Translate this page into:
Molecular classification of endometrial cancer: Impact on adjuvant treatment planning

*Corresponding author: Dimitrios Zouzoulas, 1st Department of Obstetrics and Gynecology, Aristotle University of Thessaloniki, “Papageorgiou” Hospital, Thessaloniki, Greece. dzouzoulas@hotmail.gr
-
Received: ,
Accepted: ,
How to cite this article: Zouzoulas D, Tsolakidis D, Sofianou I, Tzitzis P, Pervana S, Topalidou M, et al. Molecular classification of endometrial cancer: Impact on adjuvant treatment planning. CytoJournal. 2024;21:47. doi: 10.25259/Cytojournal_37_2024
Abstract
Objective:
The traditional histopathological analysis of endometrial cancer (EC) is the main risk group classification tool (low, intermediate, high-intermediate, and high) for the implementation of adjuvant treatment. The International Federation of Gynecology and Obstetrics staging system of EC has incorporated a new molecular classification that serves as a new triage tool for optimal treatment planning for these patients. Our study aimed to investigate the prognostic role of the new molecular classification in EC.
Material and Methods:
A prospective study was conducted in the 1st Department of Obstetrics and Gynecology from January 1, 2022, to March 30, 2024, and included all new EC cases that presented the multidisciplinary tumor (MDT) board after surgery. We considered the traditional pathologic analysis and new molecular classification after performing tests on microsatellite instability (MSI), DNA polymerase epsilon (POLE) mutation, and p53 immunohistochemistry testing.
Results:
The study included 65 patients with presumed early endometrial. All patients underwent surgery and subsequent molecular testing. Among the patients, 35 (54%) had a “positive” result in all of the three markers of molecular classification: 14 patients presented with MSI-H, 5 with POLE gene mutation, and 17 with p53 abnormal expression. One case of multiple classifiers was presented. After the integration of molecular classification, a change was observed in the final MDT board decision in 23 cases (35.4%), including six cases of overtreatment and 17 cases of undertreatment, with statistical significance (P = 0.03469).
Conclusion:
The data suggest that the new molecular classification, that is, testing for POLE mutation, MSI, and p53 mutation and for endometrial carcinoma, is a valuable tool for the recurrence risk prognosis and improved planning of adjuvant treatment for EC.
Keywords
Endometrial neoplasms
Molecular diagnostic techniques
Chemoradiotherapy
INTRODUCTION
Endometrial cancer (EC) is the fourth most common neoplasia in female patients in the United States of America (USA).[1] A total of 66,200 (7%) newly diagnosed EC patients were recorded in the United States in 2023, with 13,030 (5%) deaths; the prevalence of EC has been rising with older age and severe obesity of the population.[1] The 5-year relative survival was 81% for women diagnosed with endometrial carcinoma in 2013–2019, with values ranging from 94.9% in localized tumor to 18.4% in distant metastasized cancer.[1]
EC emerges from the inner epithelial layer of the uterus and was historically divided into two histopathological subgroups by Bokhman[2] in 1983. The majority of cases, namely, type I endometrioid tumors, including those estrogen receptor-positive or low-grade tumors, display minimal myometrial invasion and a better prognosis than type II tumors.[2] On the other hand, type II tumors include those with aggressive histologies, higher grade, and poor outcomes. Most of the women with endometrial carcinoma have a favorable prognosis, and high-grade tumors may not respond to adjuvant therapy.[3] The diagnosis and treatment of EC remain as subjects of contention due to the irreproducibility of pathological categorization and the lack of consensus among pathologists despite the use of immunohistochemistry.[4] This lack of reproducibility results in the mismanagement of many women in cancer centers globally.[5]
To address these shortfalls, scholars have shown the exceptional findings of the new molecular testing for EC in terms of reproducibility and association with daily clinical practice.[6] The novel molecular classifier called Proactive Molecular Risk Classifier for EC categorizes patients with endometrial carcinoma to 1–4 genomic subgroups based on the results of the Cancer Genome Atlas (TCGA) in 2013 and those of mutation and protein expression analyses.[7] The following subgroups have been created: no specific molecular profile, p53 mutation, DNA polymerase epsilon (POLE) mutation, and microsatellite instability (MSI).[8] This differentiation has led to the creation of a new molecular classification, which is currently integrated into the old International Federation of Gynecology and Obstetrics (FIGO) classification and the European Society of Gynecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology (ESGO/ESTRO/ESP) guidelines for the treatment of EC patients.[9] Thus, our ability to categorize patients in accordance with the new guidelines can contribute to the improvement of the traditional clinicopathological risk group system.[10]
This study aimed to assess the role of the new molecular classification in endometrial carcinoma as a valuable tool for recurrence risk prognosis and appropriate adjuvant treatment planning.
