Translate this page into:
Pitfall in immunohistochemical staining for thyroglobulin in case of thyroid metastasis from lung carcinoma
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 73-year-old female presented with an enlarging neck mass over the last 2 years. She then started experiencing hoarseness, dysphagia, and weight loss for 5 months. Physical examination showed an irregular and hard consistency mass with a diameter of 4 cm occupying the left lobe and isthmus of the thyroid gland. Fine-needle aspiration biopsy (FNAB) was performed and the cytology specimen revealed sheets of neoplastic cells with enlarged, hyperchromatic, slightly pleomorphic nuclei, prominent nucleoli, and brownish pigment inside the tumor cells [Figure 1a]. The definitive diagnosis could not be made from cytology alone. Immunohistochemical staining was requested with positive results for thyroglobulin [Figure 1b], thyroid transcription factor 1 (TTF-1) [Figure 1c], but negative for calcitonin.
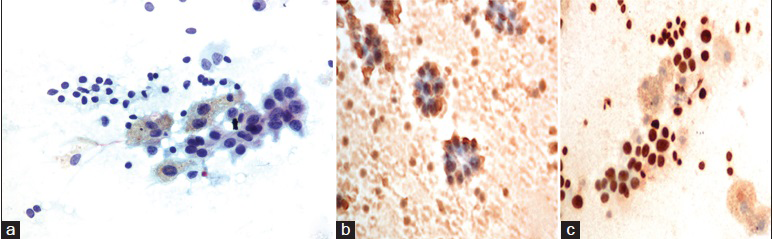
- (a) Fine-needle aspiration thyroid showed a background of cystic lesion (foamy cells) with few of neoplastic cells and a sheet of degenerative follicular cells (Papanicolaou stain, ×400), (b) cell block preparation showed the immunoreactivity to thyroglobulin was false positive and was seen in the contaminated thyroid follicular cells/background but not in the neoplastic cells (immunohistochemical stain for thyroglobulin, ×400), (c) neoplastic cells showed positive nuclear stained pattern (immunohistochemical stain for thyroid transcription factor 1, ×400)
QUESTION
Q1: What is the most specific immunohistochemical marker for differentiated thyroid cancer?
-
Thyroglobulin
-
TTF-1
-
Calcitonin
-
Chromogranin.
ANSWER
Q1: Thyroglobulin.
Following the clinical information, we considered the differential diagnosis between primary thyroid cancer and thyroid metastasis. FNAB cytology alone may not be as useful in distinguishing metastatic high-grade malignancy from poorly differentiated or anaplastic primary thyroid carcinoma.[1] There have been reports of diagnostic difficulties of thyroid metastasis from cytology[2] and misdiagnosis of adenocarcinoma metastasis to the thyroid gland as primary thyroid carcinoma due to the similarity of FNAB cytology between the tumors.[3]
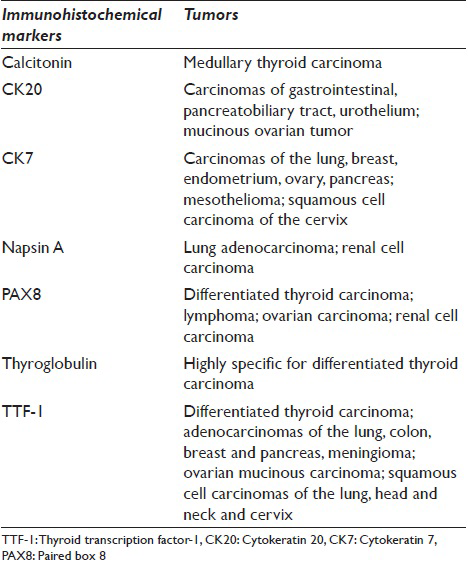
Immunohistochemical studies, especially TTF-1, thyroglobulin, and calcitonin are good adjunctive to FNAB. Table 1 demonstrates the immunohistochemical markers and the corresponding tumors.[456] TTF-1 is a transcription factor expressed in lung and thyroid epithelial cells. It is also expressed in prostate, stomach, salivary gland, colon tumors, and urothelial carcinoma. It is highly sensitive in the detection of lung and thyroid carcinoma. On the contrary, thyroglobulin is a specific marker for differentiated thyroid cancer, and it is positive in only 20-30% of anaplastic thyroid carcinoma.[16] However, a negative thyroglobulin and positive TTF-1 can be found in medullary thyroid carcinoma. Therefore, calcitonin immunohistochemical stain or serum calcitonin should be performed if medullary thyroid carcinoma is suspected.[6]
