Translate this page into:
An uncommon vascular lesion over the right hand

*Corresponding author: Jitendra Singh Nigam, Department of Pathology and Lab Medicine, All India Institute of Medical Sciences, Bibinagar, Telangana, India. nigamjs@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pradeep I, Sharma A, Nigam JS. An uncommon vascular lesion over the right hand. CytoJournal 2023;20:41.
A 45-year female presented with progressively enlarging, 2 × 1 cm, soft, mobile, non-tender swelling over the dorsum of the right hand around the wrist joint for 6 months. Fine needle aspiration cytology are shown in Figure 1.
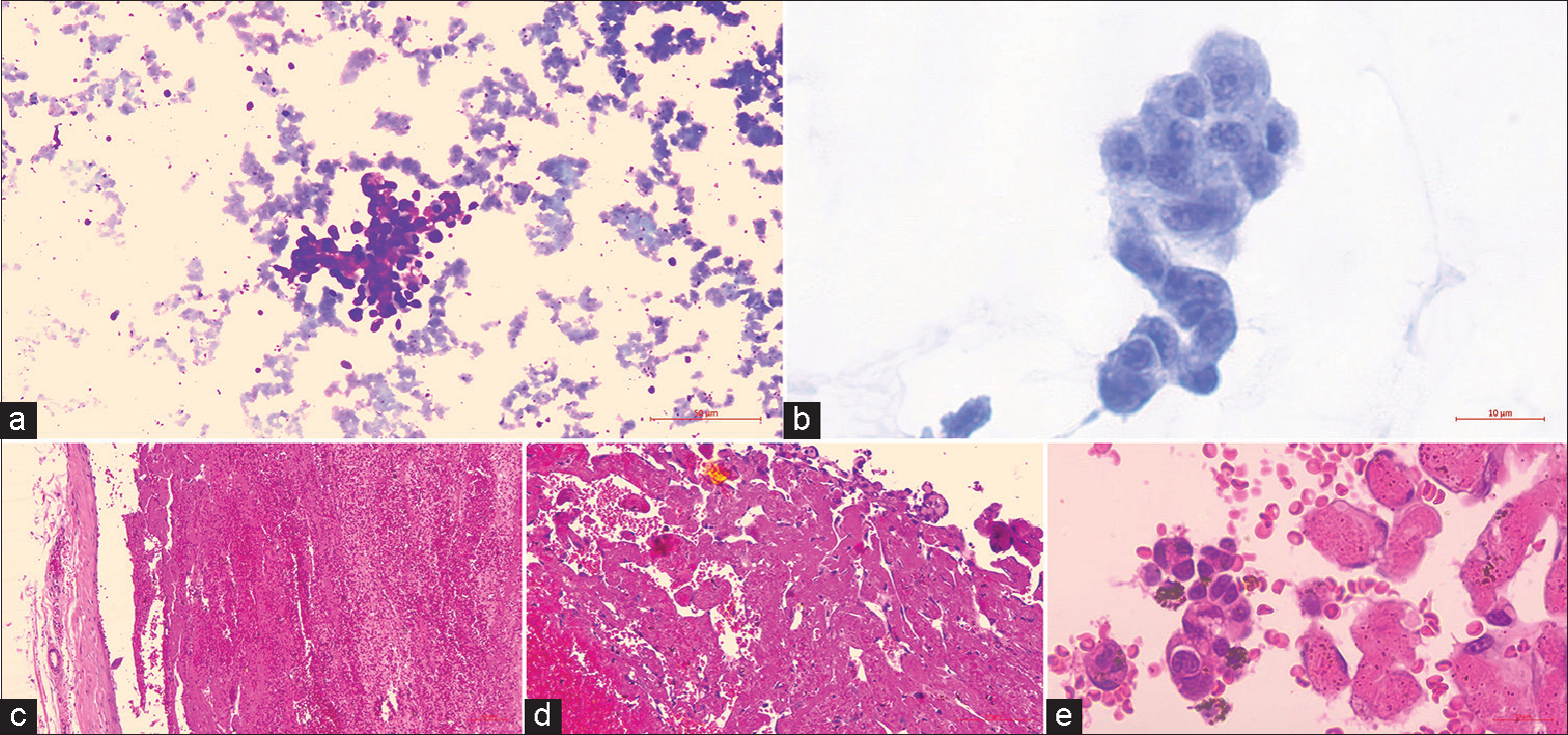
- (a) Isolated cell clusters with plump nuclei displaying “hobnailing” (May Grunwald-Giemsa stain ×100). (b) There is moderate pleomorphism with distinct nucleoli (Papanicolaou stain ×400). (c) A venous wall with intravascular organized thrombus (Hematoxylin and Eosin stain ×400). (d) Thrombus invaginated by anastomosing delicate papillae with a hyalinized core lined by endothelial cells (Hematoxylin and Eosin stained cell-block section ×100). (e) Plump endothelial cells with hobnail nuclei (Hematoxylin and Eosin stained cell-block section ×400).
Q1. What is your interpretation?
Hemangioma
Angiosarcoma
Papillary endothelial hyperplasia (PEH)
Hobnail hemangioendothelioma.
Answer: c. Papillary endothelial hyperplasia (PEH)
Common sites of involvement by PEH include the head-and-neck, lip, tongue, buccal mucosa, and limbs. Usually presents as a reddish-blue nodular lesion in the skin or mucosa.[1] On histology, they present as an intravascular lesion with residual organizing thrombus, anastomosing vascular channels, and papillary formations with hyaline or fibrous stalks lined by plump endothelial cells (histiocyte or epithelial-like).[2-5]
Q2. Which among the following finding is characteristically seen in PEH
Hobnail
Thrombus
Nuclear atypia
Necrosis.
