Translate this page into:
Atypical glandular cells (AGC): Cytology of glandular lesions of the uterine cervix

*Corresponding author: Sudeshna Bandyopadhyay, MD Departments of Pathology, Wayne State University School of Medicine, Detroit Medical Center, and Karmanos Cancer Center, Detroit, Michigan, USA. sbandyop@med.wayne.edu
-
Received: ,
Accepted: ,
How to cite this article: Khan MY, Bandyopadhyay S, Alrajjal A, Choudhury MS, Ali-Fehmi R, Shidham VB. Atypical glandular cells: Cytology of glandular lesions of the uterine cervix. CytoJournal 2022;19:31.
Abstract
The Pap smear is a well-known screening tool for squamous lesions of the uterine cervix. However, its screening role in glandular lesions is less effective. The incidence of squamous cell carcinoma of the cervix has dramatically decreased with the advent of Pap smear and recent understanding related to HPV carcinogenesis of cervical cancers including the advent of HPV vaccines. However, in recent years, the incidence of glandular abnormalities, diagnosed on Pap smears, has increased with greater sensitivity and precision.
The incidence of atypical glandular cells (AGC) is approximately 0.18–0.74% of all cervical smears with a reported prevalence of 2.5% among all Pap smears. A high degree of suspicion, good clinical history, and the presence of diagnostic cytomorphological findings are essential for the proper interpretation of glandular cell abnormalities. A methodical approach to evaluate Pap smear greatly helps interpretation and avoids the diagnostic pitfalls. The Bethesda System for reporting cervical cytology has categorized glandular cell abnormalities into various categories as follows:
Endocervical adenocarcinoma in situ (AIS) Atypical glandular cells (AGCs) Endocervical cells: a1 NOS or specify in comments; a2 Favor neoplastic Endometrial cells: NOS or specify in comments Adenocarcinoma (AdCa) Endocervical Endometrial Extrauterine NOS
Subtle differences in quantitative and qualitative cytologic features are essential for distinguishing one category from another. In this chapter, we highlight an organized approach for the interpretation of glandular abnormalities in Pap smear for our readers. This is an overview of the Bethesda categories, the reason for classification, and differential diagnosis with key characteristic features. An approach to the methodical evaluation of hyperchromatic crowded groups is discussed with key cytomorphologic differences. An algorithmic approach is suggested to facilitate the interpretation of various AGC categories.
Keywords
Atypical glandular cells
AGC
HCG
Hyperchromatic crowded groups
Cervical cytology
HPV
Cancer
Screening
Adenocarcinoma
AIS
Adenocarcinoma in situ
Endocervix
Endometrial
INTRODUCTION
The success story of Pap smears in the dramatic decrease in the prevalence of cervical squamous cell carcinoma is further accelerated with advances in the understanding of Human papillomavirus (HPV) carcinogenesis of cervical cancers along with the efficacy of recently available HPV vaccines.[1] However, the glandular abnormalities reported in Pap smears have increased recently.[2]
Although Pap smears are less sensitive for the evaluation of epithelial cell abnormalities of glandular origin as compared to squamous lesions, they usually fall in the differential diagnoses of high-grade squamous cell lesions (HSILs) [Figure 1] and hyperchromatic crowded groups (HCGs). A high degree of suspicion, good clinical history, and methodical application of diagnostic criteria, especially in an algorithmic manner highlighted in this review would facilitate improved interpretation of cytologic features and facilitate methodical interpretation of glandular cell abnormalities [Figure 2].
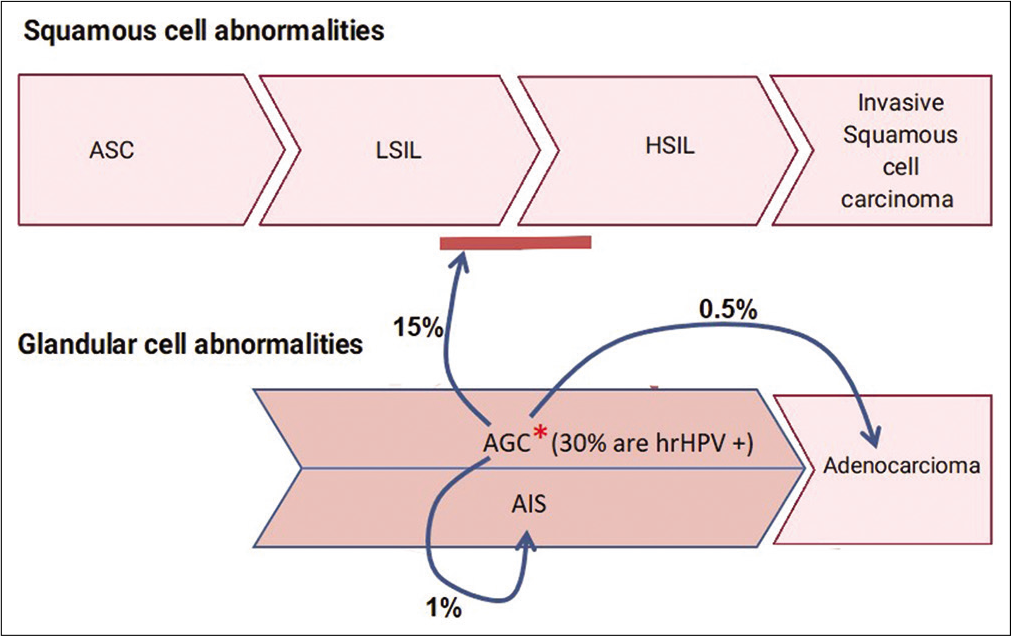
- Cyto-histo correlation of AGC: *Around 30% of AGC are High-risk HPV (hrHPV) positive2a. On cyto-histo correlation about 15% are associated with LSIL or HSIL. 1% are associated AIS and 0.5% with adenocarcinoma2.
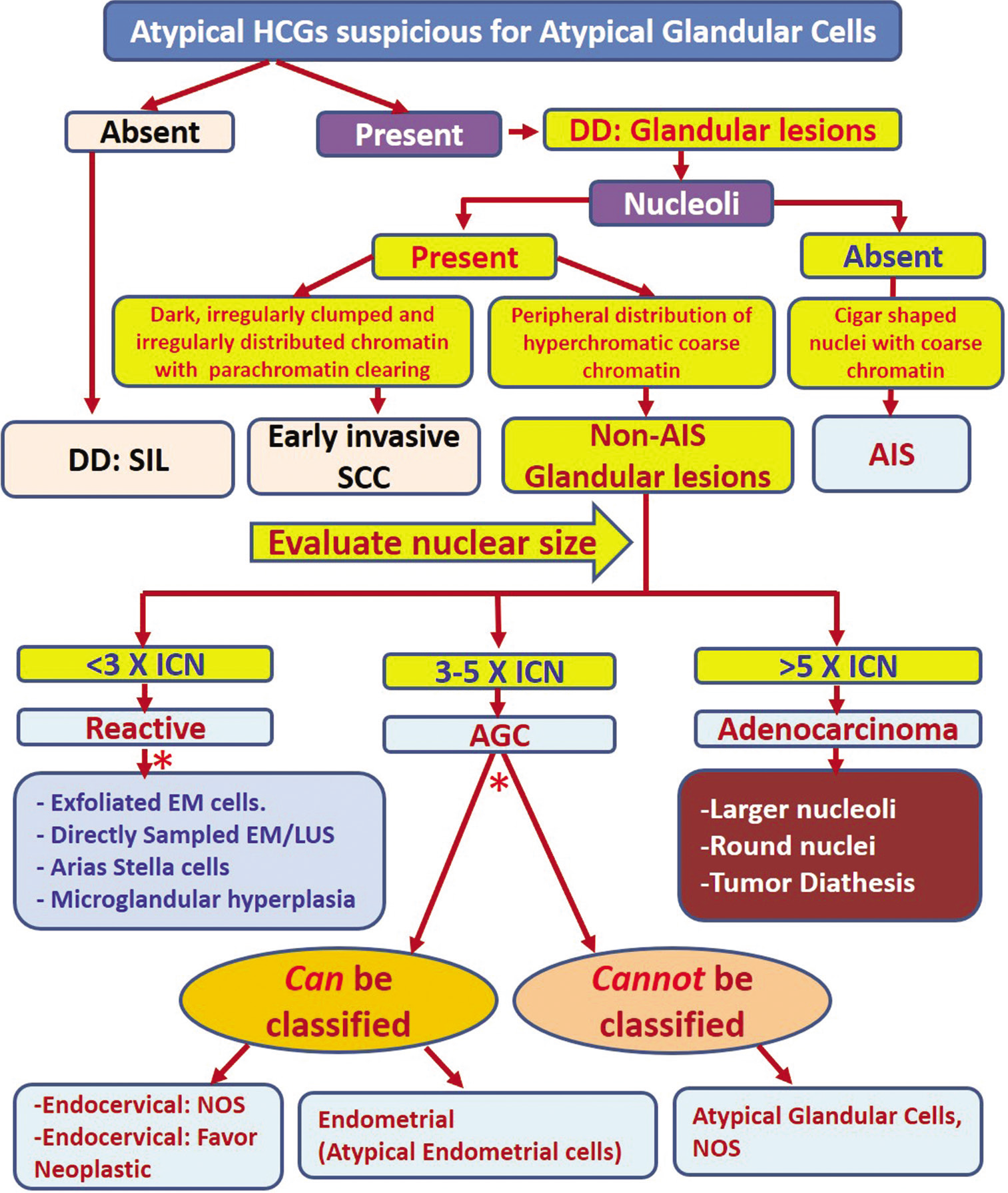
- Algorithmic approach for evaluating atypical HCGs. Apply the features described for specific category. DD: Differential diagnosis, EM: Endometrial cells, HCG: Hyperchromatic crowded group, AIS: Adenocarcinoma in situ, SCC: Squamous cell carcinoma, SIL: Squamous intraepithelial lesion, ICN: Intermediate cell nuclei, AGC: Atypical glandular cell, NOS: Not otherwise specified.
The Bethesda System broadly categorizes glandular cell abnormalities into:
Endocervical adenocarcinoma in situ (AIS)
-
Atypical glandular cells (AGCs)
-
Endocervical cells:
a1 NOS or specify in comments;
a2 Favor neoplastic
Endometrial cells: NOS or specify in comments
-
-
Adenocarcinoma (AdCa)
Endocervical
Endometrial
Extrauterine
NOS
It was observed during the Bethesda Inter-observer Reproducibility Study (BIRST-2) in 2017 that the interpretation of AGC is challenging with lower interobserver reproducibility. The study showed that there was 1 / 3 (33%) concordance for AGC interpretations among participants (cytopathologists) and the Bethesda panel (experts).[3]
Even after many advances in cytological techniques, the interpretation of AGC remains elusive because of associated challenges in distinguishing them from other lesions such as HSIL and other HCGs with some cytomorphological overlaps [Figure 1]. This issue has enhanced significance in the light of recent increase in the incidence of cervical adenocarcinoma in situ (AIS) and invasive adenocarcinoma.[3,4] An algorithmic approach would help in improving the interpretation with precision, for more effective management [Figure 2].
The Society of Gynecologic Oncology recently recommended risk-based management of AIS in 2019 ASCCP consensus guidelines for glandular lesions. The guidelines do not specifically recommend cold knife conization over loop electrocautery excisional procedure (LEEP) but do state that excisional procedures should aim to remove an intact specimen for the evaluation of resection margins.[5] Performance of a LEEP followed by a “top hat” endocervical excision is less acceptable.[6]
The recurrence risk of AIS is only 2.6% with negative margins but increases to 19% with positive margins.[6,7] It is important to highlight that AIS is frequently associated with “skip lesions” with a propensity for non-contiguous multiple foci of AIS. Because of this, the risk of residual AIS on a second excisional specimen is 20% even with negative margins (compared to 53% if margins are positive). About 2% of these patients with negative margins may be associated with invasive cancer as compared to 6% if margins are positive.[8]
Ultimately for AIS, hysterectomy is preferred because it is often located within the endocervical canal and is difficult to recognize on colposcopy. However, fertility-sparing procedures are considered acceptable in select patients.
DIAGNOSTIC ALGORITHM
With aggressive surgical management at stake, the task of the cytopathologist is to accurately report abnormal glandular cells by excluding mimickers mostly HSIL and other HCGs. However, distinguishing these entities may not be straightforward, especially from squamous lesions involving endocervical glands.