FOLLOW-UP OF THE PRESENT CASE
The patient's thyroid function tests were as follows: FT4 1.64 μg/dL (0.7–1.48), T3 74 ng/dL (58–159), and thyroid-stimulating hormone 0.015 mIU/L (0.35–4.94). Computed tomography (CT) scan of the neck showed a large lobular enhancing thyroid mass with central necrosis and multiple small calcifications with an epicenter at the left and pyramidal thyroid lobes, measuring 5.6 × 2.9 × 6.8 cm, accompanied by multiple necrotic cervical and mediastinal lymph nodes [Figure 2]. Chest CT showed a 3 cm mass in the right middle lung abutting the major fissure with multiple small nodules in both lungs and multiple enlarged mediastinal lymph nodes [Figure 3a]. A small right adrenal gland nodule was also found. CT scan of her brain demonstrated multiple brain metastases [Figure 3b]. A bone scan found multiple areas of increased uptakes in the vertebrae, left femoral neck, proximal left fibula, and parietal bone [Figure 3c].

- Computed tomography neck showed a 5.6 × 2.9 × 6.8 cm lobulated enhancing thyroid mass with central necrosis and multiple small calcifications at left and pyramidal thyroid lobes (arrow) with multiple necrotic cervical lymphadenopathies
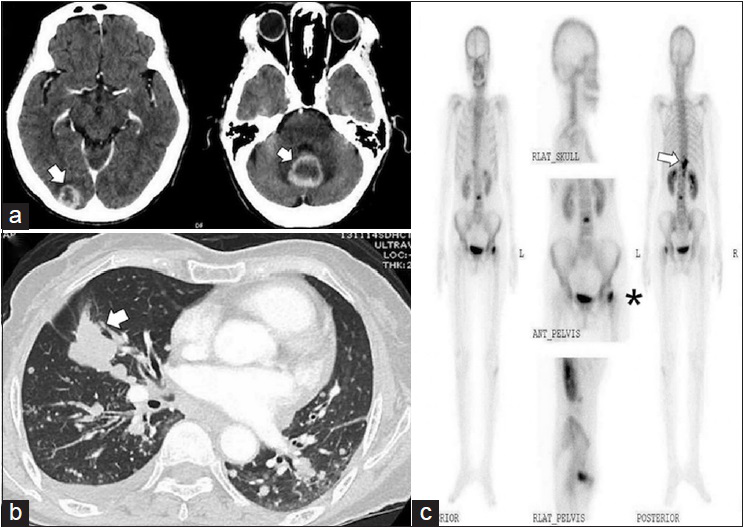
- (a) Computed tomography brain showed multiple brain metastases (arrows), (b) computed tomography chest and mediastinum showed a 3 cm mass at right middle lung (arrow) abut major fissure with multiple small nodules in both lungs and multiple mediastinal lymphadenopathies, (c) bone scan found increase uptake in her vertebrae (arrow), left femoral neck (*), proximal left fibula and parietal bone
The patient was diagnosed with poorly differentiated thyroid carcinoma with distant metastases. She underwent total thyroidectomy with radical neck dissection to relieve her compressive symptoms and to obtain tissue for pathological diagnosis. Histologic sections revealed nodular goiter and small foci of carcinoma in glandular and papillary formations in the left lobe of the thyroid [Figure 4a]. Immunohistochemical staining was slightly positive for thyroglobulin in the background thyroid follicular cells, positive for cytokeratin 7 and TTF-1, and negative for cytokeratin 20 in the neoplastic cells [Figure 4b and c]. Her biopsied cervical lymph node also showed metastatic carcinoma [Figure 4d] with positive immunohistochemical stain for TTF-1, but negative for thyroglobulin [Figure 4e and f]. The definite diagnosis was changed to poorly differentiated lung adenocarcinoma with metastasis to the thyroid gland. After surgery, the patient received palliative whole-brain radiation therapy. Unfortunately, she passed away 7 months after diagnosis.