MATERIAL AND METHODS
Study characteristics
We prospectively investigated all women with EC who received treatment in the 1st Department of Obstetrics and Gynecology from January 1, 2022, to March 30, 2024, and selected those who were offered upfront surgery. A total of 120 consecutive patients were diagnosed with endometrial neoplasia in the aforementioned period.
Patients
Inclusion criteria
Histopathological verification of endometrial neoplasia
Surgery at the Gynecological–Oncology Unit.
Exclusion criteria
Refusal to be tested for molecular classification
Diagnosis of a synchronous neoplasm.
After screening in accordance with the inclusion and exclusion criteria, 55 of the 120 women from our cohort were dropped out due to their refusal for molecular testing, due to the high cost of testing (especially for POLE gene mutation) and no government compensation. No patients were excluded due to synchronous neoplasm. Hence, 65 women with EC were considered eligible for statistical analysis, with no duplications and loss of valuable registry data. Figure 1 presents the flowchart of the population of the study.
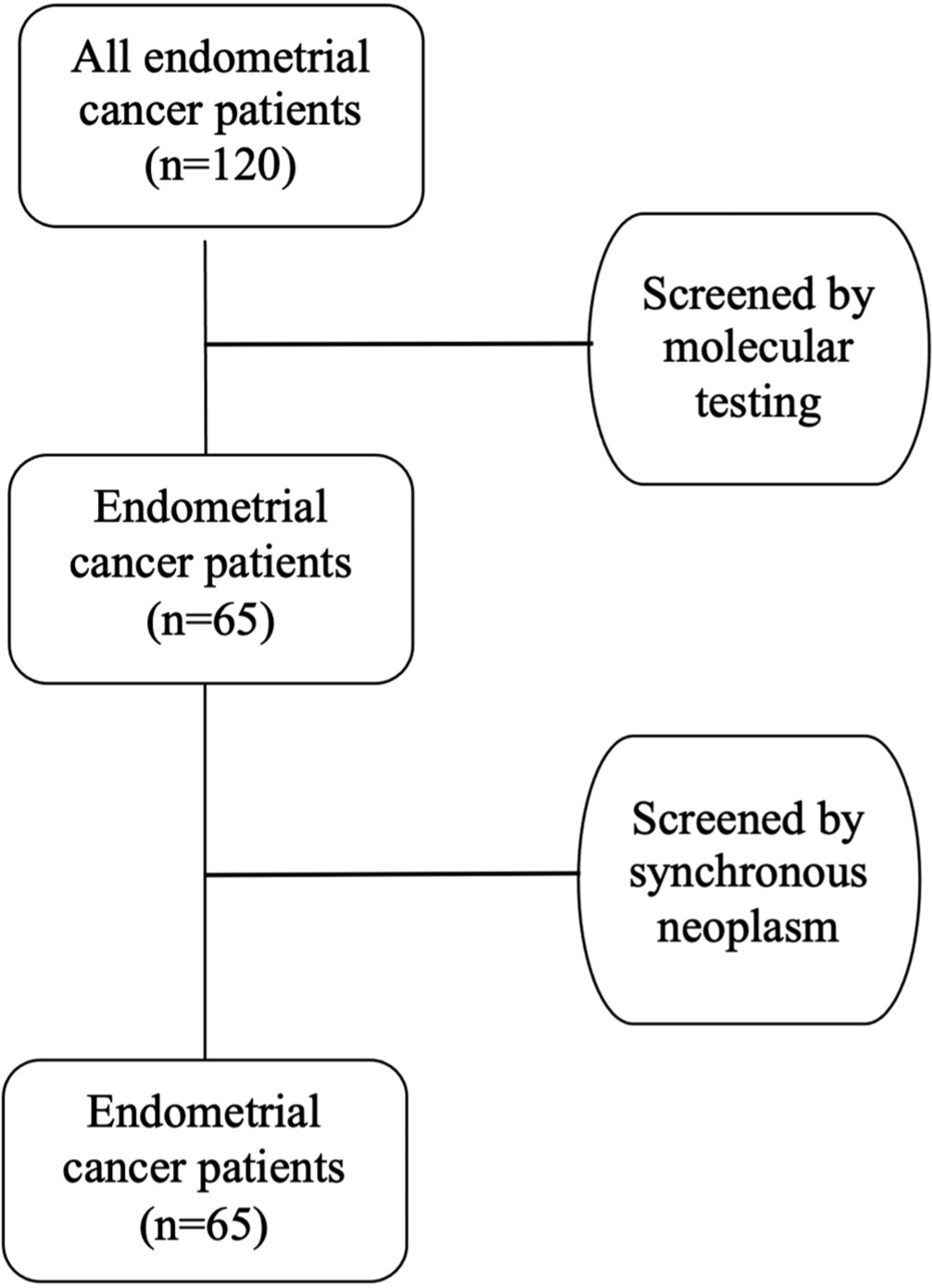
- Patients’ selection flowchart.