The distinction between squamous and glandular lesions can be approached by examining subtle differences in nuclear and cytoplasmic features [Figure 3]. In general, nuclei of glandular cells show discernible nucleoli (except in AIS). The cytomorphological features are best examined at the periphery of the hyperchromatic crowded groups (HGs). The cytoplasm of glandular cells often displays a finely vacuolated or “textured” lacy pattern (in contrast to glassy/waxy relatively homogeneous cytoplasm in squamous epithelial cells). Nuclear size is usually larger than 5 times intermediate cell nuclei (ICN) (except in endometrioid adenocarcinoma) for distinguishing these cells from squamous epithelial lesions with overlapping features [Figure 2].[4]
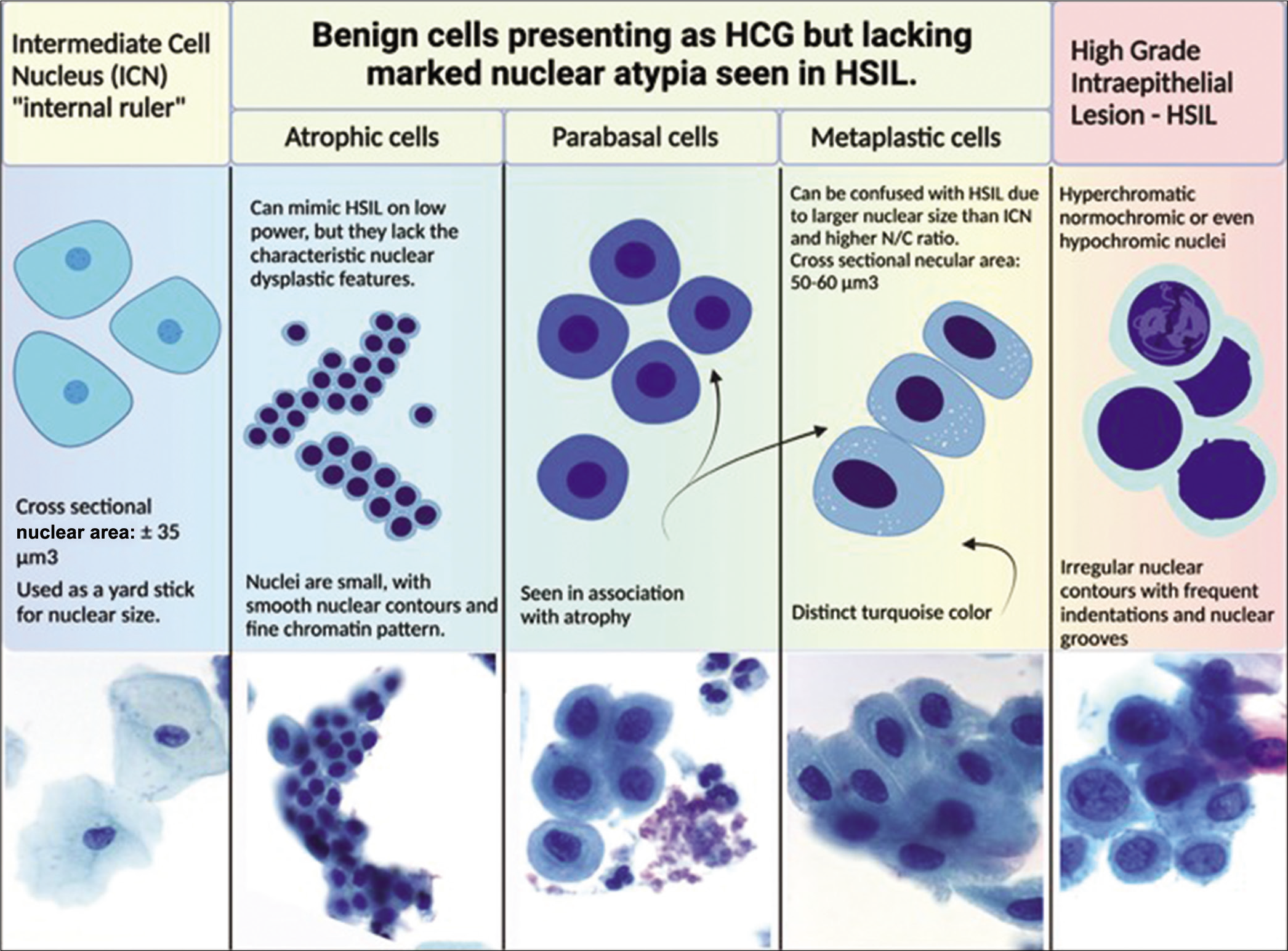
- Various non-neoplastic cellular components seen on Pap smear is preferable compared to AGC. The cell sizes and how they relate to each other are shown in the drawings (relative proportions are maintained). Actual images of superficial, intermediate, parabasal, metaplastic, and HSIL are shown below the drawings. (Reproduced under Open-Access charter from Ref #31).
AIS demonstrates cigar-shaped, enlarged, hyperchromatic nuclei with coarse chromatin without nucleoli. In addition, AIS shows nuclear feathering at the periphery of the groups [Figure 4]. This feature is better seen in conventional direct smears than in liquid-based cytology preparations[3] As many of these features overlap with HSIL, AIS has to be usually distinguished from HSIL with or without endocervical gland involvement (rather than AGC).[9]
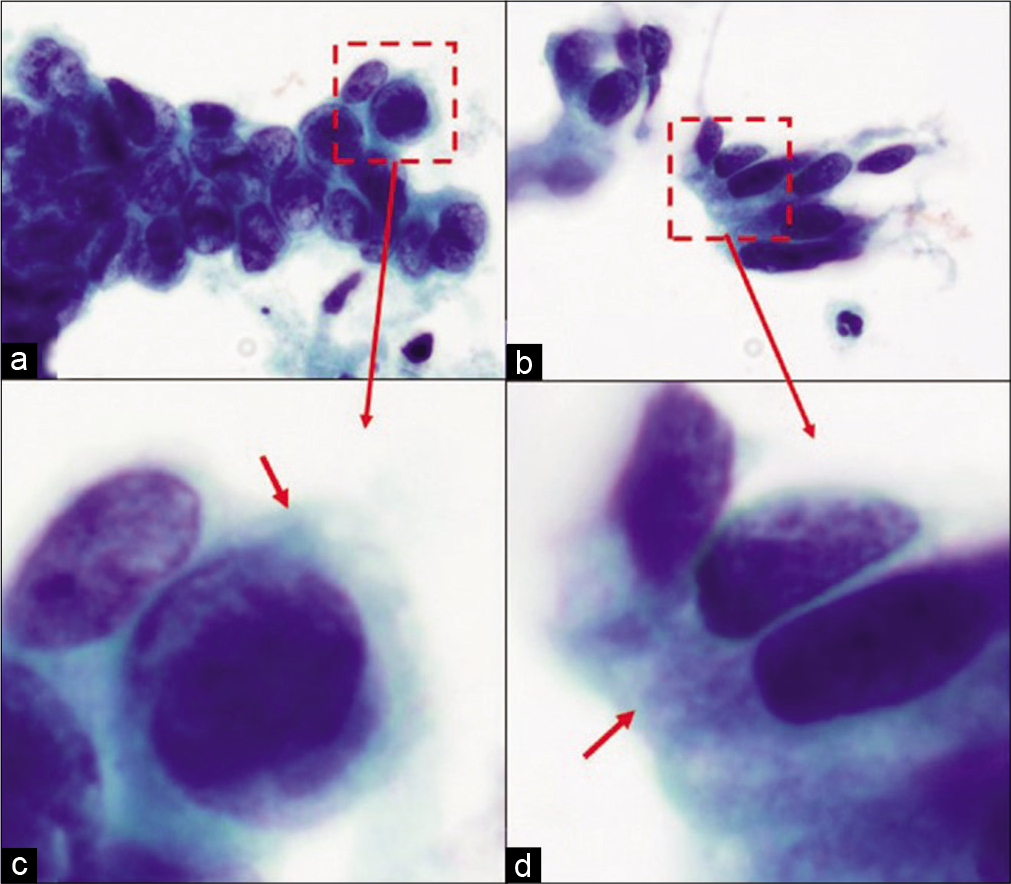
- HSIL versus AIS cytoplasm of HSIL versus AIS cells: (a and c) Groups of HSIL cells: The metaplastic cytoplasm of cells as seen in the cells at the periphery (arrow) is dense and homogeneous. (b and d) Groups of AIS cells: The cytoplasm shows lacy appearance (arrow).
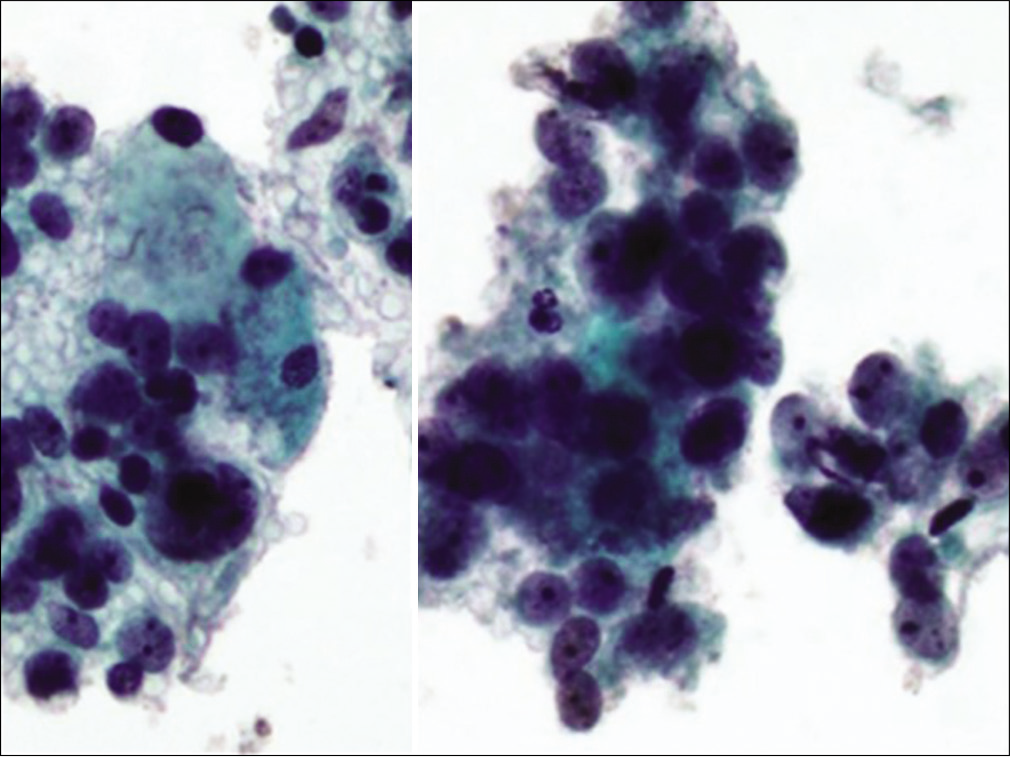
HCGs of atypical endometrial cell groups with nuclei larger than non-neoplastic endometrial cells show a high nuclear-cytoplasmic (N/C) ratios. In contrast to AIS, the nuclei with irregular nuclear outlines show nucleoli [Figure 5].[10]
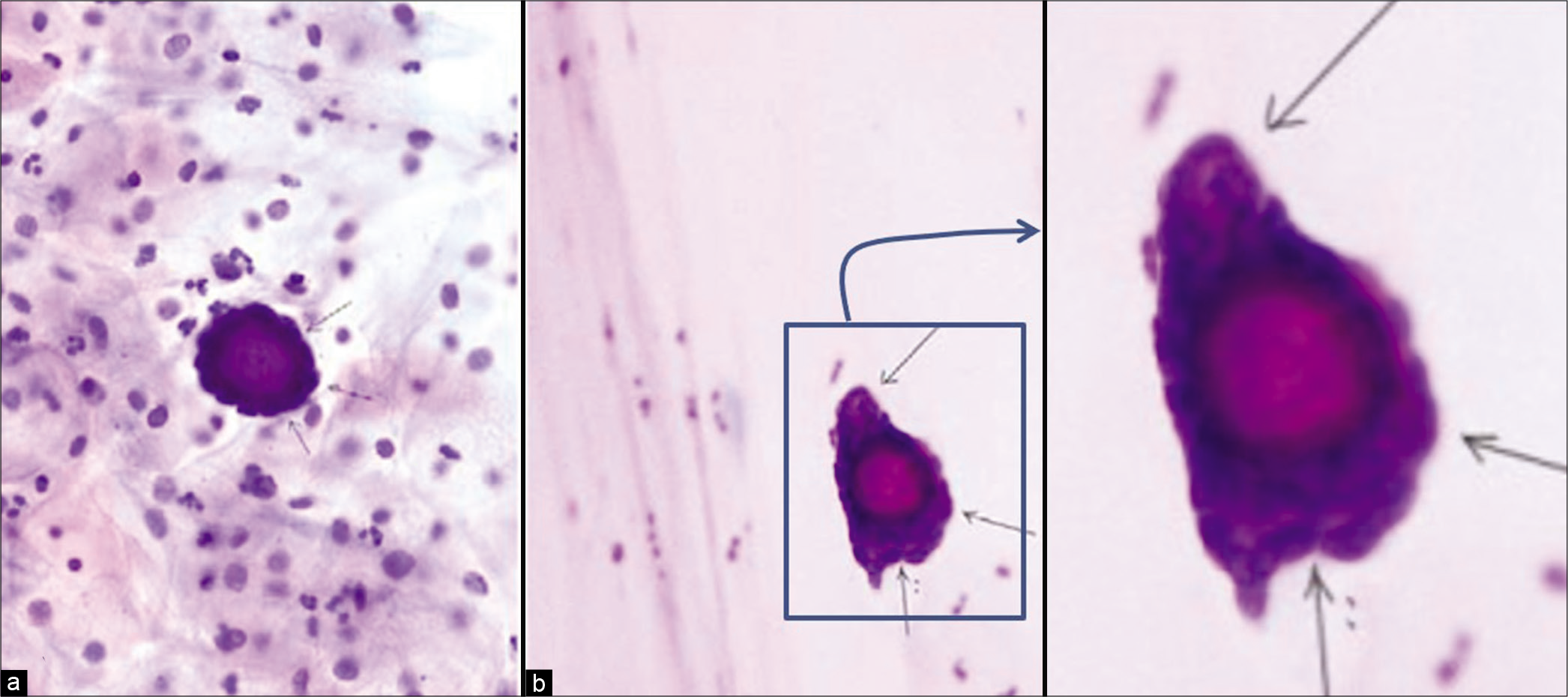
- Adenocarcinoma, other (a) psammoma body surrounded by atypical cells (thin arrows) in cervicovaginal smear (Papanicolaou stain, ×200); (b) psammoma body surrounded by atypical cells (thin arrows) in endometrial aspiration smear (Papanicolaou stain, ×200). Follow-up showed serous carcinoma of the ovary. (Reproduced under Open-Access charter from Ref #32).
For other glandular lesions (other than AIS and endometrial adenocarcinoma), the questionable group with atypical cells can be interpreted as abnormal glandular cells based on size (usually more than 5 times ICN) of hyperchromatic nuclei with detectable nucleoli (chromocenters should not be confused for nucleoli). Larger-hyperchromatic nuclei with nucleoli favor AGC. Often, only the cytomorphological features of atypical cells may not be adequate. AGC is the option if the findings are not sufficient to render a definitive interpretation of adenocarcinoma.