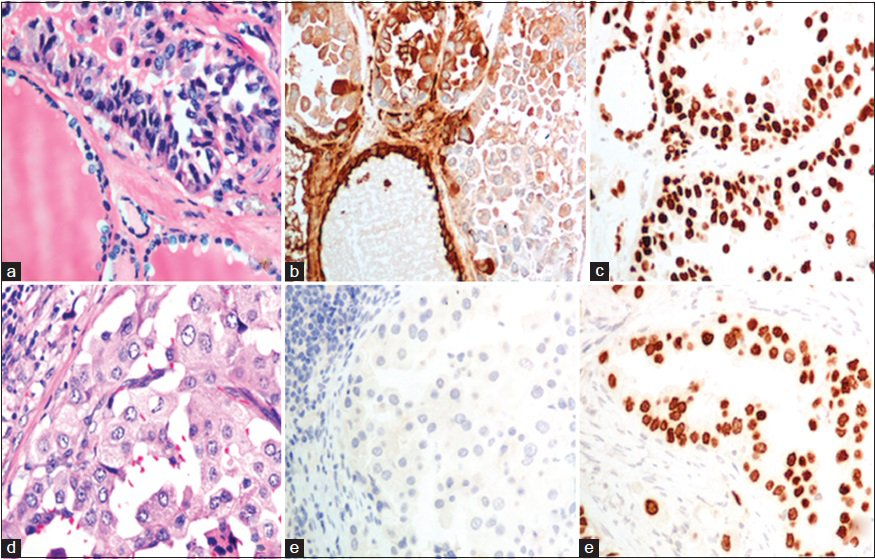
- (a) Thyroidectomy specimen demonstrated neoplastic cells in nodular goiter (H and E, ×400), (b) Thyroidectomy specimen demonstrated heterogeneous positive immunoreactivity to thyroglobulin (immunohistochemical for thyroglobulin, ×400), (c) Thyroidectomy specimen demonstrated nuclear stained pattern in tumor cells and follicular cells (immunohistochemical for thyroid transcription factor-1, ×400), (d) Lymph node containing metastatic carcinoma (H and E, ×400), (e) Lymph node demonstrated completely negative immunoreactivity to thyroglobulin (immunohistochemical for thyroglobulin, ×400), (f) Lymph node demonstrated nuclear stained pattern in tumor cells (immunohistochemical for thyroid transcription factor-1, ×400)
ADDITIONAL QUIZ QUESTIONS
Q2: What is the most frequent primary cancer that metastasized to the thyroid gland?
-
Lung carcinoma
-
Renal cell carcinoma
-
Hepatocellular carcinoma
-
Malignant melanoma
-
Lymphoma.
Q3. What is the usual management of thyroid metastasis?
-
Levothyroxine suppression
-
Lobectomy
-
Radioactive iodine
-
Prophylactic radiation
-
Treatment of primary malignancy.
ANSWERS TO ADDITIONAL QUIZ QUESTIONS
Q2. (B): The most common tumor that metastasizes to the thyroid gland is renal cell carcinoma. Following renal cell carcinoma, the next most common tumors are colorectal, lung, and breast carcinoma.
Q3. (E): Management of thyroid metastasis depends on the primary site of the tumor, the presence of other metastases and symptoms caused by thyroid mass. Despite thyroid, metastasis is associated with poor prognosis aggressive surgical treatment could be applied for the selected patients such as isolated metastasis, especially from renal cell carcinoma. The radiation therapy can help to relieve symptom and should be considered in the patients with high risk for surgery. There is no role for radioactive iodine therapy and levothyroxine suppression therapy.
