cytoplasmic margins and sheets of anucleated squames along with focal areas of calcified debris. Case 1 showed few scattered giant cells in addition to the above mentioned findings and case 2 in addition showed a solitary cluster comprising of small squamous cells with small, dark nuclei and scant dense cytoplasm surrounded by basaloid cells [Figures 2 and 3a].
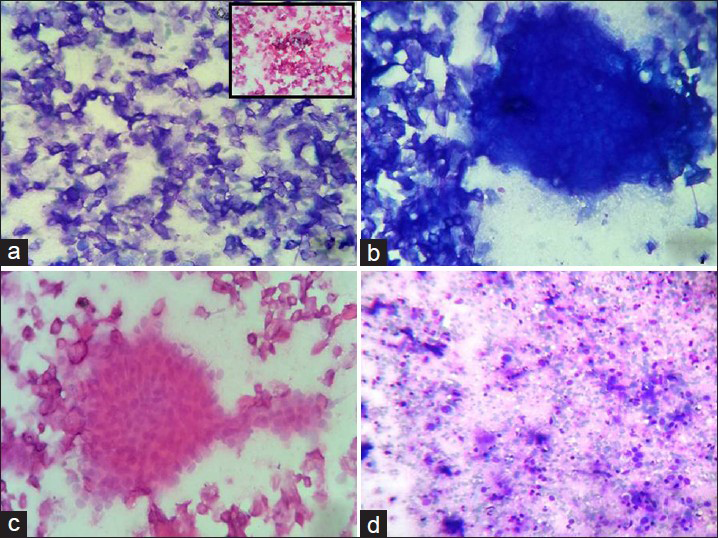
- (a) Sheets of anucleated squames (Giemsa, ×400) with foci of calcification (inset H and E, ×400). (b) Island of ghost cells along with anucleated squames (Giemsa, ×400). (c) Cluster of basaloid cells with round to oval nuclei with ill-defined cytoplasm (H and E, ×400). (d) Few anucleated squames with background comprising of inflammatory infiltrate (mainly lymphocytes) few foam cells, few naked nuclei and cellular debris (Giemsa, ×400)
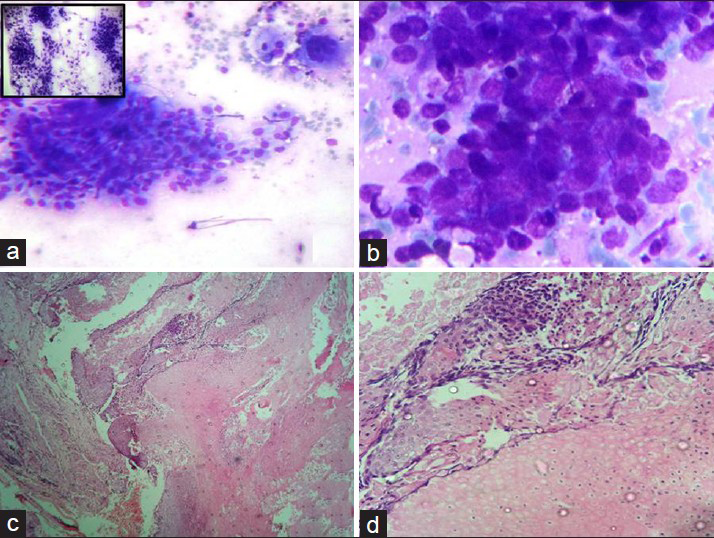
- (a and b) Cluster of basaloid cells having eccentric round to oval vesicular nuclei with mild to moderate amounts of ill-defined cytoplasm. Cells within the cluster show mild pleomorphism and overlapping. A giant cell, few foam cells, naked nuclei and scant inflammatory infiltrate is also seen and three dimensional clusters of basaloid cells (inset) (Giemsa, ×100, ×400). (c and d) Histopathology section showing basaloid cells, anucleate squamous cells and ghost cells (H and E, ×100, ×400)
Case 3 on FNA showed highly cellular smears comprising mainly of singly lying and clusters of small and medium sized basaloid cells showing mild pleomorphism with round to ovoid vesicular nuclei, dispersed nuclear chromatin, occasional nucleoli and mild to moderate cytoplasm with well-defined cell borders. Cells within the clusters at places showed overlapping and nuclear molding. Background showed few naked nuclei, cellular debris and mixed inflammatory infiltrate along with the occasional mitosis [Figure 3b]. A cytologic diagnosis of PMX was rendered in case 1 and case 2 and biopsy advised. However, case 3 was earlier categorized as squamous cell carcinoma/appendageal tumor on the basis of predominance of basaloid cells showing pleomorphism and occasional nucleoli. But considering the patients young age, duration of the swelling and lack of significant pleomorphism made us do a careful reexamination of smears which eventually showed an occasional ghost cells and a diagnosis of PMX cannot be rule out was given on review.
Histopathological examination in all three cases showed typical picture of PMX showing mainly nests of basaloid cells, few islands of ghost cells along with foreign body giant cells and focal areas of calcification. Giant cells were absent in case 1 and calcification was absent in case 3 [Figure 3c and d].