Study design
The multidisciplinary tumor (MDT) board conducted pre- and post-operative discussion of all patients in our Gynecological–Oncology Unit. The cases with the traditional pathological analysis were first presented to the members of the MDT board, and a decision regarding the administration and type of adjuvant treatment was made. Then, the cases were presented to the MDT board with the addition of the new molecular classification, and the final decision on the adjuvant treatment was documented. The MDT board meeting decision was made in accordance with the new ESGO/ESTRO/ESP guidelines.[9]
All cases were tested using all the three proposed tests in the literature to intergrade the new molecular classification: First, next-generation sequencing (NGS) sequencing was performed for POLE mutation and MSI status. The POLE gene was checked for mutations in known exonuclease hotspots (11 in total): DNA was extracted through examination mutational analysis of exons 9–14. Sequencing was performed using the Ion Gene Studio S5 Prime System NGS platform (Thermo Fisher Scientific, USA). Moreover, MSI was tested as follows: DNA was extracted from the tumor tissue sample and analyzed via NGS for the 76 markers to assess the MSI status using Ion Ampliseq technology. The Ion Gene S5 Prime System NGS platform was used. The result provides information on individual microsatellites and is used to calculate the MSI score. A test result was considered positive for MSI if the MSI score >30.
Second, immunohistochemistry was utilized to distinguish the various mutant-expression patterns of the p53 gene; four distinct p53 mutant-expression patterns can be identified: Diffuse pattern with a high nuclear positivity, no expression, overexpression in the cytoplasm, and a well-delimited area of the tumor with mutant expression of p53 in a background of wild-type expression.[11]
Statistical analysis
The patient characteristics of this cohort were collected. The flowchart of patients was constructed using Microsoft Word for Mac, version 16.87 (24071426; Microsoft Corporation, USA). No registry data were missing, and further analysis was performed. Concerning descriptive statistics, the mean, median, range, and standard deviation were calculated, and for categorical variables, frequencies and percentages were considered. Categorically paired variables were analyzed using the McNemar test to determine the change in the MDT board decision before and after the integration of the new molecular classification. Statistical significance was set at 0.05 (P < 0.05). R statistical software version 4.3.0 was used for statistical analysis (R Project for Statistical Computing).[12]
Ethical approval and informed consent
The study was conducted in accordance with the Declaration of Helsinki[13] and approved by the Institutional Review Board of the “Papageorgiou” general hospital, number 37577, dated December 10, 2021. A written patient consent was obtained from every patient at the time of the molecular testing proposal and after meticulous explanation of the study protocol.
RESULTS
This prospective cohort study included 65 women diagnosed with EC of any histological type and received treatment at the aforementioned period in our Gynecological–Oncology Unit and who were also tested for POLE mutation, MSI, and p53 mutation to intergrade the new molecular classification. Surgical treatment included total hysterectomy with lymph node staging (either sentinel lymph-node biopsy and/or pelvic with or without para-aortic lymphadenectomy), with or without omentectomy and peritoneal washing cytology.