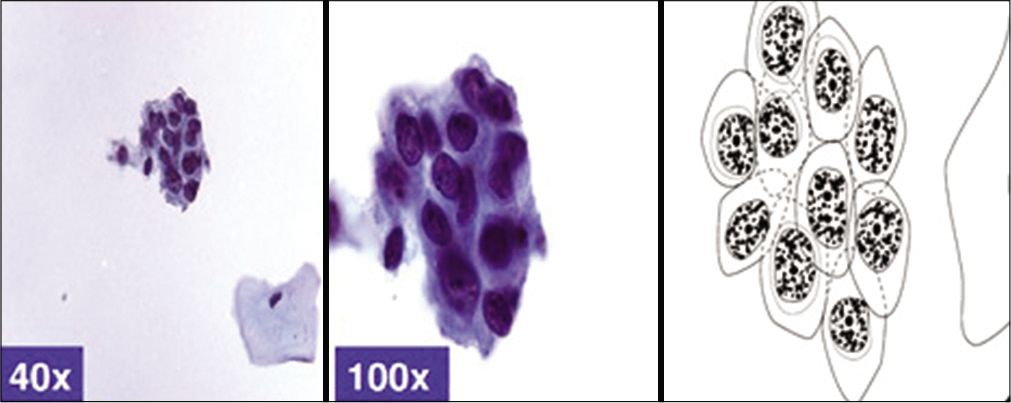
HCGs are the most important differential with glandular lesions and are one of the significant diagnostic challenges in the cytopathology of Pap smears [Figures 6 and 7]. HCG is specifically defined as dark crowded cell groups of usually more than 15 cells identified at ×10 screening magnification. Studies have shown that the vast majority of HCGs are non-neoplastic. However, their presence should warrant more rigorous scrutiny, because HCGs in small proportion of cases may represent higher grade epithelial cell abnormalities including AGC.[10] AGC falls in “high-risk” category because of increased chances of AdCa, AIS, or HSIL (CINII/CINIII) on biopsy after AGC on Pap test. Based on various studies, 9–96% of AGC turn out to be HSIL and the majority have high-risk HPV (hrHPV).[2,3] However, if the nuclear features are interpreted strictly with the evaluation of nuclear details, especially with reference to nucleoli, this disparity should be minimal [Figure 2]. The chromocenters in nuclei of HSIL may be misinterpreted as nucleoli, leading to their misinterpretation as AGC instead of HSIL.
- Hyperchromatic crowded group of small parakeratotic cells showing cohesive groups of hyperchromatic cyanophilic small atypical parakeratotic (SAPK) cells with relatively straight cell borders with angulations better seen at periphery. N/C ratio is higher. Chromatin is smudgy. Some cells may show koilocytic space around nuclei. (Reproduced under Open-Access charter from Ref #10).

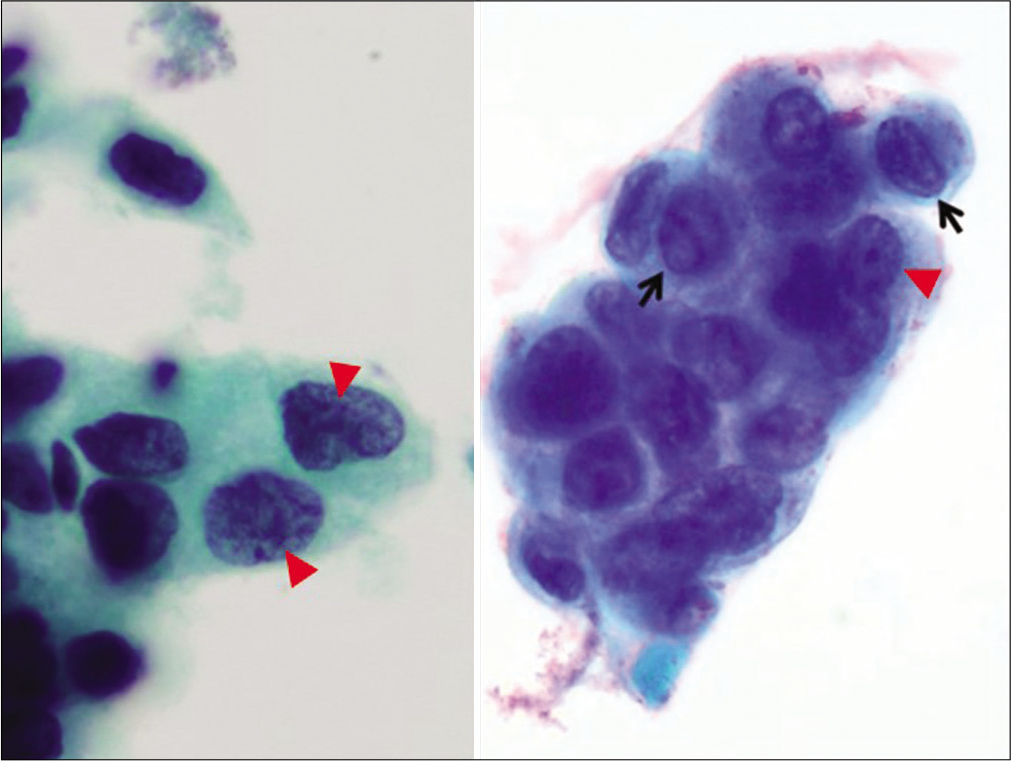
- HSIL with endocervical gland involvement: HSIL cells with endocervical gland involvement seen as (a) hyperchromatic crowded groups (HCG) showing (b) high N/C ratio, hyperchromatic nuclei evenly distributed coarse chromatin and prominent nucleoli at the periphery of HSIL group (arrow in c) as epigenetic feature. The dysplastic cells in the center (arrowhead in c) show features of HSIL without nucleoli.
THE ROLE OF HPV TESTING AND SUBTYPING
Most cervical glandular lesions are associated with 16, 18, and 45 with higher likelihood of HPV positivity in younger women (<40 years, ≠ 90%) compared to older (>60 years, ≠ 40%).[11,12] Other hrHPV types include HPV 31, 33, 35, 39, 51, 52, 56, 58, 59, 66, and 68.
Some adenocarcinoma (AdCa) negative for hrHPV and can be encountered in cervical Pap smears. The HPV-negative AdCa in Pap smears include the majority of endometrial carcinomas, clear cell carcinoma, high-grade serous carcinoma, mesonephric AdCa, and adenocarcinomas of other sites[13]
At present, guidelines about testing for hrHPV in Pap smears with an AGC interpretation are not available. For example, HPV is more likely to be positive in the AGC group with concomitant squamous lesions compared to lower HPV positivity in cases with atypical endometrial cells. Therefore, positive HPV status in AGC group is associated with higher detection rate of clinically significant lesions compared to HPV-negative cases with negative predictive value of 99.2%.
The source of glandular cells in cervical cytology preparations could be from a variety of anatomic sites along the tract from the ovary – fallopian tube – uterus – endocervix tract – to the vagina. However, the most common source of glandular cells is endocervix and/or endometrium. Although the endocervical canal anatomically runs from the external os to the internal os, the endocervical glandular epithelium is not limited by anatomic borders. Rather the transformation zone, (a line that marks the transition from the glandular lining of endocervix to the squamous epithelium of ectocervix), is dynamic and constantly changing depending on multiple factors including age, parity, and hormonal changes, especially during the reproductive years. Because, the cytomorphology of endocervical glandular cells can be diverse, familiarity with these features cannot be overemphasized [Figures 8 and 9].
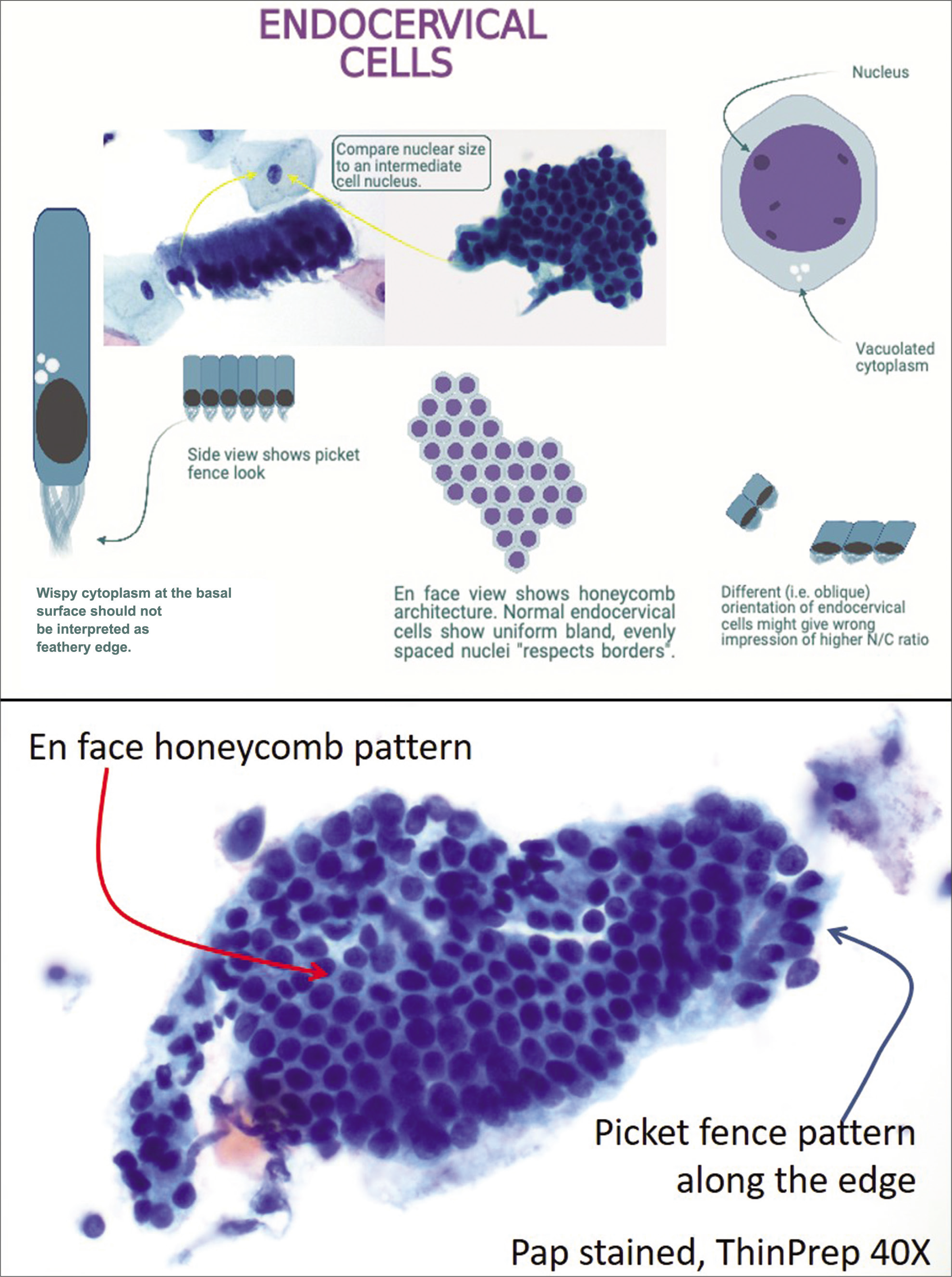
- Cytomorphology of endocervical glandular cells.
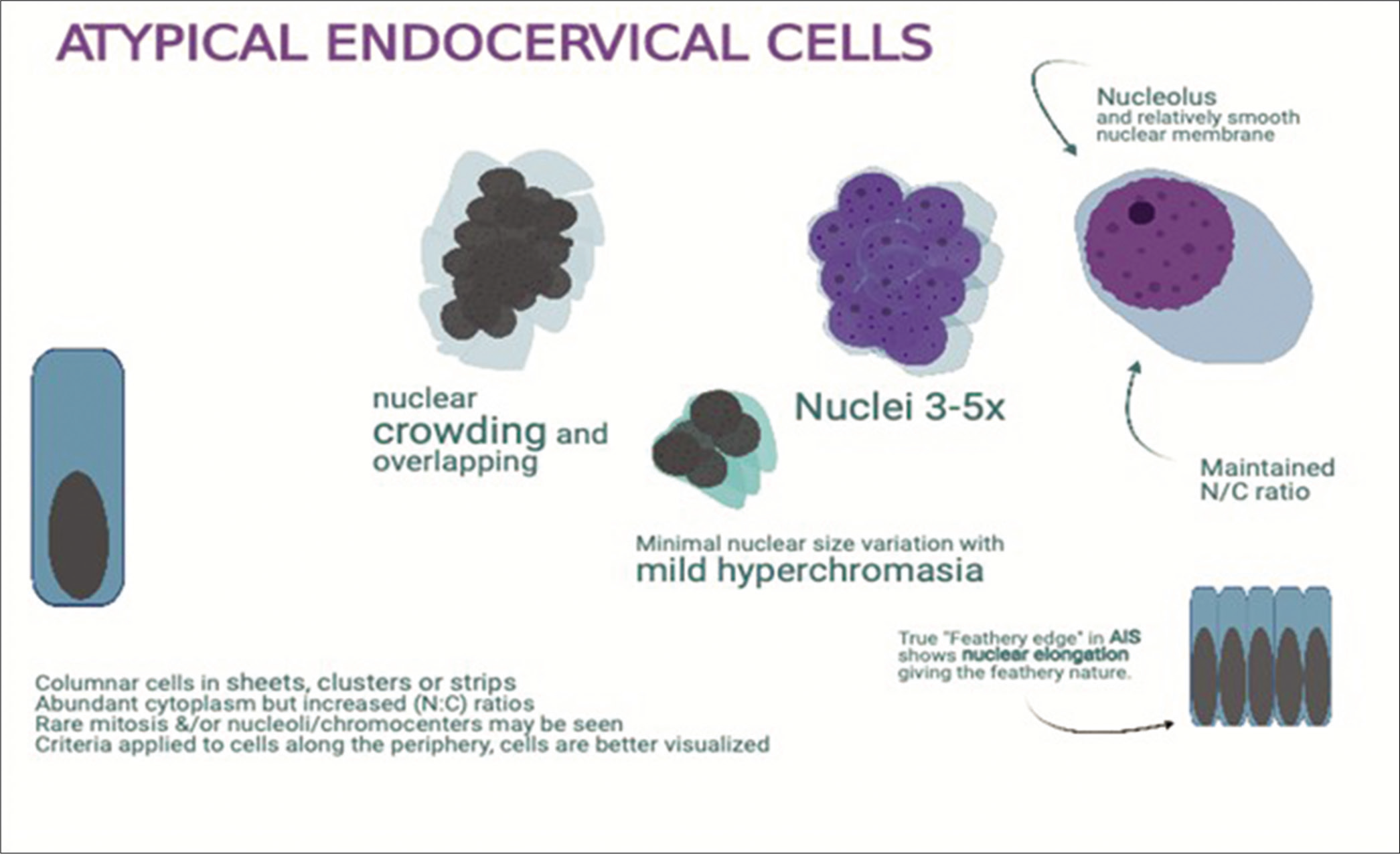
- Atypical endocervical cells: enlarged nuclei (3 to 5X ICN) with prominent nucleoli with minimal architectural disorganization with architectural atypia.
