Translate this page into:
Fine-needle aspiration of a right neck mass in a 10-year-old boy: Diagnostic clues and workup for tumors with small round blue cells
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Enlarging right neck mass in 10-year-old boy since 1 month with 5-pound weight loss, new onset cough, and change in voice. Examination of the oral cavity showed 8 cm × 8 cm oropharyngeal mass involving the entire right tonsillar region crossing the midline with deviation of the uvula. Computed tomography studies showed involvement of the parapharyngeal space from skull base to the omohyoid area with encasing of carotid artery. Fine-needle aspiration (FNA) [Figure 1] revealed highly cellular smears composed of small round blue cells with oval nuclei showing mild to marked anisonucleosis, lobulated to irregular nuclear contours, and intense hyperchromasia with occasional bare tumor nuclei and mitotic figures. Occasional loosely cohesive clusters and possible rosette formation were seen. Tumor karyotype was highly abnormal, complex, hyperdiploid with several structural and numerical aberrations, including gains of chromosomes 5, 8, 12 and 13. Fluorescence in situ hybridization (FISH) showed extra copy of the 13q14/FOXO1-specific signal in 85.7% of interphase nuclei (gain of chromosome 13q) without 13q14 (FOXO1) rearrangement.
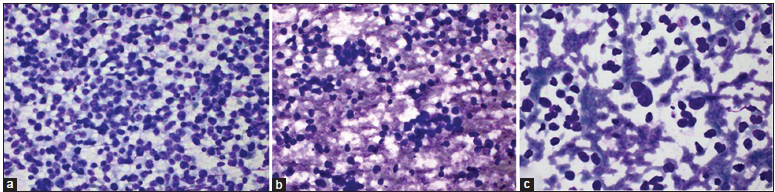
- (a) The aspirate showed a dyshesive population of small blue tumor cells (Diff-Quik, ×400). (b) Occasional cohesive nests and possible rosette formation were seen (Diff-Quik, ×400). (c) Cells with scant delicate cytoplasm had increased nuclear-cytoplasmic ratios and irregular nuclear contours with tendency for bare nuclei in the background without lymphoglandular bodies. (Diff-Quik, ×600)
QUESTION
Q1. What is your interpretation?
-
Rhabdomyosarcoma (RMS), embryonal type
-
Neuroblastoma
-
Acute lymphoblastic lymphoma (ALL)
-
Ewing sarcoma/primitive neuroectodermal tumor (PNET).
ANSWER
Q1. (a) RMS, embryonal type.
Based on the combination of cytomorphology, surgical biopsy with immunohistochemical staining, cytogenetic findings, and FISH analysis, final diagnosis was embryonal RMS.
FOLLOW-UP OF THE PRESENT CASE
A concurrent surgical biopsy contained sheets of malignant small round blue tumor cells. The tumor cells had hyperchromatic nuclei with mild to moderate pleomorphism and scant amounts of clear to eosinophilic cytoplasm. Mitoses were easily identified. The tumor cells showed some nesting with surrounding thin fibrous borders, but no alveolar pattern was appreciated [Figure 2].
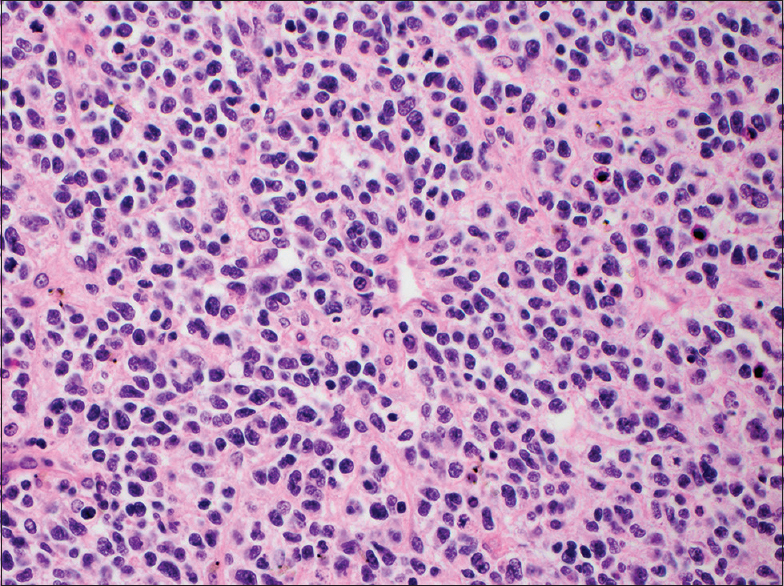
- The concurrent surgical biopsy showed similar-appearing cells with hyperchromatic nuclei and scant pale cytoplasm, arranged in small nests (H and E, ×400)
Immunohistochemical studies were performed on the biopsy. Myogenin and desmin were positive in scattered cells. CD56 was weakly positive [Figure 3]. Vimentin was positive. The Ki-67 showed a markedly elevated proliferation index. FLI-1 showed equivocal staining with high background staining. CD45, CD43, CD34, and multiple other hematologic markers were negative. Chromogranin, synaptophysin, NSE, CD99, EMA, keratin AE1/AE3, and ALK were negative.