Table 1 outlines the oncological information. The patients included in this study had a mean age of 65.1 (±12.7) years. All patients were preoperatively tested with Pap smear, and 25 (38.5%) had abnormal results. Specifically, 15 (23.1%) patients were detected with atypical glandular cells (AGC), 10 (15.4%) with atypical squamous cells of undetermined significance, and 40 (61.5%) with a negative result for intraepithelial lesion or malignancy result. A total of 46 (70.8%) patients had endometrioid histology, and 40 (61.5%) exhibited low-grade differentiation. Meanwhile, substantial lymphovascular space invasion (LVSI) was present in 6 (9.2%) patients. No ascites was detected in any case, and peritoneal washing for cytology was performed on all patients: Seven (10.8%) cases had a positive cytology for malignant cancer cells in the peritoneal cavity. Furthermore, concerning the FIGO stage, in accordance with the 2009 classification, more than three quarters (84.6%) of the patients had early-stage disease confined to uterus corpus (FIGO Stage I).
| Characteristics | Number of patients | Percentage |
|---|---|---|
| Pap smear | ||
| NLIM | 40 | 61.5 |
| ASCUS | 10 | 15.4 |
| AGC | 15 | 23.1 |
| Peritoneal washing cytology | ||
| Positive | 7 | 10.8 |
| Negative | 58 | 89.2 |
| Histologic subtype | ||
| Endometrioid | 46 | 70.8 |
| Undifferentiated | 6 | 9.2 |
| Clear cell | 5 | 7.7 |
| Mixed | 8 | 12.3 |
| Binary FIGO grading | ||
| Low-grade | 40 | 61.5 |
| High-grade | 25 | 38.5 |
| LVSI | ||
| No | 48 | 73.9 |
| Focal | 11 | 16.9 |
| Substantial | 6 | 9.2 |
| FIGO stage | ||
| I | 55 | 84.6 |
| II | 3 | 4.6 |
| III | 7 | 10.8 |
| IV | 0 | 0 |
NLIM: Negative for intraepithelial lesion or malignancy, ASCUS: Atypical squamous cells of undetermined significance, AGC: Atypical glandular cells, FIGO: International federation of gynecology and obstetrics, LVSI: Lymphovascular space invasion
In accordance with the new molecular classification, all patients were tested for POLE mutation, MSI, and p53 mutation, and in 35 (53.8%) out of the 65 patients, a “positive” result in one of the tested markers was received. Specifically, 14 (21.5%) patients were diagnosed with MSI-H and further advised to undergo genetic testing for hereditary non-polyposis colorectal cancer syndrome (Lynch syndrome), 5 (7.7%) patients had a POLE gene mutation, and 17 (26.2%) patients expressed a p53 mutation. One case of multiple classifiers, with a POLE and a p53 mutation, was documented.
Our study aimed to assess the implications in the daily clinical practice of the new molecular classification in patients with EC during the recurrence-risk group prognosis and consequently in adjuvant treatment planning. Out of the 65 patients, the final MDT board changed its decision on 23 cases (35.4%) after molecular testing. McNemar’s test was performed to assess whether a significant change occurred in proportions over time between these 23 cases and the 42 with no change in the final MDT board decision. This test was conducted because certain before-after studies included paired not independent categorical measurements. A statistical significance (P = 0.03469) was observed, which means that a significant number of patients benefited from these comprehensive assessments. Specifically, 6 (9.2%) cases of overtreatment and 17 (26.2%) cases of undertreatment were observed. Specifically, the majority of the cases that would have been overtreated had a POLE gene mutation, and thus, no adjuvant treatment was proposed. Meanwhile, most of the cases that would have been undertreated were classified as p53abn, and they were offered sequential chemotherapy and external beam radiotherapy (ERBT).
DISCUSSION
Historically, Bokhman’s classification of endometrial carcinomas into types I and II tumors, which provides a good tool for understanding most of endometrial carcinomas, served as a landmark.[2] However, the TCGA-based molecular classification offers an improved subclassification system.[7] The data enhance the reproducibility of EC-risk group categorization to provide adequate adjuvant therapy and follow-up program for patients with endometrial carcinoma.
The present study included patients with any histological type of EC of all stages and who underwent total hysterectomy with lymph node staging (either sentinel lymph node biopsy and/or pelvic with or without paraaortic lymphadenectomy) with peritoneal washing cytology, irrespective of the adjuvant treatment given. However, peritoneal washing cytology is excluded in the 2009 FIGO staging revision[14] and currently in the new 2023 FIGO staging[15] for endometrial carcinoma; studies showed that this technique may have important prognostic significance[16,17] in certain patients and should not be abandoned.[18,19] Furthermore, all our cases were tested preoperatively with a Pap smear. AGC cells were found in 15 (23.1%) cases, which shows an association between the cytopathological results of Pap smear and EC; this outcome was also described in literature[20] and implies the need for differentiation from glandular cervical cancer.[21]
All cases have been tested through POLE sequencing, MSI assay, and p53 immunohistochemistry testing. Of the included 65 patients, 35 (54%) had a “positive” result on any of the three markers of molecular classification. A total of 14 patients were grouped into the MSI group, five into the POLE mutation group, and 17 into the p53 abnormal expression group, with one case of a multiple classifier: POLEmut and p53abn. However, one case revealed the importance of investigating all three markers, especially through POLE sequencing, which is often omitted due to cost or unavailability. This patient would have been classified as p53abn and would have undergone unnecessary sequentially chemotherapy and ERBT.