BRIEF REVIEW OF THIS TOPIC
Thyroid metastasis
Although the thyroid gland is the second most vascularized organ in the body, metastasis to the thyroid gland is uncommon and usually indicates a poor prognosis.[7] It previously had been reported in autopsy case series, but it is now believed to be more commonly diagnosed due to the more frequently performed FNAB and improved survival of patients with disseminated cancer.[1] The increase in thyroid metastasis incidence is also a result of increased surveillance from imaging studies such as ultrasound and more accurate diagnostic methods including ultrasound-guided FNAB.[8] Recent data show the mean prevalence of 0.16% of secondary neoplasm of the thyroid gland in all thyroid FNAB and 1.9% of malignant thyroid FNAB.[8] Most commonly found primary tumors have usually been renal cell carcinoma or breast cancer followed by lung cancer. Primary lung cancer with thyroid metastasis is found in 13–26% of all thyroid metastases. In addition, thyroid metastasis from melanoma and sarcoma are also common.[8910]
Clinical presentation
Thyroid metastasis occurs in generally equal sexual distributions with a slight female predominance (1.2–1.4:1) and a mean patient age of 59 years.[811] The majority of patients with thyroid metastasis presented as thyroid nodules or goiter with compressive symptoms, but the minority of cases were found incidentally.[11] From a recent cohort, 58% of patients with thyroid metastasis had histories of malignancy, while 18% were without a known history of malignancy.[8] Most thyroid metastases and their primary tumors are metachronous with a mean interval of 69.9 months between detection of primary tumors and thyroid metastases. However, lung cancer presents synchronously with thyroid metastasis.[11] In rare cases, lung adenocarcinoma can initially manifest as a thyroid nodule.[12] Although most of the literature did not clearly define patients’ thyroid function and underlying thyroid pathology, most patients were euthyroid, and a significant number of patients had preexisting thyroid pathology. Patients with underlying thyroid pathologies, such as multinodular goiter, are more susceptible to thyroid metastasis due to blood supply abnormality leading to decreased oxygen and iodine content.[11] Furthermore, it is not unusual for patients to present with thyrotoxicosis similar to our patient. Thyrotoxicosis can be a result of the destruction of thyroid tissues by the tumor cells causing destructive thyroiditis leading to the leakage of hormones into the bloodstream,[11] preexisting toxic multinodular goiter, or both.
Role of fine-needle aspiration biopsy: Accuracy and pitfalls
FNAB is an accurate, convenient, and inexpensive method for the diagnosis of thyroid nodule. Its sensitivity and specificity, from a cohort of 62 patients with secondary neoplasm of thyroid gland in the United States and Europe, are 87% and 93%, respectively.[8] It generally provides a correct diagnosis in 90% of metastases from lung cancer.[11] However, as described in our case report, the diagnosis cannot be made on the basis of cytology alone. The most common diagnostic pitfall is metastatic renal cell carcinoma which is difficult to distinguish from Hürthle cells carcinoma due to its cytological features.[8] Underlying multinodular goiter can decrease the accuracy of FNAB with a false negative rate of 3.6%. The risk of false negatives rises as nodules size increases. Multinodular goiter can also cause errors in interpretation from accidental needle puncture through colloid nodules.[1113] Other potential pitfalls in interpretation include inadequate samplings and lack of information on primary tumors for immunohistochemical staining.[914]
Poorly differentiated thyroid carcinoma, previously known as insular carcinoma, is rare and clinically aggressive. Its cytomorphologic features are highly cellular with scant colloid and rare necrosis. The cells are arranged in loosely cohesive solid, trabecular, or insular patterns. Its cells are medium-size with scant cytoplasm, round nucleoli, and a high nuclear-cytoplasmic ratio.[1516] Its features are quite similar to high-grade thyroid metastasis. Positive immunohistochemical stains for TTF-1 and thyroglobulin usually exclude metastasis. However in our case, thyroglobulin were positive possibly, because diffusion artifact of thyroglobulin from surrounding thyroid follicles or possibly from a needle punctured through colloid nodules of multinodular goiter leading to misdiagnosis.[16]
Prognosis and treatment
Overall prognosis for patients with thyroid metastasis cancer was 24% after 4.5 years depending on primary cancer. Renal cell carcinoma had the best prognosis among others. The role of surgery is controversial in thyroid metastasis. In anaplastic thyroid carcinoma, the decision to perform surgery is determined by the resectability of the tumor.[17] However in thyroid metastasis, types of primary tumor and the presence of metastases to other organs must be taken into account. Surgical intervention should only be considered in patients with renal cell carcinoma with solitary thyroid metastasis or in patients with signs and symptoms of tracheal or esophageal compressions and should not be performed in patients with widespread metastases from any primary cancer. It is still unclear whether total thyroidectomy is beneficial, but thyroid lobectomy should be performed in patients with the tumor confined in a single lobe to preserve thyroid function.[91114] In patients with polymetastatic cancer, systemic treatment such as chemotherapy and targeted therapy should be considered. There has been a report of lung cancer with mutations in epidermal growth factor receptor (EGFR) showing marked response from EGFR inhibitor.[2] In our patient's case, even though it was a misdiagnosis, total thyroidectomy was beneficial. The surgery reduced her compressive symptoms and demonstrated true pathological diagnosis, due to the fact that her underlying goiter reduced the diagnostic accuracy of FNAB.[11]
CONCLUSIONS
Evaluating poorly differentiated malignant neoplasm of the thyroid gland is a challenge, due to overlapping cytopathological features of poorly differentiated thyroid cancer and thyroid metastasis. Immunohistochemical staining, especially thyroglobulin usually helps lead to accurate diagnosis. However, it is not as ideal as previously thought. As it was demonstrated in our patient, false positive thyroglobulin can occur with underlying nodular goiter, possibly from diffusion of thyroglobulin from surrounding tissues. The interpreting immunoreactivity to thyroglobulin should be done with caution. The immunoreactivity should be seen in the tumor cells – not in the background and/or thyroid follicular cells. It is important for physicians to be aware of the possibility of thyroid metastasis when evaluating poorly differentiated primary thyroid carcinoma in patients with underlying thyroid pathology, even with suggestive immunohistochemical markers.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author.