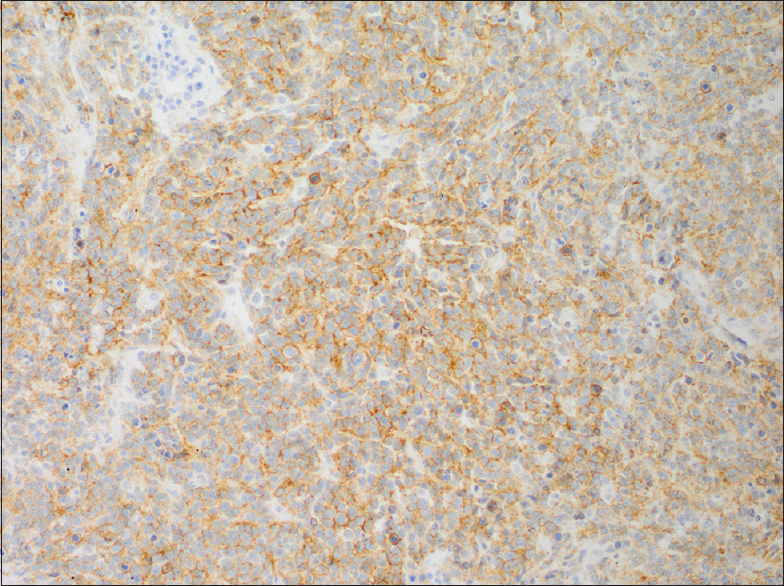
- Immunohistochemical staining for CD56 was weakly positive. Other neuroendocrine markers were negative
FISH analysis showed an extra copy of the 13q14/FOXO1-specific signal in 85.7% of interphase nuclei, indicating a gain of chromosome 13q. Gains of chromosome 13 are a commonly reported finding in embryonal type RMS. Importantly, there was no evidence of the 13q14 (FOXO1) rearrangement seen in alveolar type RMS. The patient received radiation therapy and chemotherapy. At last checkup, he was healthy and without evidence of disease at 41 months after diagnosis.
ADDITIONAL QUESTIONS
Q2. Which is NOT a common diagnosis in the differential diagnosis for a small round blue cell tumor in a child?
-
Lymphoma
-
Ewing sarcoma
-
Rhabdomyosarcoma
-
Squamous cell carcinoma
Q3. Which is the most common subtype of rhabdomyosarcoma in children?
-
Alveolar
-
Embyronal
-
Pleomorphic
-
Spindle cell/sclerosing
ANSWERS TO ADDITIONAL QUIZ QUESTIONS
Q2: D; Q3: B.
BRIEF REVIEW OF THIS TOPIC
The family of small round blue cell tumors (SRBCT) encompasses a broad spectrum of neoplasms with similar cytomorphologic features. These tumors are characterized by generally uniform small to medium-sized, round, and relatively undifferentiated cells with hyperchromatic nuclei and a high nuclear to cytoplasmic ratio. FNA of SRBCTs typically leads to highly cellular smears with abundant material for evaluation.
An initial branch point we used in the workup of this case was the age of the patient. In children, the differential diagnosis includes precursor lymphoid neoplasms (e.g., ALLs), neuroblastoma, Ewing sarcoma/PNET, and RMS.[1]
ALLs can have variable morphology, consisting of dyshesive small cells with high nuclear-cytoplasmic ratios, darkly staining chromatin, and inconspicuous nucleoli to more pleomorphic blasts with lower nuclear-cytoplasmic ratios, irregular to convoluted nuclear contours, finely dispersed chromatin, and more prominent nucleoli.[2] The mitotic rate is high. Their immunophenotype may be B- or T-cell, and the lymphoma entity frequently presents with bone marrow leukemic involvement as well. Although both B- and T-lymphoblastic lymphomas can have nodal and extranodal lesions, T-ALLs present frequently with mediastinal (thymic) involvement. Flow cytometric analysis, chromosomal analysis, targeted FISH studies, and molecular studies are essential for proper diagnostic characterization, treatment plans, and clinical management. On cytology, singly dispersed pattern and the presence of cytoplasmic fragments (i.e. lymphoglandular bodies) in the background help distinguish the tumor from other non lymphoid tumors.
