Translate this page into:
Urine cytology: Pitfall due to a “remnant” lesion
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 36-year-old G0 P0 woman presented with complaints of increased urinary frequency and nocturia. She did not report incontinence, dysuria, gross hematuria, or other medical history. Radiologic evaluation showed 2.6 cm irregular, solid and cystic lesion in the superior wall of the bladder, located immediately right of the midline. Cytopathologic findings in voided urine were as shown in Figure 1.
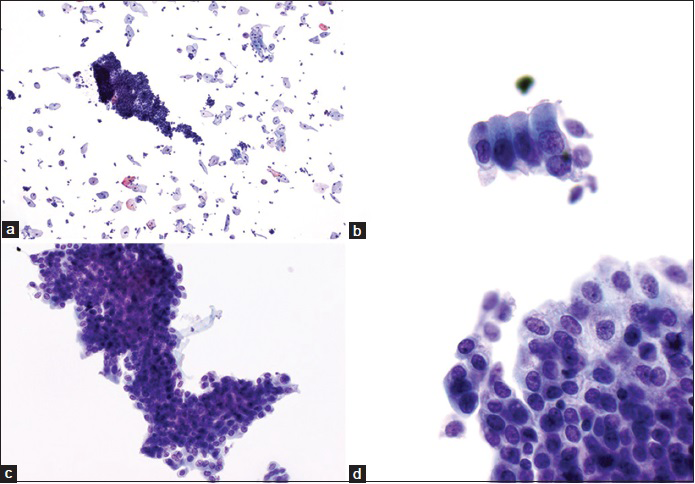
- Voided urine cytology in a liquid based (ThinPrep) preparation. (a) Large cohesive sheet of glandular epithelium with ragged outline (ThinPrep, Papanicolaou stain, ×100). (b) Strip of benign glandular cells exhibiting eccentric nuclei with retained nuclear polarity (ThinPrep, Papanicolaou stain, ×600). (c) Sheet of glandular epithelium with scant to moderate amount of cytoplasm and round to oval nuclei (ThinPrep, Papanicolaou stain, ×400). (d) Group of cells with granular cytoplasm, fine chromatin, and inconspicuous nucleoli (ThinPrep, Papanicolaou stain, ×600)
WHAT IS YOUR INTERPRETATION?
-
Cystitis cystica et glandularis
-
Endometriosis involving the bladder
-
Urachal remnant
-
Adenocarcinoma.
ANSWER
The correct cytopathologic interpretation is:
C. Urachal remnant
The urachus is a remnant of the allantois, a connection between the fetal bladder and the umbilical cord. There are different types of urachal remnants, which can be classified pathologically and radiologically as a communicating sinus between bladder and umbilicus, bladder dome diverticulum, or urachal cyst.[12] In this case transvaginal ultrasound and magnetic resonance imaging (MRI) revealed features shown in Figure 2.
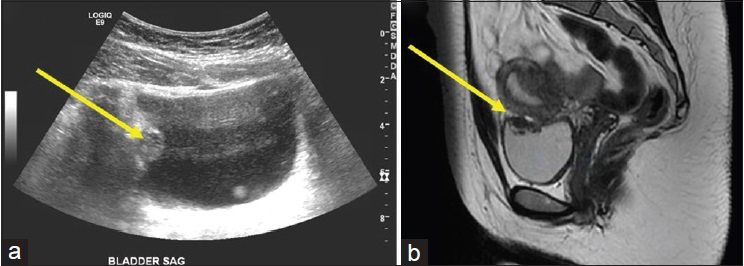
- (a) Transvaginal ultrasound showing a 1.4 cm, right superior urinary bladder wall lesion (arrow). (b) MRI showing a 2.6 cm irregular, solid and cystic lesion in the superior wall of the bladder (arrow)
The persistence of the urachus may be an underreported entity and overall, urachal remnants are not a common finding.[2] In infants, a concerning clinical symptom is the presence of umbilical discharge in remnants that communicate to the umbilicus.[3] Because the abdominal ultrasound is often used as a screening test, many urachal remnants are detected early in life in the pediatric population.[4] In one study by Ozbek et al., 99% of children referred for abdominal ultrasound for any abdominal symptoms (other than those of a patent urachal remnant) showed incidental ultrasonic evidence of a urachal remnant.[5] These may also persist asymptomatically into adult years. In a study performed in autopsies of patients >38 years, the persistence of a urachal remnant was present in 32% of bladders.[6] In adult patients, lower abdominal pain or a palpable mass may be present. Furthermore, lower urinary tract symptoms may be seen as a result of infection. As a more extreme complication of this entity, cases of pelvic Actinomyces spp. has been reported subsequent to infected urachal remnant.[7]
Surgical intervention is recommended when a persistent urachus is identified. Through surgical intervention, symptomatic recurrence and complications can be prevented. Traditionally, an open procedure approached through a lower midline laparotomy or semicircular infraumbilical incision was employed. However, laparoscopic approaches to resection offers lower morbidity and mortality, in addition to improved cosmetic benefits.[891011]
