Translate this page into:
Retropharyngeal SOL: An unusual presentation of a multifaceted entity
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 33-year-old female presented with difficulty in swallowing (to both solids and liquids) over 2 months. However, she had no complaints of cough, fever, chest pain, weight loss, or any bone pains without significant past history. Blood and serological investigations including blood sugar, liver function test, kidney function test, and viral serology were within normal limits except for a mild elevation in erythrocyte sedimentation rate (34 mm/h). Endoscopic examination of the nasopharynx and oropharynx revealed edematous posterior pharyngeal wall with intact mucosa and an approximately 3 cm × 3 cm diffuse bulge in the posterior pharyngeal wall on the right side, involving the nasopharynx, part of oropharynx, and reaching up to the midline. Her chest X-ray was unremarkable. Contrast-enhanced computed tomography scan of the neck revealed an oblong hypodense nonenhancing lesion of about 3 cm × 2 cm in the right paramedian retropharyngeal space. The lesion was causing medial displacement of the right pharyngeal tonsils with attenuation of oropharyngeal air space, suggesting an infectious etiology. An endoscopy-guided fine needle aspiration from the retropharyngeal bulge was carried out and smears were prepared [Figure 1a and b].
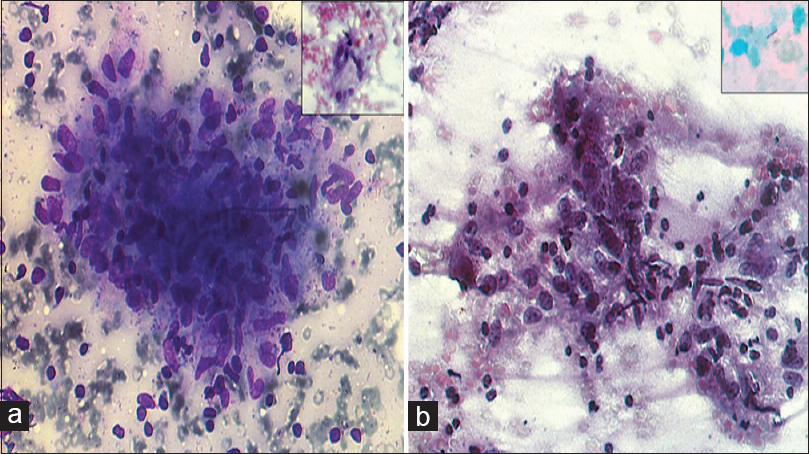
- (a) Fine-needle aspiration findings: Epithelioid cell granuloma (Giemsa, ×400). Multinucleate Langhans' type giant cell (Inset; PAP, ×400). (b)Fine-needle aspiration findings: Lymphohistiocytic cell aggregates (PAP, ×400). Acid-fast bacilli (Inset; ×1000)
QUESTION
Q1: What is your Interpretation?
-
Suppurative lymphadenitis
-
Granulomatous lymphadenitis
-
Neoplastic
-
Inadequate for opinion.
ANSWER
1. B) Granulomatous lymphadenitis.
Retropharyngeal lymph nodes lie deep in the buccopharyngeal fascia [Figure 2] and drain the nasal cavities, nasal part of pharynx, and the auditory tube. A retropharyngeal abscess is an infection in one of the deep spaces of the neck resulting from suppuration of the retropharyngeal lymph nodes.[12]
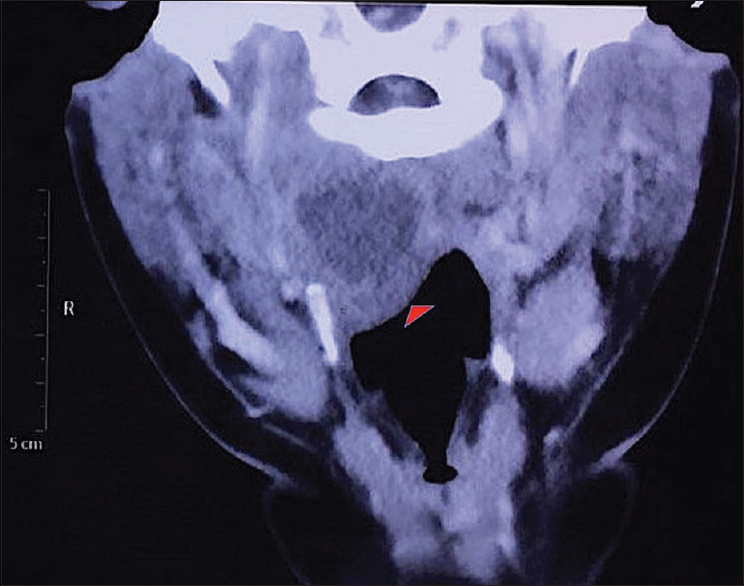
- Contrast-enhanced computed tomography neck scan (axial view): Oblong hypodense lesion in the right paramedian retropharyngeal space (arrow) causing attenuation of oropharyngeal air space
Causes of granulomatous lymphadenitis include;[34]
-
Infections:
-
Bacterial: tuberculosis (TB), leprosy, cat scratch disease
-
Parasitic: leishmaniasis, toxoplasma
-
Viral: EBV, CMV, HCV
-
Fungal: cryptococcosis, histoplasmosis, pneumocystis,
-
Coccidioidomycosis
-
Spirochetes: syphilis, yaws, pinta.