The differential diagnoses considered include vasoformative lesions such as hemangioma, angiosarcoma, and hobnail hemangioendothelioma. Hemangioma and angiosarcoma commonly involve the skin and subcutis of the head-and-neck region. Angiosarcomas exhibit marked nuclear atypia, necrosis, and mitoses. They are never confined to the intravascular location.[1] Hobnail hemangioendothelioma (retiform type) is a rare intermediate-grade (locally aggressive) tumor of vascular origin affecting distal extremities. It consists of numerous elongated vessels (retiform) involving the dermis and extending into the subcutis. They display “hobnail” endothelial cells similar to PEH.[6] However, they lack the organized thrombus seen in histology sections.[6]
Q3. Which of the following is a reactive, non-neoplastic process.
Arteriovenous malformation
Hereditary hemorrhagic telangiectasia
PEH
Hobnail hemangioma.
Q4. Papillary endothelial hyperplasia is not a common feature of PEH:
Usually begins within a thrombosed blood vessel
They usually have abundant thrombotic material
They show papillae are lined by plump, normochromatic endothelial cells, in a single, non-stratified layer
PEH shows frequent mitotic figures.
Papillary endothelial hyperplasia is a reactive, non-neoplastic lesion representing an exuberant organization and recanalization of the thrombus.[3] It occurs in normal vessels as well as in preexisting vascular lesions such as varices, hemorrhoids, pyogenic granulomas, hematomas, and angiosarcomas. The clinical presentation is non-specific, so histopathological examination is ultimately required to establish the diagnosis.
A BRIEF REVIEW OF THE TOPIC
PEH is an exuberant intravascular, endothelial cell proliferation mimicking a neoplastic tumor of vascular origin with papillary tufting and “hobnail” morphology.[1] Although initially described as a neoplastic lesion by Masson,[7] it is now considered as reactive vascular proliferation with an organized thrombus.[8] In its pure form, as in our case, it occurs in dilated veins of the head, neck, limbs, and trunk. It can also engraft in pre-existing vasoformative lesions. In the early lesions, numerous small, delicate papillae with a hyalinized core lined by plump endothelial cells invaginate into the lumen with tufting growth and “hobnail” morphology as in our case.[2-5] During the late stage, the fusion of the papillae results in an anastomosing network of vessels embedded in a loose, meshlike stroma of connective tissue.[1] Rupture of the vein can result in the passive extension of the lesion into the surrounding soft tissue.[1] The prognosis is generally excellent. Essentially, all cases are treated and cured by simple excision.[1] Recurrent lesions are generally secondarily superimposed on preexisting vasoformative lesions.[1]
SUMMARY
Papillary endothelial hyperplasia carries a significant potential for misdiagnosis as angiosarcoma. Cytopathological diagnosis of this uncommon reactive vascular lesion is difficult only on FNA findings. A vascular lesion may be considered, especially when polygonal cells with plump nuclei and “hobnail” morphology are seen in a hemorrhagic background. The cytological differential diagnoses to be considered include the common neoplastic vascular lesions. Histomorphology of the resected specimen helps provide conclusive evidence in excluding the neoplastic nature of the vascular lesion.
Answers to Q2 through Q4:
Q2:b, Q3: c, Q4: d.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
The authors have no conflicts of interest.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Concept, Design, Data Acquisition, and Literary Search: Dr. Immanuel Pradeep, Dr. Abhimanyu Sharma, and Dr. Jitendra Singh Nigam. Manuscript Preparation: Dr. Immanuel Pradeep and Dr. Jitendra Singh Nigam. Manuscript Editing and Review: Dr. Immanuel Pradeep, Dr. Abhimanyu Sharma, and Dr. Jitendra Singh Nigam.
ETHICS STATEMENT BY ALL AUTHORS
Informed and written consent was obtained from the patient. The case was submitted without identifiers.
LIST OF ABBREVIATIONS (In alphabetic order)
FNA – Fine needle aspiration
PEH - Papillary endothelial hyperplasia
EDITORIAL/PEERREVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (the authors are blinded for reviewers and vice versa) through automatic online system.
References
- Papillary endothelial hyperplasia (vegetant intravascular hemangioendothelioma, intravascular angiomatosis) In: Enzinger and Weiss’s Soft Tissue Tumors. St. Louis: Mosby; 2020. p. :7447.
- [Google Scholar]
- Masson’s vegetant intravascular hemangioendothelioma. Fine needle aspiration cytology, histology and immunohistochemistry of a case. Acta Cytol. 1990;34:1758.
- [Google Scholar]
- Fine needle aspiration cytology of papillary endothelial hyperplasia. A case report. Acta Cytol. 1999;43:6636.
- [CrossRef] [PubMed] [Google Scholar]
- Intravascular papillary endothelial hyperplasia of the neck masquerading as malignancy on fineneedle aspiration cytology. Diagn Cytopathol. 2003;29:147.
- [CrossRef] [PubMed] [Google Scholar]
- Papillary endothelial hyperplasia of the orbit: Report of a case highlighting a pitfall on fine needle aspiration biopsy. Acta Cytol. 2007;51:20710.
- [CrossRef] [PubMed] [Google Scholar]
- Papillary endothelial hyperplasia (vegetant intravascular hemangioendothelioma, intravascular angiomatosis) In: Enzinger and Weiss’s Soft Tissue Tumors. St. Louis: Mosby; 2020. p. :7727.
- [Google Scholar]
- Hemangioendotheliome vegetant intravasculaire. Bull Soc Anat (Paris). 1923;93:517-24.
- [Google Scholar]
- Intravascular papillary endothelial hyperplasia. Arch Pathol Lab Med. 1976;100:441-4.
- [Google Scholar]