GLANDULAR CELL ABNORMALITIES
Endocervical AIS
The typical endocervical AIS is a non-invasive high-grade endocervical glandular lesion that is characterized by palisades of cells with cigar-shaped, hyperchromatic nuclei with coarse chromatin, nuclear enlargement with high N/C ratios, pseudostratification, and mitotic activity usually with apoptotic bodies.
Histological variants, that include conventional, endometrioid, tubal, intestinal, and stratified mucinous, are diagnostically challenging. This is true even on biopsies and LEEP specimens.[14,15] However, a few features such as intestinal differentiation are always suspicious for significant lesion because non-neoplastic intestinal metaplasia is exceedingly rare in endocervix. Most of these variants of AIS may have to be interpreted as AGC-NOS or AGC endocervical-NOS.
Diagnostic criteria
The cell groups show palisading nuclear arrangement with elongated oval- to cigar-shaped nuclei, which protrude out along the periphery because of scant cytoplasm related to high N/C ratio. This is typically referred to as nuclear feathering. This feature is better seen in conventional direct Pap smears as compared to liquid-based cytology (LBC) preparations [Figure 10]
The groups present as sheets, clusters, pseudostratified strips, and rosettes with nuclear crowding and overlap without well-defined honeycomb pattern
High N/C ratios
Variation in nuclear size
Nucleoli are usually inconspicuous (chromocenters should not be confused for nucleoli)
Mitoses and apoptotic bodies may be present
Background is typically clean without diathesis, although inflammatory debris may be present
Atypical squamous cells may be present if there is a coexisting squamous lesion [Figures 4 and 11].
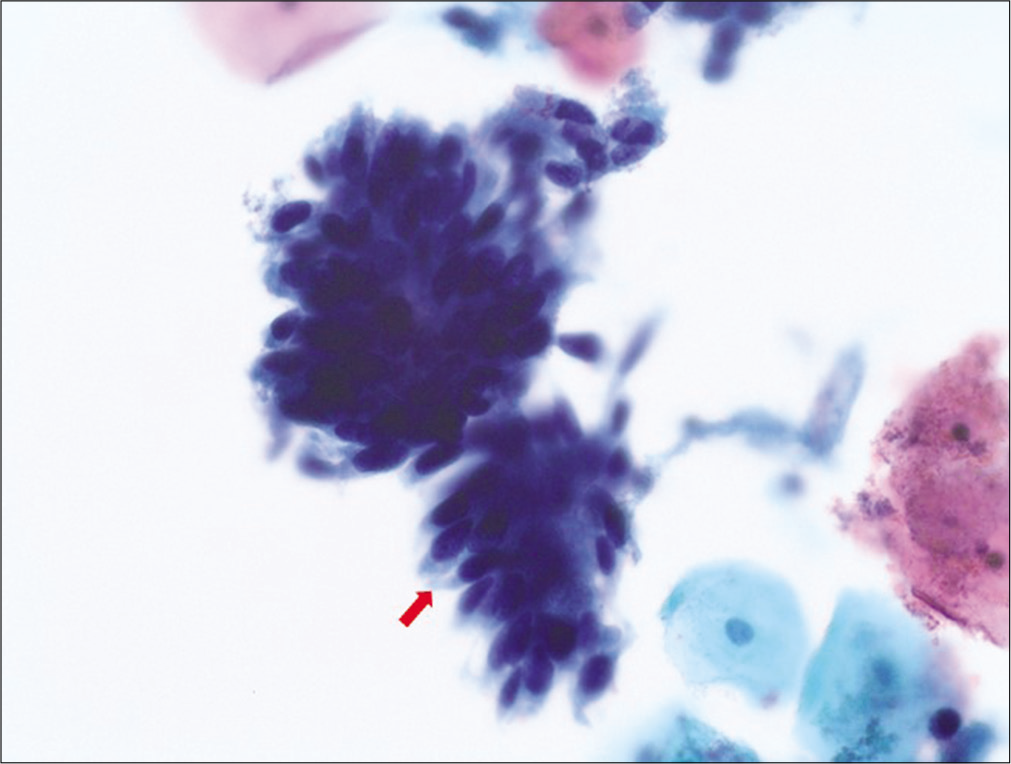
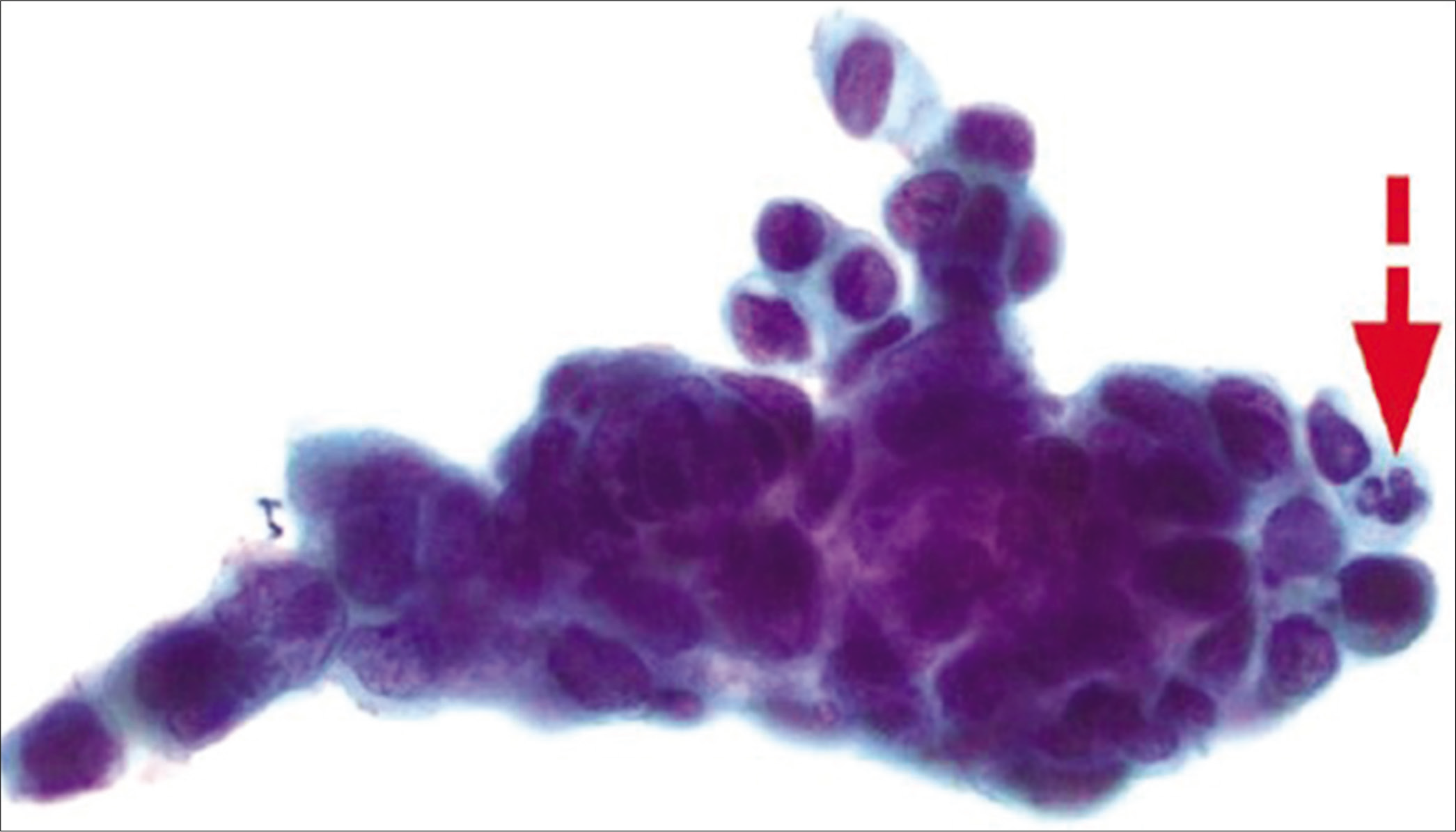
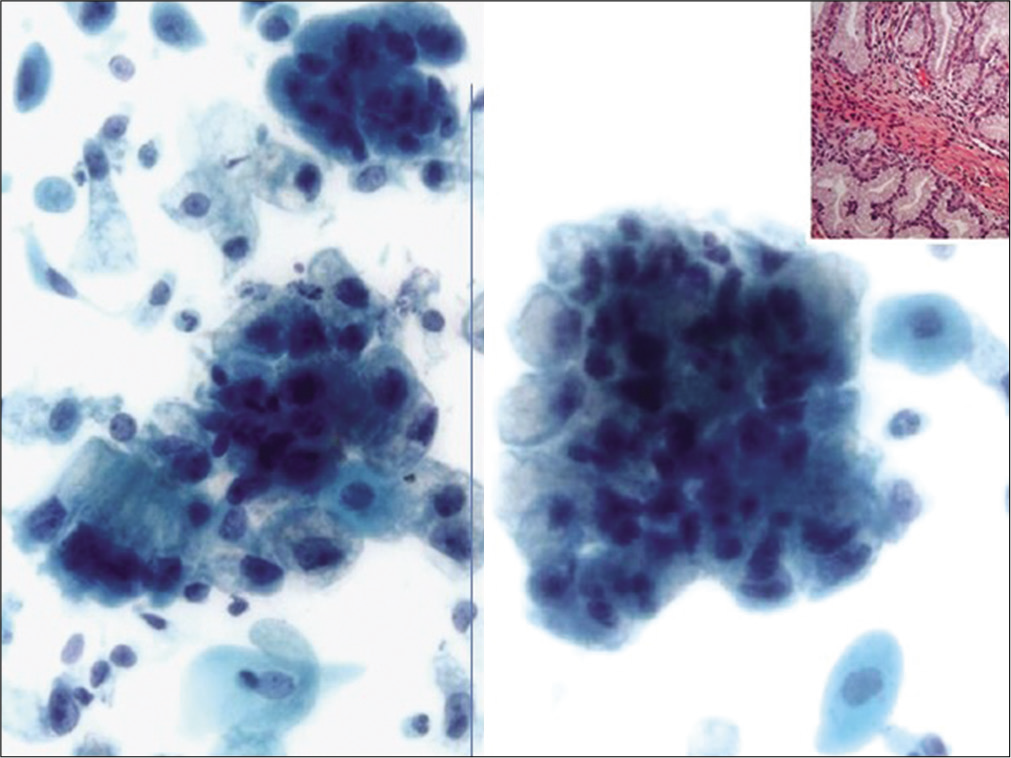
- Adenocarcinoma in situ (AIS): hyperchromatic crowded groups (HCGs) of cells exhibiting high N/C ratio with elongated (cigar shaped), hyperchromatic nuclei without nucleoli with some variation in nuclear sizes and lacy cytoplasm. Note the “feathering” of the protruding nuclei at the periphery of the HCG.
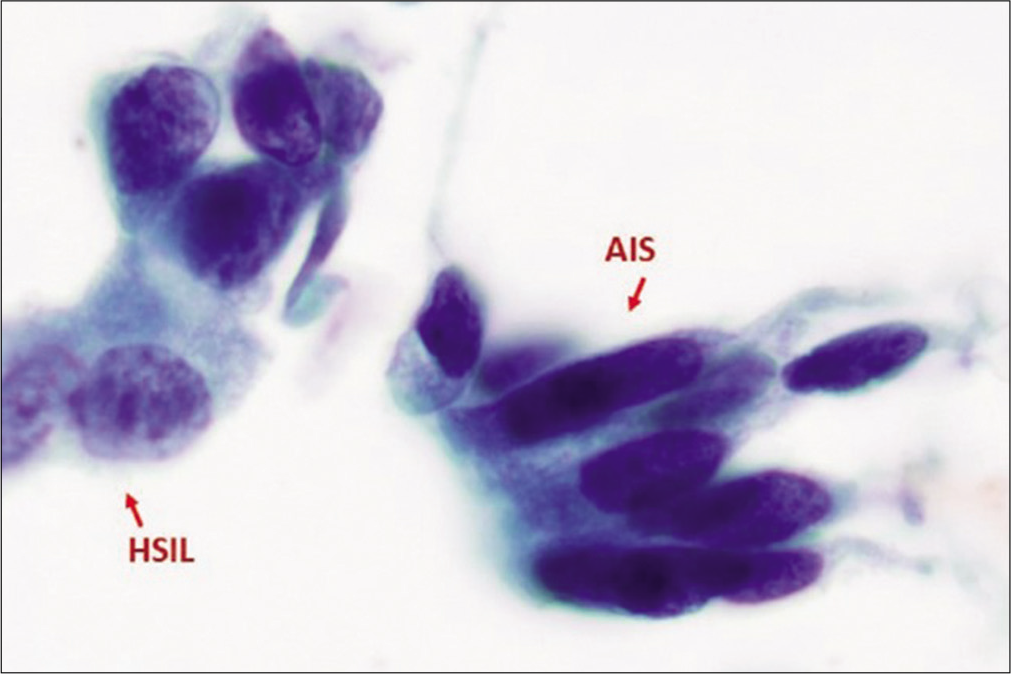
- Adenocarcinoma in situ (AIS) along with HSIL. AIS cells exhibits nuclear atypia characterized by hyperchromasia without nucleoli similar to that seen in HSIL, but with cigar-shaped elongated nuclei with lacy cytoplasm (as compared to dense, metaplastic cytoplasm in HSIL cells). (Reproduced under Open-Access charter from Ref #31).