DISCUSSION
Malherbe and Chenantais coined the term calcifying epithelioma of Malherbe describing its origin as sebaceous glands, however in 1961 Forbis, and Helwig gave the term PMX describing its cell of origin and Arnold coined the term pilomatricoma.[56] PMX is a benign cutaneous adnexal tumor having differentiation toward the hair follicle matrix with a predilection for head and neck region of children and young adults and as it is under recognized on cytology, FNAC of PMX usually results in the over diagnosis of malignancy.[3] Julian and Bowers retrospectively analyzed 209 cases of PMX and observed that the age of presentation of PMX shows a bimodal pattern with the first peak in first decade and the second in sixth decade of life with a female preponderance.[7] Head-neck region being the most common affected region followed by upper limbs, chest and the lower extremities.[28] The neck is most commonly affected followed by the cheek, scalp, preauricular and periorbital areas in the head and neck region and pinna involved only in 4.5% cases.[8] In case 1, the patient had a 1.5 cm × 1.5 cm swelling on right pinna. The cytological characteristics of PMX is the presence of basaloid cells, calcium deposits, naked nuclei, shadow (“ghost”) cells, giant cells and inflammatory background however in about 40% cases characteristic cytological findings of PMX are absent and the rate of correct identification of PMX by FNA is 44%.[2] The basaloid cells are large, round, regular with basophilic nuclei, evenly dispersed chromatin and large nucleoli with ill-defined cytoplasmic margins. Nuclear over lapping and molding is noted in few cases, and the occasional mitosis is present.[9] Small squamous cells with small, dark nuclei and scant dense cytoplasm are present, usually in the center of basaloid cell clusters.[9] Multinucleated giant cells were associated closely with the basaloid cell clusters as well as squames and keratin fragments.[9] A characteristic finding is the presence of fibrillary pink material enveloping basaloid cells singly and in clusters and no background necrosis is seen.[9] In the present cases (1 and 2), FNA smears showed mainly sheets of ghost cells, few clusters of basaloid cells, sheets of anucleated squames and ghost cells along with focal areas of calcification however lacking the characteristic fibrillary pink material. Case 3 showed basaloid cells predominantly with occasional ghost cells in an inflammatory background. Based on FNA smears, differential diagnosis include basal cell carcinoma, squamous cell carcinoma, small cell carcinoma and skin appendage tumor where the smears are predominantly composed of basaloid cells and when ghost cells or foreign body giant cells predominate, the cytologic differential diagnosis include epidermal inclusion cysts or giant cell lesions.[910] Though the lesion in our case (1 and 2) was clinically diagnosed as an inclusion cyst, microscopically diagnosis of PMX was given. However, case 3 was initially diagnosed as squamous cell carcinoma/appendageal tumor as the lesion showed predominant population of compact clusters of basaloid cells showing pleomorphism and occasional nucleoli. However considering the patients young age, duration of the swelling and lack of significant pleomorphism made us do a careful reexamination of smears which eventually showed an occasional ghost cells and a specific diagnosis of PMX was given on review. However, due to the presence of sheets of ghost cells a probable diagnosis of PMX was given which was confirmed on biopsy.
SUMMARY
The present cases highlight the importance of FNAC in considering PMX as a differential diagnosis of dermal or subcutaneous nodules in locations other than head and neck (in our cases it presented as finger and pinna swelling). Furthermore, FNA smears from a swelling located in head and neck region (comparable to our case with right posterior triangle neck swelling). In a young adult should be examined carefully to exclude PMX, as these swellings many a times are mistakenly diagnosed as primary/metastatic malignancies leading to unnecessary radiation/surgery in young adult. Sheets of degenerated anucleated and keratinized squamous cells (ghost cells), cluster of basaloid cells, mild nuclear pleomorphism, dispersed nuclear chromatin, occasional large nucleoli, mild to moderate cytoplasm with ill-defined to well defined cytoplasmic margins, calcified debris, scattered giant cells, nuclear overlapping, and nuclear molding in the clusters are potential pitfalls leading to the misinterpretation of malignancy.
Cytopathologists who play an important role in the preliminary diagnosis should keep in mind the variability of the cellular composition of these types of lesions to avoid misdiagnosis. Further to add that all diagnostic features of PMX are not present in every case.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
On behalf of all the contributors I (Jitendra Singh Nigam) will act and guarantor and will correspond with the journal from this point onward. On behalf of all the contributors I declare that we have no financial or non-financial competing interests, no prior publication, and no conflicts of interest
AUTHORSHIP STATEMENT BY ALL AUTHORS
Both authors of this article declare that we qualify for authorship as defined by ICMJE. Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article. Both J. S. Nigam and S. Singh were each directly involved in the diagnosis of these cases. Both authors read and approved the final manuscript. Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
As in this article case reports were without identifiers, our institution does not require approval from ethical committee of Institute.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model.(authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Limits of fine-needle aspiration cytology in diagnosing pilomatrixoma: A series of 25 cases with clinico-pathologic correlations. Indian J Dermatol. 2012;57:152-5.
- [Google Scholar]
- Diagnostic pitfalls of pilomatricoma on fine needle aspiration cytology. Iran J Dermatol. 2012;15:59-61.
- [Google Scholar]
- Pilomatrixoma: Fine-needle aspiration cytology a report of three cases. Ann Saudi Med. 1997;17:88-91.
- [Google Scholar]
- Multiple pilomatrixomas: Case report and literature review. Ear Nose Throat J. 2008;87:230-3.
- [Google Scholar]
- Pilomatricoma of the head and neck: A retrospective review of 179 cases. Arch Otolaryngol Head Neck Surg. 2003;129:1327-30.
- [Google Scholar]
- A case of pilomatrixoma misdiagnosed as metastatic carcinoma on fine needle aspiration cytology. J Cytol. 2007;24:207-8.
- [Google Scholar]