Neuroblastomas represent one end of a spectrum of neoplasms that exhibit variable degrees of maturation up to, and including, mature ganglion cells. Depending on the percentage of neuroblasts and mature ganglion cells, these neoplasms are then termed ganglioneuroblastoma or ganglioneuromas. Neuroblastomas have small round nuclei with “salt-and-pepper” chromatin, small nucleoli, nuclear molding and crowding, and scant pale cytoplasm. Ninety percent of these tumors occur in children younger than 8 years. The adrenal glands and paravertebral sympathetic ganglia are most commonly involved but the neck can be a primary or metastatic site of involvement.[3]
Ewing sarcoma/PNET is the most common bone/soft tissue sarcoma in children. Extraskeletal Ewing sarcoma can arise in the paraspinal area, and up to 25% of patients have metastases at the time of diagnosis. The conventional appearance is that of small- to medium-sized round cells that is densely packed and show nuclear molding. The cells are monomorphous, with dark granular chromatin, inconspicuous nucleoli, and scant delicate cytoplasm. Mitotic activity is high and necrosis is common. Unfortunately, Homer Wright rosettes (seen in histologic sections) are uncommon and particularly difficult to preserve in FNA samples. EWSR1-FLI1 or EWSR1-ERG fusions or EWSR1 rearrangements are characteristic of these tumors.[3]
RMSs are divided into embryonal, alveolar, pleomorphic, and spindle cell/sclerosing subgroups. The embryonal subtype is the most common in children, comprising 60% of RMS cases. Further, the head and neck region are the most common site for RMSs in children. These tumor cells are round or spindled, with high nuclear-cytoplasmic ratios, dark chromatin, and dense eosinophilic cytoplasm. Rarely, cross-striations can be appreciated on histologic sections.[3] Gains of chromosomes 2q, 8, and 20 have been reported in embryonal RMS. Rarely, as was seen in this case, gains of chromosome 13q can be detected by a FOXO1-specific FISH probe in embryonal RMS. The alveolar subtype of RMS is less common, and is composed of larger round cells with even chromatin and prominent nucleoli. Scattered giant cells are admixed with smaller cells. It is the specific rearrangement of 13q14 FOXO1 as either t(2;13)(q35;q14) PAX3/FOXO1 or t(1;13)(p36;q14) PAX7/FOXO1 that is detected by FISH in embryonal RMS.[4] In both subtypes, the RMS cells are arranged in nests with fibrous septae or in flat sheets.
The presence of enlarged pleomorphic or strap-shaped cells with myogenic cytoplasm is helpful in prompting the pathologist to consider RMS in the differential. However, cytomorphology and immunohistochemistry are usually insufficient to further distinguish between the subtypes of RMS. Because treatment and prognosis can vary based on the subtype, it is important for pathologists and cytotechnologists to recognize the need to collect aspirate material for molecular testing and cytogenetic studies at the time of FNA.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
For all authors, the authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
SC carried out literature review, coordinated submission, and drafted and edited the manuscript.
SH collected clinical cases, performed additional literature review, and edited the manuscript.
DYL collected clinical cases and edited the manuscript.
RCM photomicrographs and drafted the manuscript.
MVL collected cases, and helped draft and edit the manuscript.
NAM conceived of the quiz case, collected clinical cases, performed additional literature review, and edited the manuscript.
All authors read and approved the final manuscript.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from Institutional Review Board (IRB) (or its equivalent).
LIST OF ABBREVIATIONS (In alphabetic order)
ALL - Acute lymphoblastic lymphoma
FISH - Fluorescence in situ hybridization
FNA – Fine-needle aspiration
PNET - Primitive neuroectodermal tumor
RMS – Rhabdomyosarcoma
SRBCT - Small round blue cell tumor.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted through automatic online system.
REFERENCES
- Goldblum JR, Weiss SW, Folpe AL, eds. Approach to the diagnosis of soft tissue tumors. In: Enzinger and Weiss‘s Soft Tissue Tumors (5th ed). New York: Elsevier; 2013.
- Lymph node. In: DeMay RM, ed. Practical Principals of Cytology. Chicago: American Society of Clinical Pathologists; 1999.
- [Google Scholar]
- Pediatric spindle cell tumors. In: Hornick JL, ed. Practical Soft Tissue Pathology (1st ed). New York: Elsevier; 2013.
- [Google Scholar]
- Sinonasal small round blue cell tumors: An approach to diagnosis. Semin Diagn Pathol. 2016;33:91-103.
- [Google Scholar]