Differential diagnosis
-
Non-neoplastic HCGs [Figure 3]
HCG of endometrial cells: Small tight spherical structures of small cells, mixed gland/stromal fragments with spindle cell stromal fragments (may have blood vessels) with hyperchromasia. The spherical groups usually show epithelial cells along the periphery with stromal component in the center. The cells show high N/C ratio with nuclear contour irregularities without significant nuclear atypia. Nucleoli are usually not prominent
HCG of tubal metaplastic cells: Group of columnar cells with cilia and/or terminal bars round to oval dark nuclei with high N/C ratio with pseudostratification. Goblet cells may be seen. Pleomorphism may be present. Lack of apoptotic bodies, coarse chromatin, uneven chromatin distribution with parachromatin clearing.
HCG of parabasal cells: Groups of cells with higher N/C ratio and overlapping relatively bland oval to round nuclei with tiny nucleoli. Usually seen in the background of atrophic cellular changes.
-
High-grade squamous intraepithelial lesion (HSIL)
HSIL cell groups with enlarged hyperchromatic nuclei with coarse chromatin (also without nucleoli similar to AIS) may resemble AIS. However, HSIL nuclei are mostly round to oval (in contrast to elongated, cigar-shaped nuclei in AIS) without palisading and without nuclear feathering in syncytial groups with nuclear overlap
Degree of nuclear enlargement is more variable. Nuclear contours may be irregular.
Nuclei are generally hyperchromatic but may be normochromatic or rarely even hypochromatic.
Chromatin may be fine or coarsely granular and is evenly distributed.
Nucleoli are generally absent, but may occasionally be seen along the periphery of groups, particularly when HSIL involves endocervical glands.
Appearance of the cytoplasm is usually metaplastic, but variable (“immature,” lacy, and delicate or densely metaplastic, occasionally, “mature,” and densely keratinized).
Atypical glandular cells (AGCs)
AGC endocervical, NOS
This category includes AGCs with a morphology that is short of adenocarcinoma but overlap with reactive endocervical cells and cells with reparative changes. Other factors limiting the definitive interpretation of adenocarcinoma may be quantitative and/or other qualitative issues including poor preservation and degenerative changes.
The qualifier “favor reactive” is potentially misleading and, therefore, is not included in the current Bethesda terminology. Instead, “Not Otherwise Specified” (NOS) is recommendation to be used with appropriate comment(s). If the index of suspicion is high, but still not meeting criteria for AIS or AdCa, the designation “favor neoplastic” (FN) may be used (See next category below). The significant morphologic feature is that it shows nuclear atypia that exceeds an obvious reactive or reparative change. The key for proper designation of atypical endocervical cells lies in the ability to exclude reactive conditions that include repair, tubal metaplasia, radiation, and intrauterine device (IUD) effect [Figures 12 and 13].
- AGC, Endocervical, NOS (specify in comment – radiation effect). This hyperchromatic crowded group shows a relatively small crowded group of cells (arrow) with cytoplasmic vacuoles (both degenerative and mucin vacuoles). The nuclei in cells with cytomegaly are around 3 times the size of intermediate cell nuclei and show minimal nuclear atypia with nuclear enlargement (but without significant change in N/C ratio), smudgy chromatin, and some variation in nuclear size with prominent nucleoli.
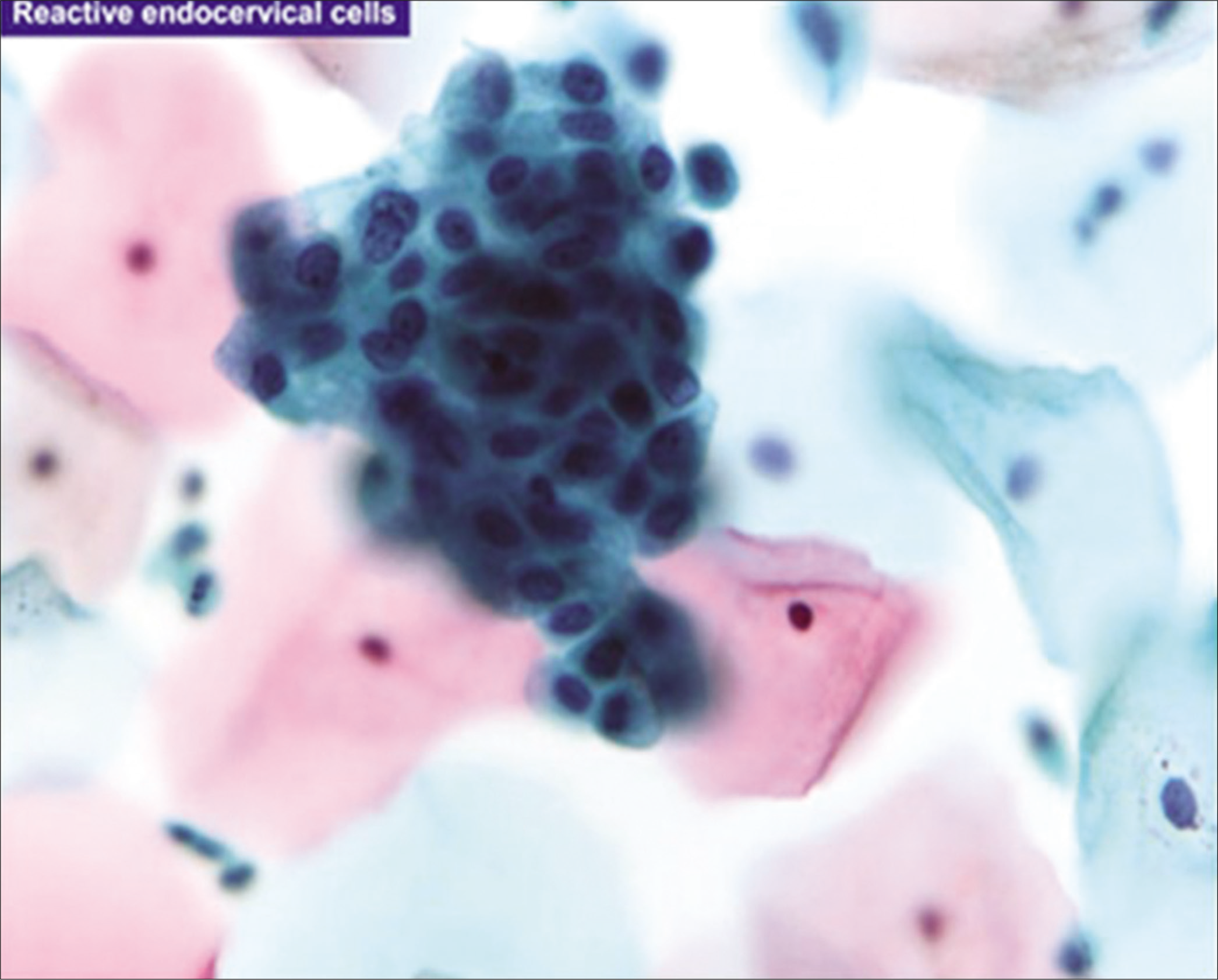
- Reactive endocervical cells with relatively prominent nucleoli and some nuclear crowding (×100). (Reproduced under Open-Access charter from Ref #35).
Diagnostic criteria
Endocervical cells with architectural atypia: Columnar cells arranged in strips and sheets with nuclear crowding, overlap, and/or pseudostratification
Nuclei are enlarged 3 to 5X size of intermediate cell nuclei (ICN)
Minimal variation in chromatin pattern and nuclear size
Higher nuclear to cytoplasmic ratios
Cell borders may be ill-defined.
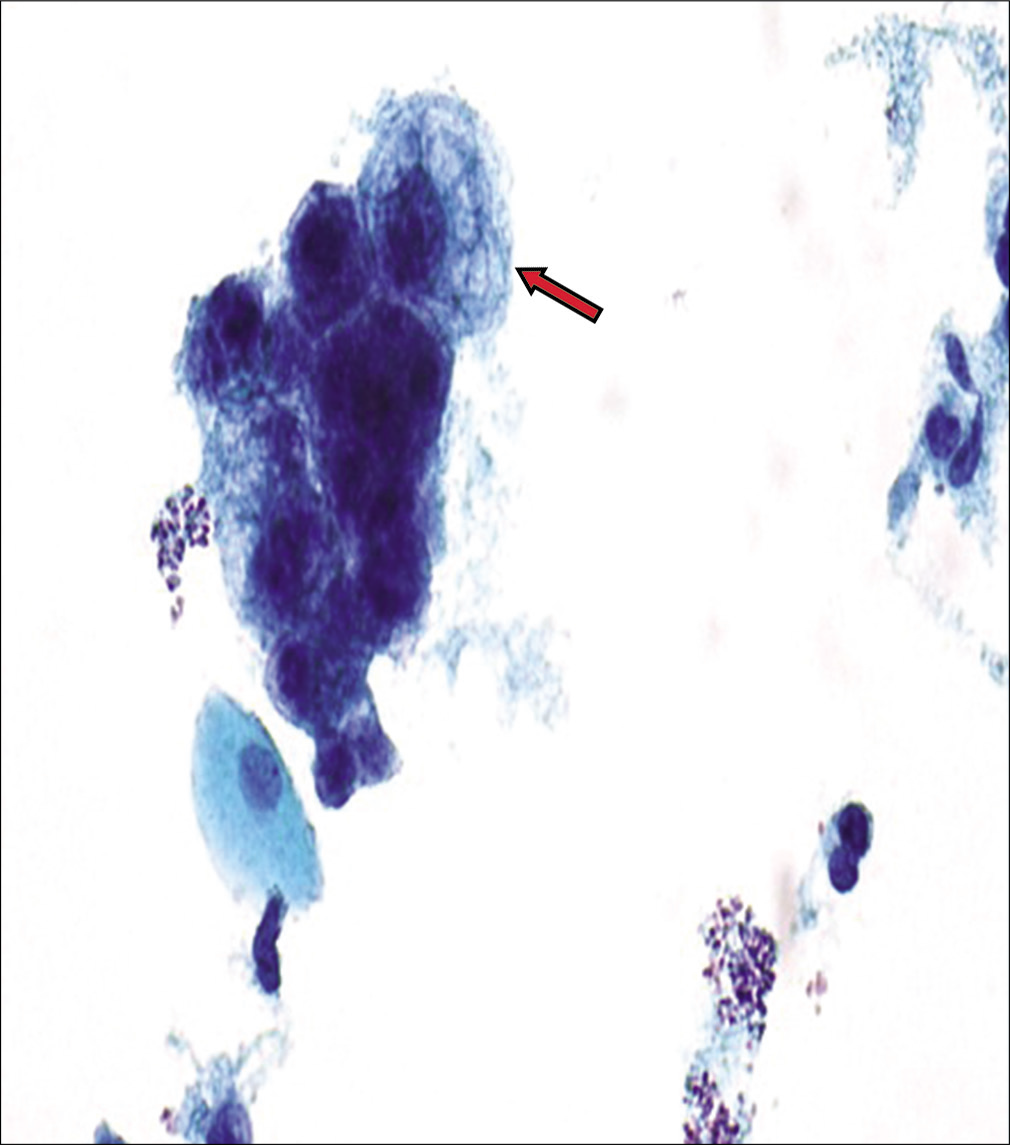
AGC endocervical, favor neoplastic
This category includes AGCs with a morphology that is suggestive of endocervical adenocarcinoma but either quantitatively or qualitatively falls short of an interpretation of endocervical adenocarcinoma.