Radiologically, if a urachal remnant has an area of calcification, urinary calculus or urothelial carcinoma should be considered in the list of differential diagnoses.[12] Histologically, the urachal remnants are composed of three layers: The innermost epithelial layer that can be urothelial or columnar, middle layer of fibroconnective tissue and the outermost smooth muscle layer that is in continuity with the surrounding detrusor muscle.
To the best of our knowledge, cytological features of the urachal remnants presented in the urine specimen have not been reported in English literature. In our case, the voided urine was moderately cellular with the absence of blood and inflammation in the background. Sheets of cells were present that were comprised of varying numbers of bland appearing glandular cells with scant to moderate amount of cytoplasm and round to oval nuclei. The nuclei had smooth contours with slightly stippled fine chromatin and inconspicuous nucleoli. Neither mitotic figures nor apoptotic bodies were identified. Also present were small strips and clusters of similar appearing glandular cells exhibiting eccentric nuclei with nuclear polarity. Groups of cells with granular cytoplasm were also seen [Figure 1]. The final cytopathologic interpretation was: “Abundant sheets and clusters of bland glandular epithelium”.
ADDITIONAL QUIZ QUESTIONS
-
In the fetus, the urachus is a remnant of the connection between the:
-
Median umbilical ligament and allantois
-
Allantois and yolk sac
-
Fetal bladder and the umbilical cord
-
Umbilical cord and yolk sac
-
None of the above.
-
-
The epithelium of the inner urachal layer is:
-
Urothelial
-
Columnar
-
Squamous
-
A and B
-
B and C.
-
-
Cytological features of urachal remnants in urine cytology include:
-
Sheets of cells comprised of bland glandular cells
-
Strips and clusters of bland glandular cells with polarized, eccentric nuclei
-
Smooth nuclear contours with stippled chromatin and inconspicuous nucleoli
-
Glandular cells with granular cytoplasm
-
All of the above.
-
Answers to additional quiz questions
1. C; 2. D; 3. E
-
During fetal development, the fetal bladder and the umbilical cord is connected by the allantois. During development, the bladder descends and the urachal lumen constricts to form the median umbilical ligament. The urachus may persist as a remnant if this process is incomplete
-
Pathological examination is necessary for a diagnosis of the urachal remnant. As described histologically, the urachal remnant has an inner epithelial layer, middle fibroconnective tissue layer, and the outer smooth muscle layer. The lining can be urothelial or columnar epithelium
-
Cytological features of urachal remnants include sheets, strips, and clusters of bland appearing glandular cells. These cells have scant to moderate amount of cytoplasm and round to oval nuclei. The nuclear features are also benign appearing with smooth contours, slightly stippled fine chromatin, and inconspicuous nucleoli. Because this is a benign entity, mitotic figures, and apoptotic bodies should not be present.
BRIEF REVIEW OF THE TOPIC
The patient underwent a transurethral resection of the posterior superior bladder wall lesion. The histological examination showed a cystic lesion that involved the bladder lamina propria and muscularis propria. The cyst was lined by stratified cuboidal epithelium without significant cytological atypia or mitoses. The underlying stroma was congested. Also seen were ductal structures lined by cuboidal epithelium sorrounded by muscular walls that were in continuity with the detrusor muscle, consistent with a urachal remnant [Figure 3].