Furthermore, the final MDT board changed its decision on 23 cases (35.4%) after the integration of molecular classification: Six cases of overtreatment and 17 cases of undertreatment, with a statistical difference (P = 0.003469). Finally, from the 14 MSI-H results, 4 led to an MDT board decision. However, all women were counseled regarding the possibility of Lynch syndrome and underwent further gene testing.
To the best of our knowledge, this work is the first prospective cohort study that showed the strong prognostic effect of the new molecular classification on endometrial carcinoma in daily clinical practice. Although the new molecular classification has been integrated in the latest FIGO staging of EC,[15] questions about the competence of the traditional classification and its possible implications in the recurrence-risk prognosis of patients remain, especially for POLE mutation.[22] Most publications[23,24] comprise large retrospective studies that investigated high-grade endometrioid endometrial carcinoma and concluded that it is a heterogenous group that can be further subclassified by molecular subtypes to identify those with a better prognosis. On the other hand, post hoc analysis of the randomized trials PORTEC-1, PORTEC-2,[25] and PORTEC-3,[26] which investigated the molecular profile of the patients, revealed a strong association between the new molecular classification and the need for adjuvant treatment to render it with an important predictive value.
This work is the first prospective research that investigated the implementation of the new molecular testing for EC and its effect on daily clinical practice and specifically the MDT board decision change. The main advantage of this cohort study is its prospective nature and the condition that all patients were tested for all three markers at the same laboratory through the same method. Moreover, all patients’ data were collected using the online database of the Gynecological–Oncology Unit of the 1st Department of Obstetrics and Gynecology, which minimized the missing data to zero. On the contrary, the main limitation of this study is the relatively small population included in the final analysis although a statistical significance in the MDT board decision change was observed.
The results of our study further validate the role of the new molecular classification in recurrence-risk prognosis and improved planning of adjuvant treatment. Future research should include patients with any histological type who will undergo testing in molecular subgroups and investigate specific targeted adjuvant therapies within specific molecular subgroups, such as the EUGENIE study.[27]
SUMMARY
Our study showed the strong prognostic effect of the new molecular classification and its great potential in determining the appropriate adjuvant therapy. The molecular classification, which includes testing for POLE mutation, MSI, and p53 mutation, must be implemented in clinical diagnostic procedures and decision-making. However, clinicians should constantly keep in mind the traditional criteria for classification, such as FIGO stage, tumor size, and LVSI.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
ABBREVIATIONS
FIGO – International Federation of Gynecology and Obstetrics
MDT – Multidisciplinary tumor
MSI – Microsatellite instability
POLE – DNA polymerase epsilon
EC – Endometrial cancer
USA – United States of America
TCGA – The cancer genome atlas
ESGO – European Society of Gynecological Oncology
ESTRO – European Society for Radiotherapy and Oncology
ESP – European society of pathology
AGC – Atypical glandular cells
ASCUS – Atypical squamous cells of undetermined significance
LVSI – Lymphovascular space invasion
ERBT – External beam radiotherapy
AUTHOR CONTRIBUTIONS
DZ and DT: Designed the study; all authors conducted the study; SP: Provided laboratory samples; MT: Developed the methodology of the study; DZ, IS and PT: Collected and analyzed the data; DZ, IS and DT: Participated in drafting the manuscript, and all authors contributed to critical revision of the manuscript for important intellectual content; ET and GG: Supervised the study. All authors gave final approval of the version to be published. All authors participated fully in the work, took public responsibility for appropriate portions of the content, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or completeness of any part of the work were appropriately investigated and resolved.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research/study was approved by the Institutional Review Board of “Papageorgiou” general hospital, number 37577, dated 10-12-2021, and was performed in accordance with the principles of the Declaration of Helsinki. The authors certify that they have obtained all appropriate patient consent.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
EDITORIAL/PEER REVIEW
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through an automatic online system.
FUNDING
Not applicable.
References
- Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15:10-7.