Diagnostic criteria: [Figures 14 and 15]
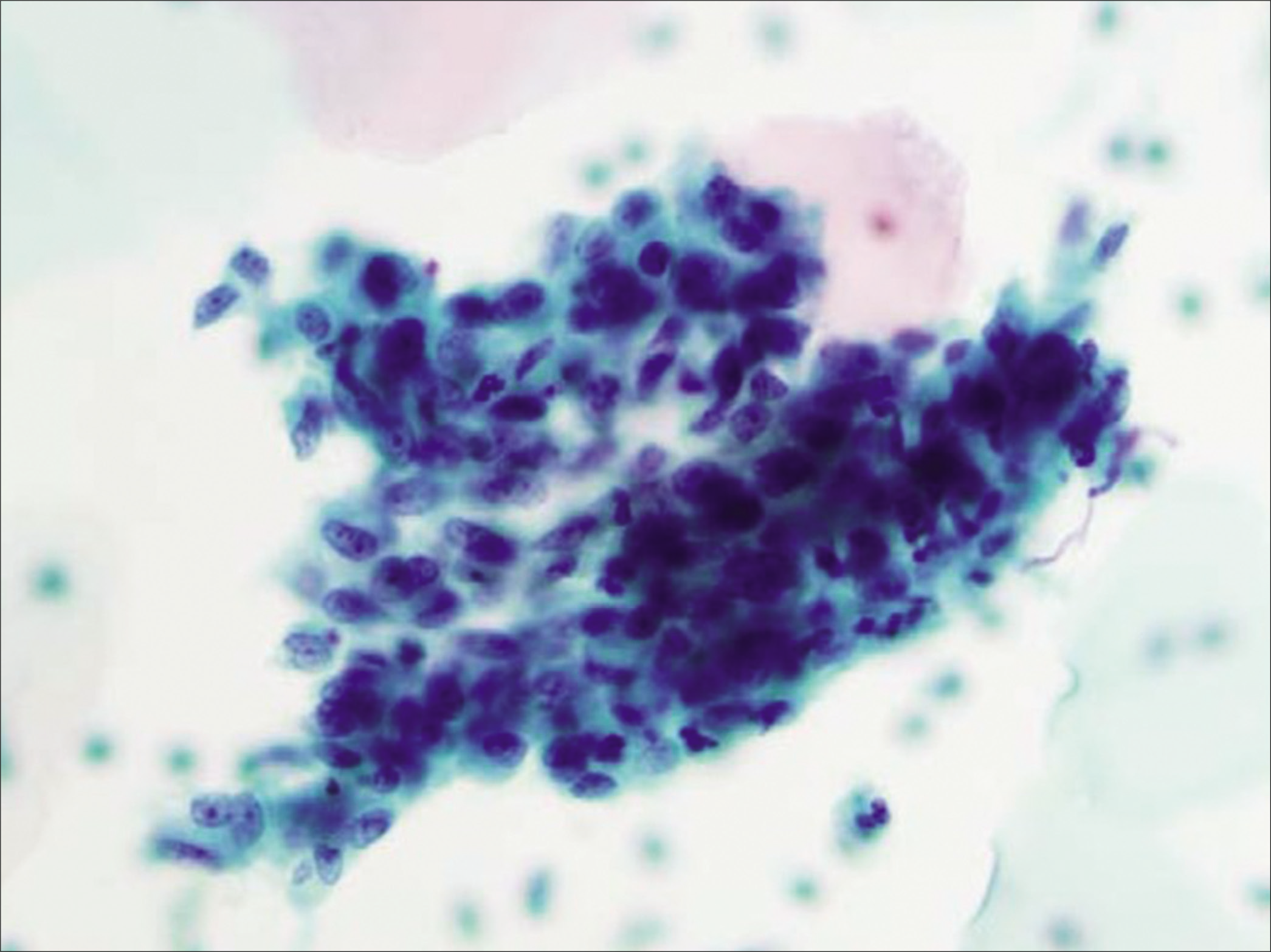
- Atypical glandular cells (AGCs), endocervical, favor neoplastic: three-dimensional groups of endocervical cells with enlarged nuclei (5X ICN) with nucleoli and some nuclear overlap of the randomly oriented nuclei (×40). (Reproduced under Open-Access charter from Ref #35).
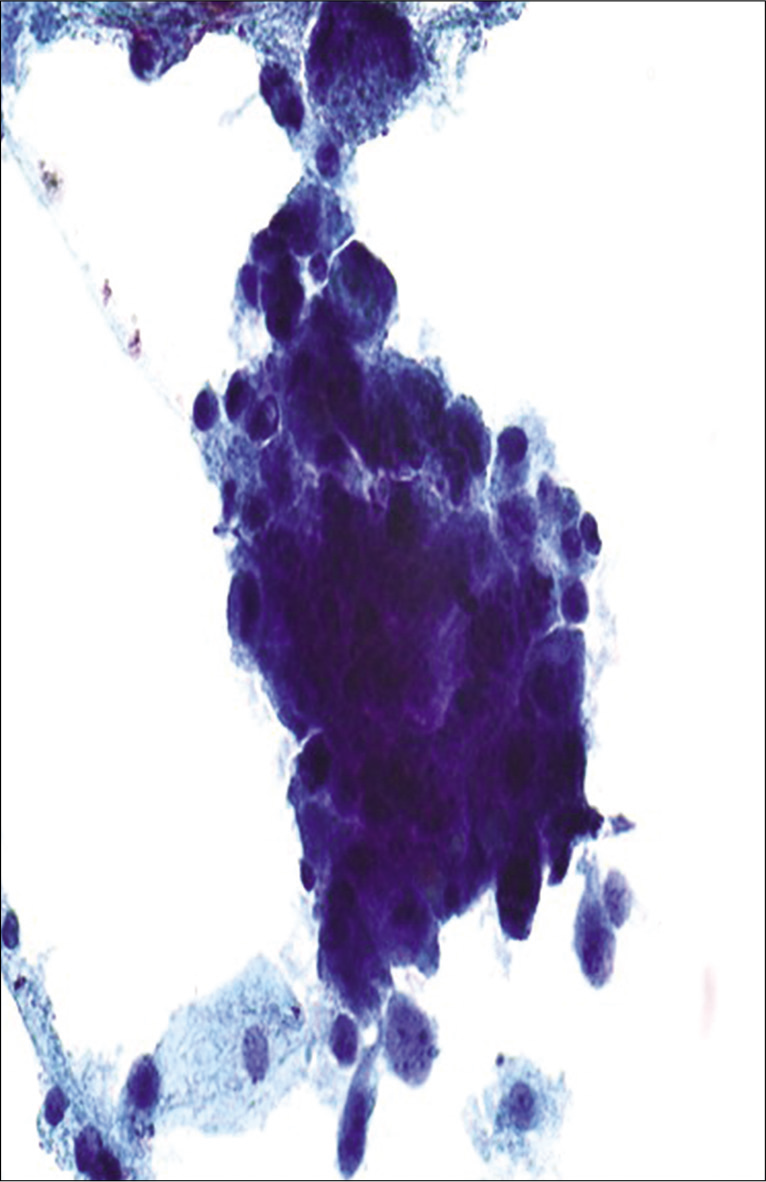
- Atypical glandular cells (AGCs), endocervical, favor neoplastic: poorly preserved hyperchromatic crowded group of cells with high N/C ratio and enlarged nuclei (more than 5X ICN) with nuclear overlap. Cytoplasm is finely vacuolated (definitive interpretation is limited due to poor preservation).
Endocervical cells with architectural atypia: Columnar cells arranged in strips and sheets with nuclear crowding, overlap, and/or pseudostratification
Rare cell groups with high N/C ratio and rosettes (gland formations)
Large nuclei (3 to 5X size of ICN) hyperchromatic nuclei with coarse chromatin with heterogeneity
Occasional mitoses with or without apoptotic bodies.
Approach to diagnosis
On a low-power screening, multiple three-dimensional HCGs or two-dimensional sheets or strips of hyperchromatic cells can be identified with variable degree of overlapping.[16,17]
On higher magnification, the two most important criteria are nuclear size and chromatin pattern. Enlarged nuclei (3 to 5X ICN) with nucleoli and increased nuclear to cytoplasmic ratio are best assessed at the periphery of a given group. The characteristics features of atypia; hyperchromasia; and slightly coarse chromatin are present with a slightly irregular nuclear membrane. Occasionally, mitotic figures and apoptotic debris can be seen. However, inability to evaluate nuclear details of the atypical cells in the central area of such HCGs of HSIL with glandular involvement may be misinterpreted as AGC.
AGCs with ill-defined nuclear feathering may be interpreted as AGC, favor neoplastic. Feathering, characterized by nuclear protrusion from the periphery of the group, is a feature that can be identified easily on conventional Pap smear. It is not distinctly appreciated in a liquid-based preparation.[9] Overall, category of “endocervical glands, favor neoplastic,” may be selected when the atypical features are not convincing enough for definitive interpretation as adenocarcinoma.
AGC endometrial (AEM)
This category includes AGC with cytomorphological features of abnormal endometrial cells. Due to the lack of poor reproducibility, this category is not further designated as favor neoplastic or NOS. Endometrial cells with atypical features represent a wide spectrum of conditions, and it is not possible to predict malignancy based on these features.
The distinction of cytologically atypical endometrial cells is based primarily on the criterion of increased nuclear size with occasional nucleoli. In addition to endometrial hyperplasia and endometrioid carcinoma, AGC endometrial may be associated with endometrial polyps, chronic endometritis, and IUD.
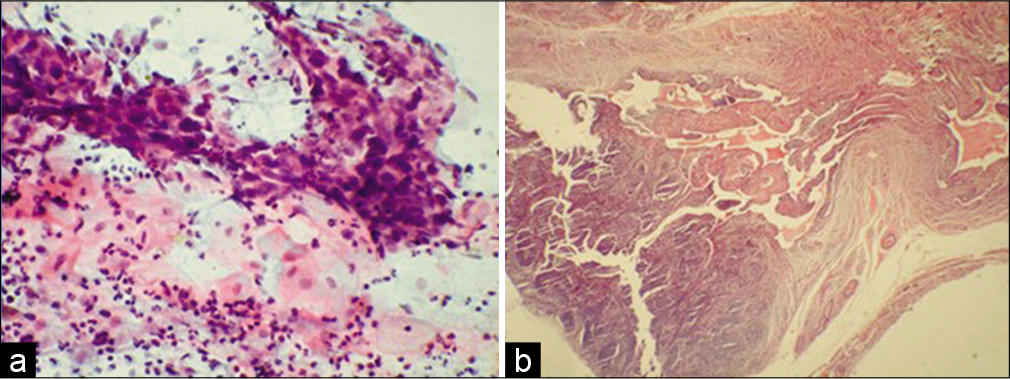
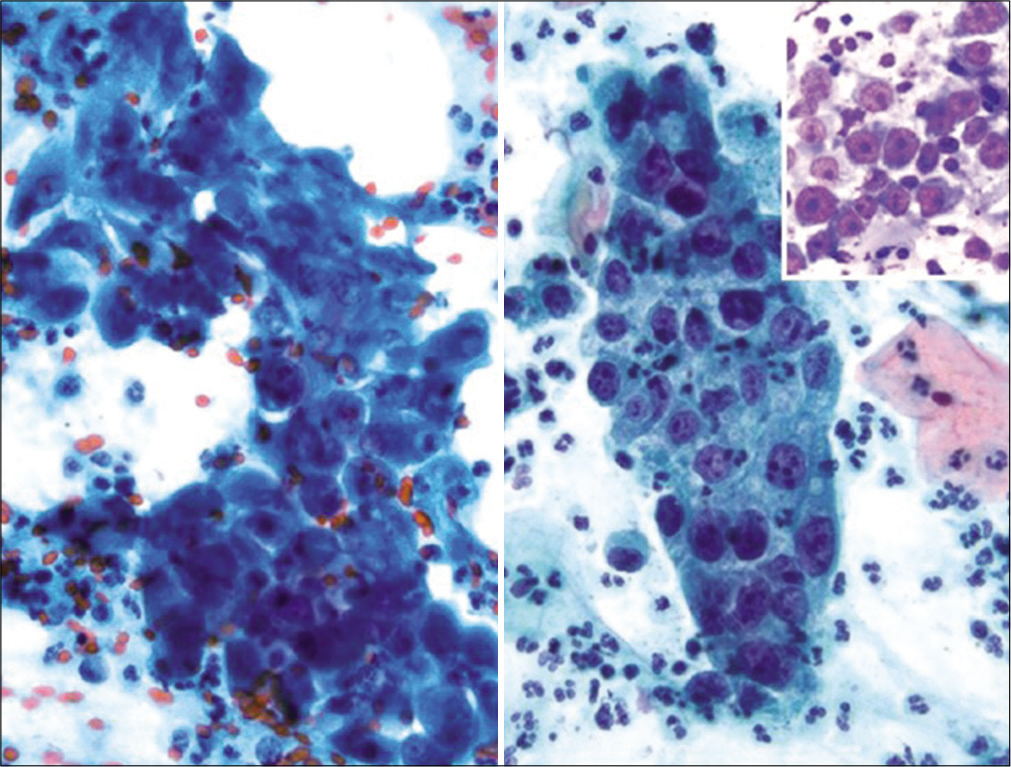
Diagnostic criteria: [Figures 16 and 17]
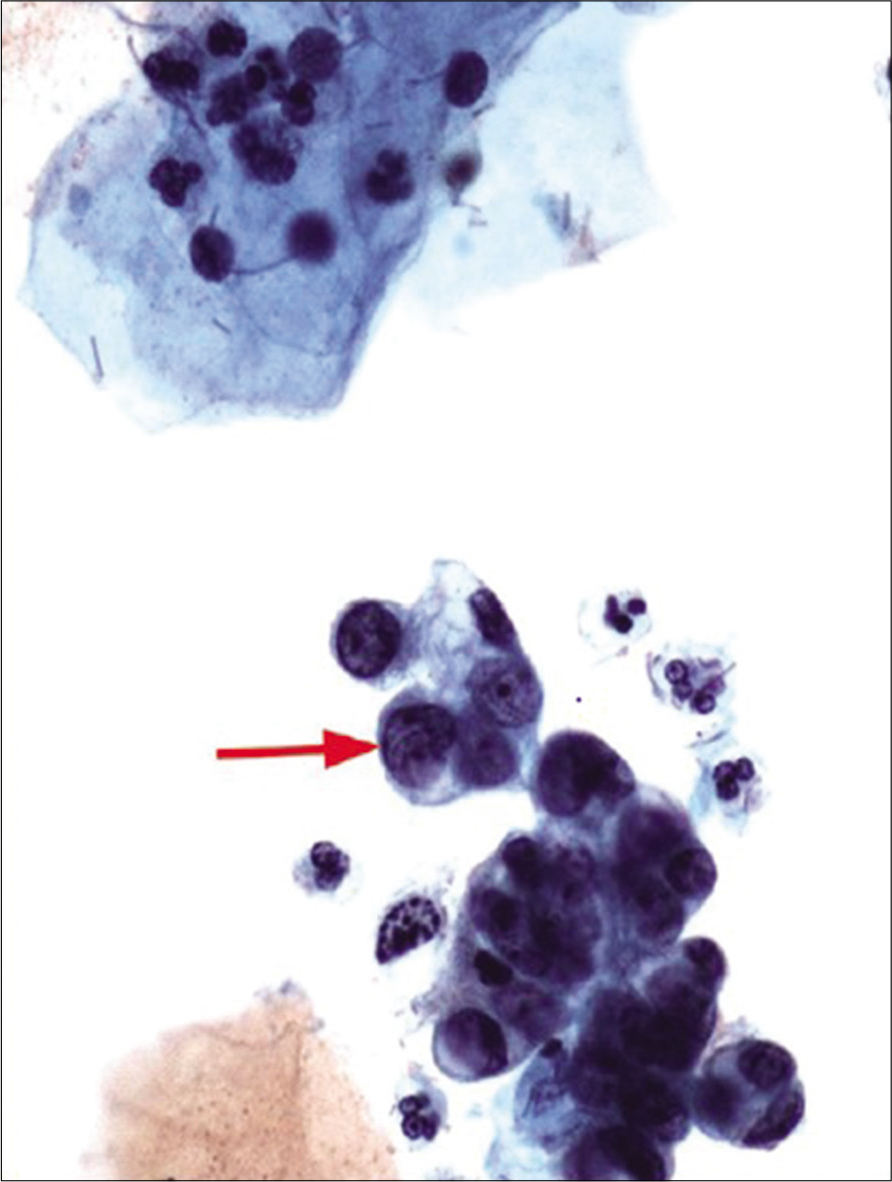
- Atypical glandular cells (AGCs)-endometrial cells (NOS) hyperchromatic crowded group of cells with nuclear size larger than normal endometrial cells (twice that of an intermediate cell nucleus) (red arrow). The nuclei show nucleoli. The histologic follow-up is well-differentiated endometrioid adenocarcinoma, FIGO Grade 1. Pap stain, ×40 (Reproduced under Open-Access charter from Ref #27).