-
-
Autoimmune causes: sarcoidosis, Crohn's disease
-
Foreign body granulomas: suture material
-
Drugs: Allopurinol, oral contraceptives, oxacillin, and amiodarone.
-
Neoplastic: Hodgkin's lymphoma, seminoma, and others
ADDITIONAL QUESTIONS
Q2: What Stain has been Used for Confirmation of etiology (Inset Figure 1b)?
-
PAS Stain
-
Ziehl Neelsen (Z-N) stain
-
GMS Stain
-
Reticulin stain.
Q3: What is not a common cause of primary retropharyngeal abscess?
-
Staphylococcus aureus
-
Bacteroides
-
Haemophilus
-
Mycobacterium
Q4: Which is the most sensitive test for tuberculosis diagnosis?
-
QuantiFERON TB Gold
-
Smear microscopy
-
GeneXpert MTB
-
Mantoux tuberculin skin test
ANSWERS
2. B) Z-N stain.
Ziehl Neelsen stain is commonly applied for staining Mycobacterium sp. The cell wall of mycobacteria contains high concentration of lipid making them waxy, hydrophobic, and impermeable to routine stain such as the Gram stain. The phenolic compound carbol fuchsin is used as the primary stain because it is lipid soluble and penetrates the waxy cell wall. However, the tubercle bacilli are resistant to decolorization by acid and alcohol and are described as acid-fast bacilli (AFB) or acid-alcohol fast bacilli.[56] Following decolorization, the smear is counterstained with malachite green or methylene blue which stains the background material, providing a contrast color against which the red AFB can be seen. Other acid-fast organisms are cysts of Cryptosporidium and Isospora, Nocardia sp., Rhodococcus sp., and Legionella micdadei.
3. D) Mycobacterium
The common causative organisms of primary retropharyngeal abscess include[789]
-
Aerobic organisms – Beta-hemolytic streptococci, Staphylococcus aureus, Haemophilus, Neisseria sp.
-
Anaerobic organisms – Bacteroides, Veillonella, Prevotella, Fusobacterium, Peptostreptococcus, and Bacteroides
-
Other uncommon organisms: Mycobacterium sp.
4. C) GeneXpert MTB
GeneXpert MTB > smear microscopy > Mantoux tuberculin skin test~
QuantiFERON TB Gold test.
The GeneXpert utilizes a DNA-polymerase chain reaction (PCR) technique for simultaneous detection of Mycobacterium TB and Rifampicin resistance-related mutations. It is a cartridge-based nucleic acid amplification assay for TB detection that includes all necessary steps of DNA PCR. It gives results within 2 h. GeneXpert has a higher sensitivity than AFB smear microscopy in respiratory samples. Park et al.[10] in a large-scale study reported the sensitivity and specificity of smear microscopy as 56.8% and 99.6%, respectively, while that of real-time PCR for solid culture was reported as 97.2% and 72.4%, respectively, and for liquid culture was 93.5% and 97.2%, respectively. Congruent results have been reported recently by Agarwal et al. as well.[11] TST and QFT tests help clinicians differentiate people infected with M. tuberculosis from those uninfected. However, a negative reaction to any of the tests does not exclude the diagnosis of TB disease or latent TB infection.[12]
BRIEF REVIEW OF TOPIC
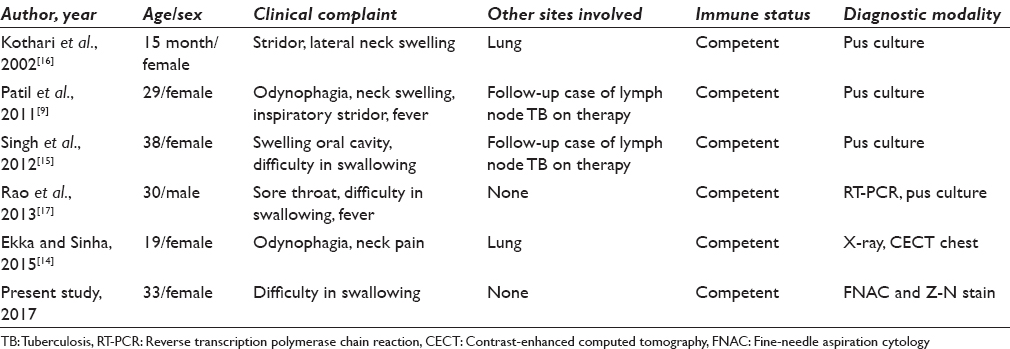
Tubercular retropharyngeal abscess (TRA) is commonly associated with cervical spine TB.[1314] The causative organism M. tuberculosis reaches the skeletal system through hematogenous or lymphatic route and invades the anterior and subchondral portions of the body of the vertebrae. This leads to osteomyelitis along with necrosis and abscess formation. When the abscess formed remains close to the vertebrae, it presents as prevertebral or paravertebral abscess on plain radiograph. The abscess may track distally along tissue plains to form cold abscess. It may bulge into the mouth or the pharynx resulting in odynophagia, dysphagia, pharyngeal discomfort and rarely airway obstruction, respiratory distress, and twelfth-nerve palsy.[13] TRA developing in the absence of cervical spine TB is extremely rare, and only a handful of cases have been reported from India [Table 1].[914151617] Four of these five previously reported cases had TB reported at other sites as well, and pus culture was the technique for a confirmatory diagnosis.
