Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
24: An analysis of fine needle aspirations with atypical diagnoses
Leigh Ann Cahill, BS, CT(ASCP)CMIAC, Joseph Bergeron, MD, Adnan Siddiqui, MD, Michael Idowu, MD, Celeste Powers, MD, PhD
Cytopathology / Anatomic Pathology, Virginia Commonwealth University Health System, Richmond, Virginia
Introduction: The development of advanced imaging techniques over the last decade has been paralleled by equally advanced image-guided fine needle aspiration (FNA) techniques. This has created a paradigm shift from a clinic to an intensivist mode. A definitive diagnosis may not always be rendered. The use of the term ‘atypical’ in the interpretation occurs for various reasons including limited material, or absence of distinctive cytomorphology, and / or patient inability to tolerate the procedure. The aim of this study is to review the final FNA diagnoses of superficial FNAs (SFNA) and image-guided FNAs (IGFNA), to determine the factors that precluded a definitive interpretation.
Materials and Methods: A five-year retrospective review of 6880 FNA cases from January 2006 to December 2010 resulted in 123 FNAs with a final diagnosis of ‘atypical’. Only cases with follow-up specimens that resulted in a definitive diagnosis were included in this analysis. Follow-up procedures included surgical biopsies, repeat FNAs and / or non-gynecological specimens. The presence of cell blocks and ancillary testing modalities (immunohistochemistry, flow cytometry) as well as specimen adequacy was noted. The rate of atypical FNA diagnosis was compared with the total FNAs and the rate of atypical diagnosis with a definitive subsequent diagnosis was determined.
Results: From a five-year total of 6880, 123 (1.8%) cases were diagnosed as ‘atypical’. Seventy-one of 123 (57.7%) cases were SFNA and 52 / 123 (42.3%) were IGFNA. Table 1 illustrates the subsequent diagnosis from the follow-up procedure for each FNA type. Sixty-nine of 71 (97.2%) SFNA cases and 45 / 52 (86.5%) IGFNA cases had either non-contributory / inadequate or no cells blocks. Although most atypical diagnoses were made in the absence of a useful cell block, other factors also played a role, including, but not limited to, low cellularity smears, bland cytomorphology, and the need for flow cytometry in suspected hematological cases. Smears with low cellularity in this study resulted from a difficult FNA procedure, and were, not surprisingly, also associated with non-contributory cell blocks and no ancillary testing.
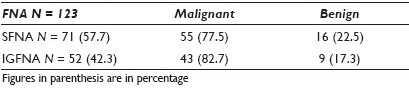
Conclusions: The ‘atypical’ diagnosis is unavoidable as it is most often attributed to low specimen yield. At our institution, only 1.8% of all FNAs had an ‘atypical’ diagnosis and 79.7% of these ultimately proved to be malignant. This suggests that ‘atypical’ diagnoses are rendered very sparingly and most prove to be malignant. For those atypical diagnoses where sampling is adequate, it may be possible to reduce this diagnosis by conducting a peer review of atypical cases before verification, thus reducing or avoiding unnecessary follow-up procedures.