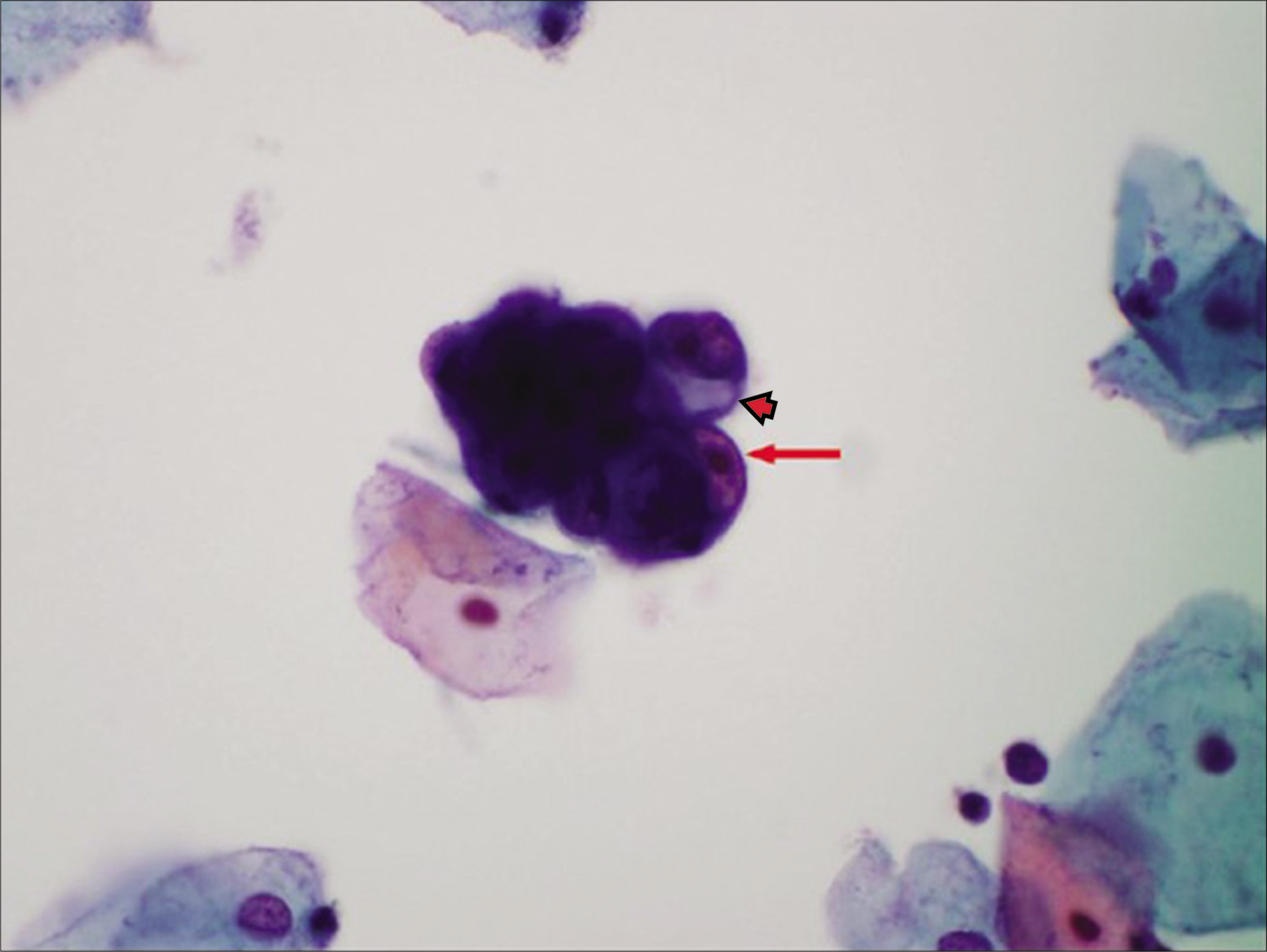
- Atypical glandular cells (AGCs)-endometrial cells (NOS) atypical endometrial cells as a small hyperchromatic crowded group of glandular cells with visible nucleoli (red arrow) with cytoplasmic vacuole (arrowhead). The histologic follow-up is endometrial intraepithelial neoplasia. (Pap stain) (Reproduced under Open-Access charter from Ref #27).
Small cohesive HCGs of endometrial cells with usually 5–10 cells per group
Nuclei are slightly enlarged compared to normal endometrial cells
Mild hyperchromasia
Chromatin heterogeneity
Occasional small nucleoli
Scant cytoplasm occasionally shows vacuole (degenerative)
Cell borders are ill defined.
Approach to diagnosis
Under low-power HCGs are seen as spheres of small groups of cells and may resemble exodus of three-dimensional cluster of endometrial cells with high N/C ratio.[18] The individual nuclei appear larger than the normal endometrial nuclei. On high power, the nuclei are hyperchromatic, with occasional small nucleoli. The cytoplasm is usually scant, with occasional cytoplasmic vacuolation (degeneration related) can be seen with ill-defined cell borders.
Differential diagnoses/mimickers of AGC
-
The nuclei of HSIL cells do not show easily detectable nucleoli (chromocenters may be present but should not be confused with nucleoli) unless associated with endocervical cells in cases with HSIL with endocervical gland involvement
The nuclei of HSIL cells although larger than ICN are smaller than AGC nuclei
Nuclear-to-cytoplasmic ratio is higher in HSIL compared to AGC
HSIL nuclear contours are usually irregular as compared to AGC
HSIL cell cytoplasm is variable but usually “immature” dense, homogeneous cyanophilic (with or without vacuoles) but may be “mature” densely keratinized. Compared to lacy delicate or vacuolated cytoplasm in AGC cells.
-
Small-cell carcinoma and other high-grade tumors [Figure 19]
Small-cell neuroendocrine carcinoma is an uncommon and highly aggressive carcinoma of the cervix. Like small-cell carcinoma of other locations, it is composed of relatively uniform small cells with scant cytoplasm. On low power, the cells are seen in loosely cohesive hyperchromatic groups. Under high power, the cells show hyperchromatic nuclei without nucleolar prominence with salt-and-pepper chromatin and scant cyanophilic cytoplasm. Some groups may show crush artifact
Other differential diagnosis in this category includes small-cell primitive neuroectodermal tumor, melanoma, and undifferentiated carcinoma
-
Tubal metaplasia[20]
HCG of tubal metaplastic cells may mimic HCG of AGC cells (may be with singly scattered tubal cells in the background)
Strips of columnar cells with nuclear overlap and pseudostratification (without nuclear feathering)
Usually cilia or terminal bars are seen
Round to oval dark nuclei may show size variation with increased N/C ratio
Some nuclei may be washed out and intervening peg cells may be present
Lacks: Apoptotic bodies, coarse chromatin, uneven chromatin distribution, and parachromatin clearing
-
Endocervical polyp
Disorganized HCGs associated with neutrophils and florid reactive/reparative changes
Inflammatory background
Immature metaplastic cells may have hyperchromasia
Nuclei with nucleoli may be enlarged but not large enough
Mitotic figures may be present but without apoptosis
Lacks: Coarse chromatin, marked nuclear contour irregularities, and parachromatin clearing.
-
Endometrial polyp
Clusters of endometrial cells with high N/C ratio as small three-dimensional spheres or papillary-like configurations
Large gland and stromal fragments
Nuclear atypia varies based on surface abrasion
Some nuclear enlargement but not large enough
Hyperchromasia
Mitoses usually without apoptosis may be seen.
-
Lower uterine segment: [Figure 20]
HCG as small tight clusters of small cells with or without stroma
Spindle cell stromal fragments
Fragments may have blood vessels
Lack: Marked nuclear atypia.
-
Cervical endometriosis
HCG as small tight groups of small cells with or without stroma
Spindle cell stromal fragments
Fragments may have blood vessels
Lack: Marked nuclear atypia in the endometrial epithelial and stromal cells.
-
Microglandular hyperplasia[21,22]
Wide spectrum ranging from HCG with or without acini.
Mild nuclear enlargement
Mild nuclear contour irregularities
Mild hyperchromasia
Small pseudoparakeratotic cells may be seen.
Inflammation
Lacks convincing nuclear features of dysplasia
Metaplastic cells with normoblast-type apoptosis (apoptotic bodies restricted to area of nucleus as seen in normoblast)[21] may be present
Presence of neutrophils.
-
Lobular endocervical glandular hyperplasia[22]
HCGs of glandular cell clusters as monolayered sheets with uniformly small nuclei
Cytoplasm with golden-yellowish mucin
Complex glandular structures
Mucin localization along the surface of glandular cell clusters.
Goblet cells may be seen
N/C ratio usually <50%
Mild nuclear enlargement
Conspicuous nucleoli
Nuclear pseudoinclusions may be seen
Lack: Marked nuclear atypia.
-
Cohesive sheets of enlarged interdigitating cells often in a classic “school of fish” architecture or may be mechanically distorted by sampling and elongate to form “taffy pull” cytoplasmic appendages
Nuclear enlargement of a variable degree
Vesicular and hypochromatic nuclei are typically non-overlapping
Occasional binucleation or multinucleation may be observed
Nuclear outlines are smooth, round, and uniform
Usually uniformly distributed and finely granular chromatin
Prominent single or multiple nucleoli may be present
Well-defined cytoplasmic boundaries
Cytoplasm may show polychromasia, vacuolization, or perinuclear halos but without peripheral thickening.
-
Ionizing radiation effect: [Figure 12]
Clusters of HCG with isolated cells
Cytomegaly with normal or low N/C ratio
Dense two tone often vacuolated cytoplasm
Large clear to vesicular to smudgy nuclei
Macronucleoli
Inflammation
More obvious reparative changes in squamous than endocervical cells
Lacks: Mitoses, apoptosis, and markedly high N/C ratio.
- HSIL showing irregular nuclear contours with subtle indentations. Some nuclei may show longitudinal Tulip flower bud-like folds (black arrows). Occasional chromocenters (arrowheads) should not be mistaken for nucleoli to prevent misinterpretation as AGC or AdCa.
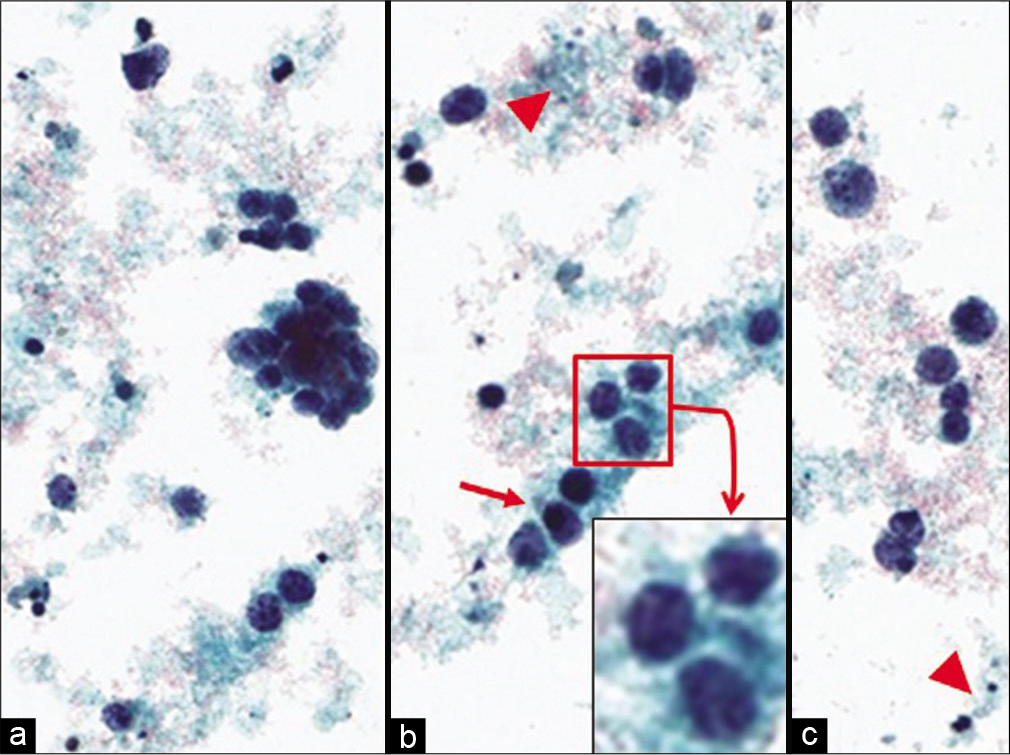
- Small-cell carcinoma in Pap stained ThinPrep™. The malignant cells are dispersed as single cells (c) and loosely cohesive hyperchromatic crowded groups (a) with nuclear molding (arrow) (b) and with tumor diathesis in the background (arrowhead). The cells with high N/C ratios show nuclei with “salt-and-pepper” chromatin (better seen in some well-preserved cells) without detectable nucleoli (inset of b) tumor cells may show mitotic figures with apoptosis (arrowhead). (Pap stain, ThinPrep, ×400) (Interpretation partially limited by degenerative changes). (Reproduced under Open-Access charter from Ref #28).