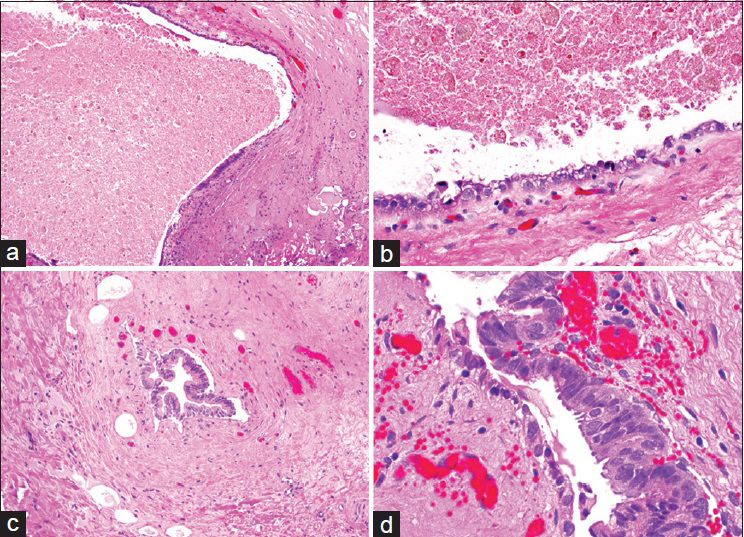
- Histology from the transurethral resection of the posterior superior bladder wall lesion. (a) Cyst involving bladder lamina propria and muscularis propria (H and E, ×100). (b) Cyst lining composed of stratified cuboidal epithelium (H and E, ×400). (c) Ductal structure with a muscular wall in continuity with the detrusor muscle (H and E, ×200). (d) Duct lining composed of cuboidal epithelium (H and E, ×600)
Urachal remnants overall are not a common fining in urine cytology. Whereas the radiological and pathological differential diagnosis is broad attention to cytological details can provide a definitive diagnosis.
Cytomorphological features of urachal remnants that can be seen in liquid-based preparation of urine specimens include the following:
-
Sheets or clusters comprised of varying numbers of bland appearing cells with scant to moderate amounts of cytoplasm
-
Strips of columnar cells with eccentric, polarized nuclei
-
Benign appearing nuclei with smooth nuclear contours, finely stippled chromatin, and inconspicuous nucleoli.
Overall, cytological features of urachal remnants in urine cytology may mimic many benign and malignant conditions involving the bladder. High index of suspicion, bland cytology of the glandular epithelial fragments, and clinical-radiological correlation will be helpful in distinguishing this entity from malignant processes and arriving at the correct diagnosis.
Surgical intervention is recommended when a persistent urachus is identified to avoid symptomatic recurrence and complications. Whereas an open procedure has been classically described, laparoscopic approaches to resection offers lower morbidity and mortality.
Focused differential diagnosis of urachal remnants
Cystitis cystica/glandularis
-
Can mimic a mucinous cystic tumor or bladder tumor radiologically[13]
-
Cytomorphological identification relies on the presence of cuboidal or columnar mucin-secreting cells which can also be of intestinal-type[14]
-
Significant atypia and mitoses are only rarely found which also differentiates them from adenocarcinoma[15]
-
Epithelium identified is usually distinguishable from the transitional epithelium seen with urachal remnants. However, both entities may cytologically appear similar if the urachal remnant is lined by columnar epithelium.
Endometriosis involving the urinary tract
-
Not a common entity, occurring in approximately 1% of all patients with endometriosis
-
Most frequent site of occurrence in the dome of the bladder[16]
-
Cytomorphological analysis of urine will often show hemosiderin laden macrophages or the presence of endometrial cells
-
Endometrial cells are identified as honeycombing sheets or as spherules with clusters of stromal cells surrounded by epithelial cells[17]
-
Usually, no nuclear atypia is observed and nucleoli are inconspicuous.