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
ETHICS STATEMENT BY ALL AUTHORS
This Quiz has been reviewed and approved by the Committee on Human Rights Related to Research Involving Human Subjects, Faculty of Medicine Ramathibodi Hospital, Mahidol University.
LIST OF ABBREVIATIONS (In alphabetic order)
CT - Computed Tomography
EGFR - Epidermal Growth Factor Receptor
FNAB - Fine-Needle Aspiration Biopsy
TTF-1 - Thyroid Transcription Factor 1
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and the highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2015/12/1/27/170734
REFERENCES
- Metastasis to the thyroid diagnosed by fine-needle aspiration biopsy. Clin Endocrinol (Oxf). 2005;62:236-41.
- [Google Scholar]
- Lung cancer, thyroid cancer or both: An unusual case presentation. J Thorac Dis. 2011;3:271-3.
- [Google Scholar]
- Metastasis to the thyroid from lung adenocarcinoma mimicking thyroid carcinoma. Jpn J Thorac Cardiovasc Surg. 2004;52:353-6.
- [Google Scholar]
- Use of thyroid transcription factor 1, PE-10, and cytokeratins 7 and 20 in discriminating between primary lung carcinomas and metastatic lesions in fine-needle aspiration biopsy specimens. Cancer. 2001;93:330-6.
- [Google Scholar]
- The value of thyroid transcription factor-1 in cytologic preparations as a marker for metastatic adenocarcinoma of lung origin. Am J Clin Pathol. 2001;116:483-8.
- [Google Scholar]
- Cytomorphologic overlap of differentiated thyroid carcinoma and lung adenocarcinoma and diagnostic value of TTF-1 and TGB on cytologic material. Diagn Cytopathol. 2014;42:5-10.
- [Google Scholar]
- Fine-needle aspiration biopsy of secondary neoplasms of the thyroid gland: A multi-institutional study of 62 cases. Cancer Cytopathol. 2015;123:19-29.
- [Google Scholar]
- Management and prognosis of metastases to the thyroid gland. J Am Coll Surg. 2005;200:203-7.
- [Google Scholar]
- Metastases to the thyroid: A review of the literature from the last decade. Thyroid. 2012;22:258-68.
- [Google Scholar]
- From the diagnostic investigations of goiter to the diagnosis of lung cancer - Case study. Thyroid Res. 2014;7:1.
- [Google Scholar]
- Assessing the risk of false-negative fine-needle aspiration cytology and of incidental cancer in nodular goiter. Endocr Pract. 2013;19:444-50.
- [Google Scholar]
- Thyroid metastasis from nonsmall cell lung cancer. Case Rep Oncol Med 2013 2013 208213
- [Google Scholar]
- Poorly differentiated thyroid carcinoma: A cytologic-histologic review. Adv Anat Pathol. 2009;16:283-9.
- [Google Scholar]
- Cytomorphologic features of poorly differentiated thyroid carcinoma: A multi-institutional analysis of 40 cases. Cancer. 2009;117:185-94.
- [Google Scholar]
- American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2012;22:1104-39.
- [Google Scholar]