- [CrossRef] [PubMed] [Google Scholar]
- Adjuvant chemoradiotherapy versus radiotherapy alone in women with high-risk endometrial cancer (PORTEC-3): Patterns of recurrence and post-hoc survival analysis of a randomised phase 3 trial. Lancet Oncol. 2019;20:1273-85.
- [CrossRef] [PubMed] [Google Scholar]
- The immunohistochemical molecular risk classification in endometrial cancer: A pragmatic and high-reproducibility method. Gynecol Oncol. 2022;165:585-93.
- [CrossRef] [PubMed] [Google Scholar]
- Poor interobserver reproducibility in the diagnosis of high-grade endometrial carcinoma. Am J Surg Pathol. 2013;37:874-81.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular profiling of endometrial cancer from TCGA to clinical practice. J Natl Compr Canc Netw. 2023;21:210-6.
- [CrossRef] [PubMed] [Google Scholar]
- Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67-73.
- [CrossRef] [PubMed] [Google Scholar]
- Confirmation of ProMisE: A simple, genomics-based clinical classifier for endometrial cancer. Cancer. 2017;123:802-13.
- [CrossRef] [PubMed] [Google Scholar]
- ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int J Gynecol Cancer. 2021;31:12-39.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of endometrial carcinoma: More than two types. Lancet Oncol. 2014;15:e268-78.
- [CrossRef] [PubMed] [Google Scholar]
- p53 immunohistochemistry is an accurate surrogate for TP53 mutational analysis in endometrial carcinoma biopsies. J Pathol. 2020;250:336-45.
- [CrossRef] [PubMed] [Google Scholar]
- Exact McNemar's test and matching condence intervals. 2020. Available from: https://cloudr-project.org/web/packages/exact2x2/vignettes/exactmcnemar.pdf [Last accessed on 2024 Sep 05]
- [Google Scholar]
- WMA-The World Medical Association. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-formedical-research-involving-human-subjects [Last accessed on 2024 Sep 25]
- [Google Scholar]
- Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009;105:103-4.
- [CrossRef] [PubMed] [Google Scholar]
- FIGO staging of endometrial cancer: 2023. J Gynecol Oncol. 2023;34:e85.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic significance of positive peritoneal cytology in endometrial cancer patients. J Obstet Gynaecol. 2022;42:2336-40.
- [CrossRef] [PubMed] [Google Scholar]
- Clinico-pathological significance of suspicious peritoneal cytology in endometrial cancer. J Surg Oncol. 2021;124:687-98.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant peritoneal cytology in endometrial cancer: A contemporary review. Expert Rev Anticancer Ther. 2022;22:947-55.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in peritoneal cytology evaluation at hysterectomy for endometrial cancer in the United States. Gynecol Oncol. 2021;161:710-9.
- [CrossRef] [PubMed] [Google Scholar]
- How useful are cervical Pap smears in detecting endometrial carcinomas? A tertiary cancer center experience. Diagn Cytopathol. 2021;49:127-31.
- [CrossRef] [PubMed] [Google Scholar]
- Detection rates and factors affecting thereof in endometrial hyperplasia, endometrial carcinoma, and cervical glandular lesions on cervical smear. Cancer Med. 2023;12:17581-91.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes of patients with POLE mutated endometrioid endometrial cancer. Gynecol Oncol. 2020;156:194-202.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathological and molecular characterization of high-grade endometrial carcinoma with POLE mutation: A single center study. J Gynecol Oncol. 2022;33:e38.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular classification of grade 3 endometrioid endometrial cancers identifies distinct prognostic subgroups. Am J Surg Pathol. 2018;42:561-8.
- [CrossRef] [PubMed] [Google Scholar]
- Interpretable deep learning model to predict the molecular classification of endometrial cancer from haematoxylin and eosin-stained whole-slide images: A combined analysis of the PORTEC randomised trials and clinical cohorts. Lancet Digit Health. 2023;5:e71-82.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular classification of the PORTEC-3 trial for high-risk endometrial cancer: Impact on prognosis and benefit from adjuvant therapy. J Clin Oncol. 2020;38:3388-97.
- [CrossRef] [PubMed] [Google Scholar]
- Improving endometrial cancer assessment by combining the new technique of genomic profiling with surgical extra uterine disease assessment (EUGENIE) Int J Gynecol Cancer. 2023;33:823-6.
- [CrossRef] [PubMed] [Google Scholar]