Müllerianosis of the urinary bladder
Nephrogenic metaplasia/adenoma
-
Often the diagnosis is preceded by a history of instrumentation or chronic inflammatory insult[20]
-
In liquid-based preparations of urine specimens, variably sized cell clusters and papillary structures are evident
-
Cytomorphological analysis shows atypical cuboidal cells with a moderate amount of cytoplasm. The nuclei may be round to slightly irregular with granular chromatin and small nucleoli
-
Cytoplasmic vacuoles can be present which may give the cells a signet-ring appearance.[2122]
Adenocarcinoma of the bladder (including primary bladder adenocarcinoma, urachal adenocarcinoma, and metastatic carcinoma)
Adenocarcinoma of the bladder
-
Adenocarcinomas of the bladder or urothelial carcinomas with glandular differentiation are rare in young patients, as are metastatic adenocarcinomas. Histologically, the majority of bladder adenocarcinoma is comprised of glandular structures showing features of colonic adenocarcinoma (enteric type), intracellular mucin (signet cell type), or extracellular mucin (mucinous type)
-
Cytomorphological analysis of urine cytology will show glandular cells with cytological atypia and frequent mitoses
-
In half of the cases of urothelial carcinoma with glandular differentiation, a second population of malignant cells with morphology consistent with high-grade urothelial carcinoma will be present
-
Adenocarcinomas (as well as rarer types of carcinomas) have been described as arising in urachal remnants.[23] In these cases, cytological features of adenocarcinomas arising in urachal remnants are similar to the other primary and secondary adenocarcinomas that can be encountered in the bladder.[24]
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author.
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
ETHICS STATEMENT BY ALL AUTHORS
As this is a quiz case without identifiers, our institution does not require approval from Institutional Review Board (IRB) (or its equivalent).
LIST OF ABBREVIATIONS
MRI - Magnetic Resonance Imaging
IRB - Institutional Review Board.
REFERENCES
- Clinical presentation and urachal remnant pathology: Implications for treatment. J Urol. 2009;182(4 Suppl):1921-4.
- [Google Scholar]
- The urachal pathology with umbilical manifestation: Overview of laparoscopic technique. J Laparoendosc Adv Surg Tech A. 2011;21:809-14.
- [Google Scholar]
- Current diagnosis and management of urachal remnants. J Pediatr Surg. 2013;48:2148-52.
- [Google Scholar]
- Urachal remnants in asymptomatic children: Gray-scale and color Doppler sonographic findings. J Clin Ultrasound. 2001;29:218-22.
- [Google Scholar]
- Laparoscopic management of symptomatic urachal remnants in adulthood. Asian J Surg. 2015;38:85-90.
- [Google Scholar]
- Laparoscopic management of patent urachus in an adult man. Urol Int. 2007;79:184-6.
- [Google Scholar]
- Don’t get caught out! A rare case of a calcified urachal remnant mimicking a bladder calculus. J Radiol Case Rep. 2013;7:34-8.
- [Google Scholar]
- Low-grade mucinous cystic tumor mimicking urinary bladder tumor: Imaging-pathologic correlation. Urology. 2013;81:e33-4.
- [Google Scholar]
- Morphological evaluation of cystitis glandularis. Indian J Pathol Microbiol. 2009;52:203-5.
- [Google Scholar]
- Endometriosis of the urinary tract in women of reproductive age. Int J Urol. 2006;13:902-4.
- [Google Scholar]
- Mullerianosis of the urinary bladder: Report of a case with diagnosis suggested in urine cytology and review of literature. Diagn Cytopathol. 2012;40:997-1001.
- [Google Scholar]
- Müllerianosis of the urinary bladder: A rare tumorlike lesion. Arch Pathol Lab Med. 2014;138:432-6.
- [Google Scholar]
- Nonneoplastic lesions of the prostate and bladder. Arch Pathol Lab Med. 2012;136:721-34.
- [Google Scholar]
- Urachal carcinomas of the nonglandular type: Salient features and considerations in pathologic diagnosis. Am J Surg Pathol. 2012;36:432-42.
- [Google Scholar]
- Carcinoma of urachus: Report of 3 cases and review of literature. Hinyokika Kiyo. 1984;30:1255-61.
- [Google Scholar]