SUMMARY
TB is a diverse disease with patients presenting with overt debilitating disease manifestations to minimal discomfort as was observed in the present case. Retropharyngeal TB is usually secondary to pulmonary or spinal TB. However, in the absence of any such previous history, the possibility of primary infection should not be ruled out. This case highlights unusual presentation of extra pulmonary TB and importance of fine-needle aspiration cytology in rapid diagnosis of deep-seated oropharyngeal lesions, which can often have serious complications due to airway obstruction.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Poojan Agarwal: Conceptualized, drafted the article and gave approval; Manju Kaushal: Contributed to conception, design and gave final approval; Shruti Dogra: Contributed to conception and design; Ankur Gupta: Contributed to conception and design; Nishi Sharma: Contributed to conception and design
ETHICS STATEMENT BY ALL AUTHORS
This study was conducted with approval from Institutional Review Board (IRB) of the institution associated with this study.
LIST OF ABBREVIATIONS (In alphabetic order)
MTB - Mycobacterium Tuberculosis
TB - Tuberculosis
PCR - Polymerase Chain Reaction.
EDITORIAL/PEER REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Parapharyngeal abscess in children: Five year retrospective study. Braz J Otorhinolaryngol. 2009;75:826-30.
- [Google Scholar]
- Retropharyngeal abscess in adults: Five case reports and review of the literature. ScientificWorldJournal. 2011;11:1623-9.
- [Google Scholar]
- Granulomatous infections: Etiology and classification. Clin Infect Dis. 1996;23:146-58.
- [Google Scholar]
- Principles and Interpretation of Laboratory Practices in Surgical Pathology. (1st ed). India: Jaypee; 2016.
- [Google Scholar]
- Medical Microbiology. A Guide to Microbial Infections: Pathogenesis, Immunity, Laboratory Investigation and Control. (8th ed). China: Churchill Livingstone Elsevier; 2012.
- [Google Scholar]
- Principles and Practice of Pediatric Infectious Disease. (4th ed). China: Elsevier Saunders; 2012.
- [Google Scholar]
- Background, Pathophysiology, Epidemiology. Available from: http://www.emedicine.medscape.com/article/764421-overview
- [Google Scholar]
- Tuberculous retropharyngeal abscess without cervical spine TB. Asian Pac J Trop Med. 2011;4:251-2.
- [Google Scholar]
- Evaluation and comparison of molecular and conventional diagnostic tests for detecting tuberculosis in Korea, 2013. Osong Public Health Res Perspect. 2014;5:S3-7.
- [Google Scholar]
- Comparative study of geneXpert with ZN stain and culture in samples of suspected pulmonary tuberculosis. J Clin Diagn Res. 2016;10:DC09-12.
- [Google Scholar]
- Tuberculosis (TB). Centre for Disease Control and Prevention. Available from: http://www.cdc.gov/tb/education/corecurr/pdf/chapter 4pdf
- [Google Scholar]
- Cervical spine tuberculosis and retropharyngeal abscess in an adult Nigerian. Ann Trop Med Public Health. 2012;5:587-90.
- [Google Scholar]
- Retropharyngeal abscess as a rare presentation of pulmonary tuberculosis. Lung India. 2015;32:262-4.
- [Google Scholar]
- An unusual cause of stridor: Retropharyngeal cold abscess. Pediatr Surg Int. 2002;18:165-7.
- [Google Scholar]
- Tuberculosis of the parapharyngeal space: A rare case report. Indian J Pathol Microbiol. 2013;56:480-1.
- [Google Scholar]