- Lower uterine segment (LUS) cells: Three-dimensional clusters of hyperchromatic crowded groups with indistinct cell borders and scant cytoplasm. Round to oval nuclei are small and are of same size as an intermediate squamous cell nucleus. Small and subtle nucleoli are present.
![Atypical repair (Pap stained SurePath) cells are arranged in a two-dimensional sheet with abundant cytoplasm showing a “pulled-out” or streaming effect (school-of-fish pattern). Nuclei exhibit prominent nucleoli (arrows) with some pleomorphism. Some cells may have multiple nuclei. These changes, although indicative of a reparative reaction, may resemble AGC because of the nuclear pleomorphism noted. In favor of a reactive process is relatively smaller nuclei (smaller than 5X ICN) with generally fine chromatin. These may be misinterpreted as AGC. The preferred approach would be to categorize them as ASC – atypical repair. (Adopted from CytoJournal open access. Chivukula M, Shidham VB. Cytojournal 2006;3:14)[10]](/content/105/2022/19/1/img/Cytojournal-19-31-g021.png)
- Atypical repair (Pap stained SurePath) cells are arranged in a two-dimensional sheet with abundant cytoplasm showing a “pulled-out” or streaming effect (school-of-fish pattern). Nuclei exhibit prominent nucleoli (arrows) with some pleomorphism. Some cells may have multiple nuclei. These changes, although indicative of a reparative reaction, may resemble AGC because of the nuclear pleomorphism noted. In favor of a reactive process is relatively smaller nuclei (smaller than 5X ICN) with generally fine chromatin. These may be misinterpreted as AGC. The preferred approach would be to categorize them as ASC – atypical repair. (Adopted from CytoJournal open access. Chivukula M, Shidham VB. Cytojournal 2006;3:14)[10]
Adenocarcinoma (AdCa)
Adenocarcinoma endocervical
Advanced endocervical adenocarcinoma may present as an exophytic mass, an ulcerative plaque, or barrel-shaped diffuse cervical enlargement.[24] Early disease may be accompanied by a component of AIS and can be seen on Pap smears.
Diagnostic criteria
Many abnormal single cells, two-dimensional sheets or three-dimensional clusters, and syncytial aggregates
Cells are columnar in shape
Enlarged nuclei with macronucleoli
Round to oval nuclei may be pleomorphic with irregular chromatin distribution, chromatin clearing, and nuclear membrane irregularities
Cytoplasm is usually finely vacuolated
Necrotic tumor diathesis is common
Abnormal squamous cells may be present, representing a coexisting squamous lesion or the squamous component of an adenocarcinoma showing partial squamous differentiation.
Approach to diagnosis
Pap smears show diverse morphologic appearance based on the histologic subtypes of invasive adenocarcinoma. On low power, HCG of adenocarcinoma cells may present in acinar or papillary clusters, or as highly vacuolated groups, or in large complex structure like a microbiopsy, or as singly scattered cells. Under higher magnification, the cells with high N/C ratio show enlarged, hyperchromatic, pleomorphic, vesicular nuclei with irregular nuclear membrane show prominent nucleoli. The best possible factor that supports adenocarcinoma is tumor diathesis. These findings may be present on the background of cytomorphological features of AIS in early invasive adenocarcinoma.
Adenocarcinoma, endometrial (AdCa-EM)
Cytopathological detection of endometrial adenocarcinoma in cervical Pap smears is limited by the small number of well-preserved abnormal cells. Thus, there are generally fewer abnormal cells present as compared to endocervical cancer.
Diagnostic criteria
Cells may typically occur singly or in small clusters
In well-differentiated tumors, nuclei may be only slightly enlarged, compared to nonneoplastic endometrial cells, becoming larger with increasing grade of the tumor [Figure 22,23]
Variation in nuclear size and loss of nuclear polarity
Nuclei display moderate hyperchromasia, irregular chromatin distribution, and parachromatin clearing, particularly in high-grade tumors
Small to prominent nucleoli; nucleoli become larger with increasing grade of tumor
Cytoplasm is typically scant, cyanophilic, and often vacuolated
Isolated cells or small groups of tumor cells may show intracytoplasmic neutrophils, often with the appearance of a “bag of polys”
A finely granular or “watery” tumor diathesis is variably present, most commonly in conventionally prepared specimens (clinging diathesis in LBC).
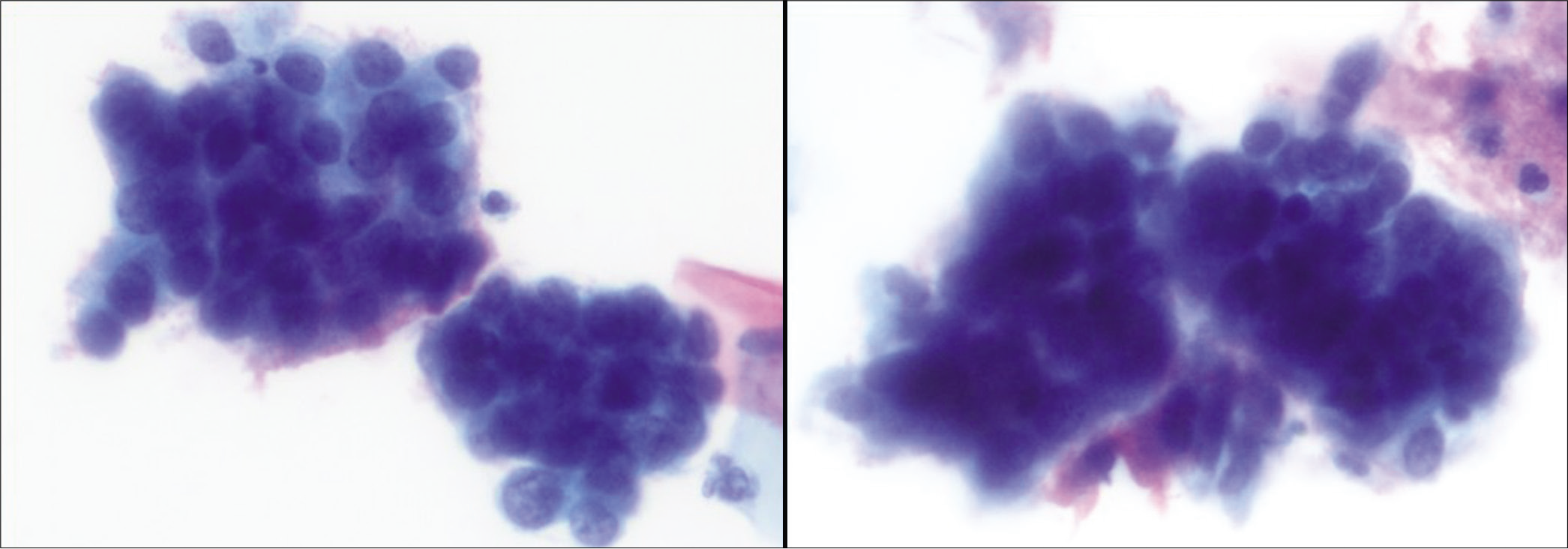
- Endometrial adenocarcinoma cells showing a large hyperchromatic crowded group of glandular appearing cells with focal cytoplasmic vacuole containing neutrophils (red arrow). Some cells show nucleoli. The histologic follow-up is well-differentiated endometrioid adenocarcinoma, FIGO Grade 1. (Reproduced under Open-Access charter from Ref #27).
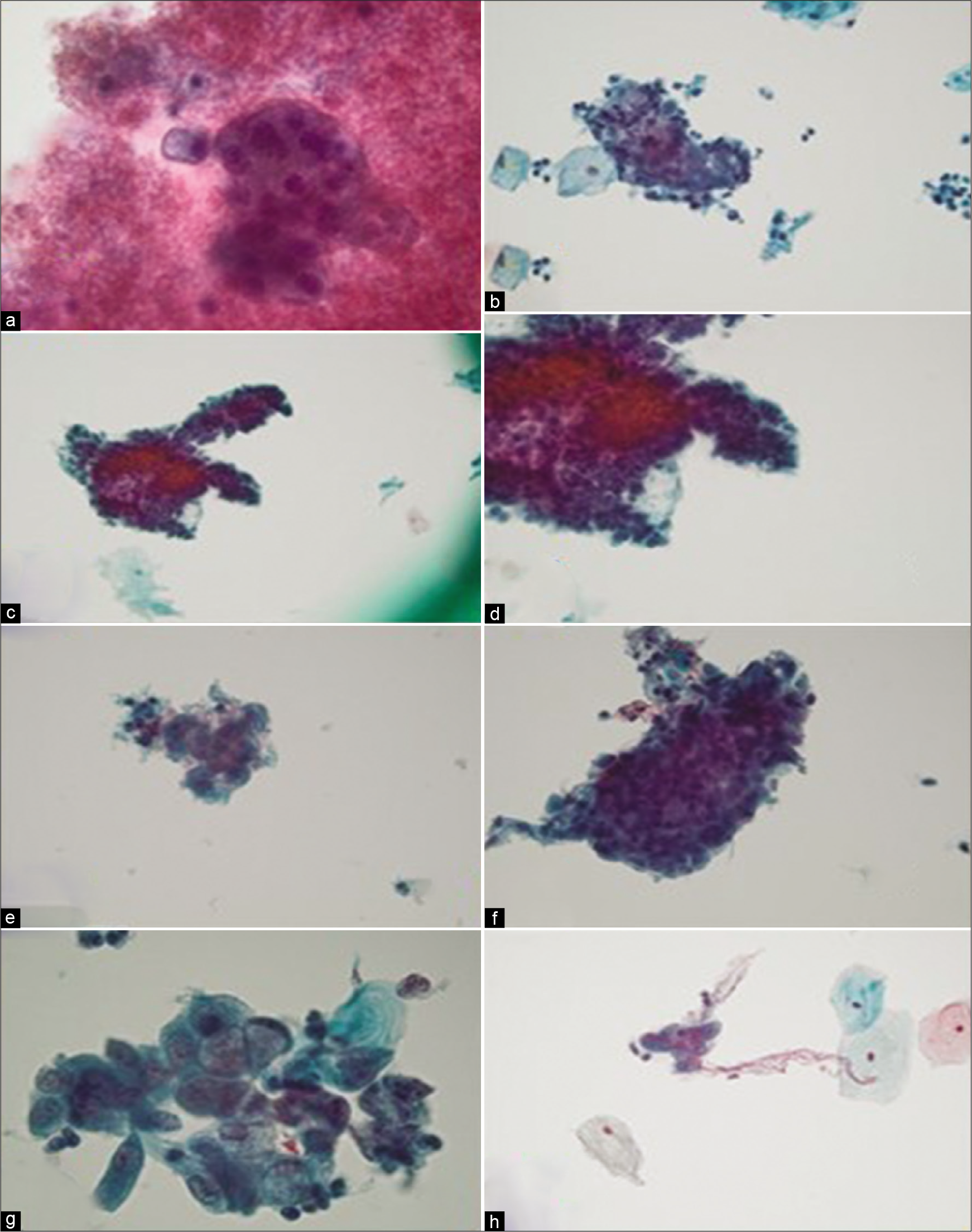
- Endometrial adenocarcinoma (a) Case 1: Dense, bloody diathesis obscuring a large monomorphic cell group in hypocellular specimen (×60). (b) Case 2: A tightly cohesive group with overlapping nuclei with obscured nuclear details (×40). (c and d) Case 3: Minimal diathesis with rare, large, cohesive group of glandular cells with obscured cellular detail (×20 in c, ×40 in d). (e) Case 4: Hypocellular specimen with rare, small epithelial group with neutrophils (×40). (f) Case 5: Rare, large, three-dimensional group of crowded but minimally atypical glandular cells with abundant atrophic squamous sheets (×40). (g) Case 6: Rarely, a pattern with enlarged nuclei and prominent intracytoplasmic mucin may be noted some cases (×60). (h) Case 7: Very scant, small, cohesive cell groups with a clean background (×40). (Reproduced under Open-Access charter from Ref #30).
Approach to diagnosis
On low power, HCGs of atypical endometrial cells show relatively small nuclei with nucleoli. The best possible feature that supports the diagnosis is tumor diathesis (watery tumor diathesis in conventional smears and clinging diathesis in LBC).
On higher power, the HCGs show atypical pleomorphic nuclei with irregular chromatin distribution with prominent nuclei [Figure 22,23].
Adenocarcinoma, extrauterine
Although rare, extrauterine carcinomas such as primary carcinoma from the ovary, GI tract, and breast have been reported in a PAP smear [Figures 5 and 24].[25] The involvement of vagina secondary to metastasis is the common cause. Certain cases show direct extension of the tumor to the endometrial cavity or rarely due to a transit of tumor cells from the abdominal cavity through the fallopian tube into the endometrial cavity without an actual metastasis.
- Adenocarcinoma, other (a) clusters of malignant cells showing moderate pleomorphism in cervical Pap smear (Papanicolaou stain). (b) Microphotograph showing a tumor in the lumen of fallopian tube. (Reproduced under Open-Access charter from Ref #29).
Approach to diagnosis
On low power, the extrauterine carcinomas are relatively hypocellular with a clean background (lack of tumor diathesis). When diathesis is present, then the differential is for colon or bladder carcinoma. The neoplastic cell groups usually show the characteristics of the tumor type and site of origin. However, if the exfoliated groups are from a distant site, then they may show degenerative features.
On a higher power, the presence of psammoma bodies and papillary configuration of neoplastic cells cluster suggest a Mullerian carcinoma. The presence of goblet cells with diathesis suggests a colon or urachal adenocarcinoma. The presence of lymphocyte like tumor cells in the background of atrophy suggests a lobular carcinoma of the breast.
Adenocarcinoma (NOS or specify in comments)
This category includes other type of neoplasms that can arise from the cervix. The category includes glassy cell carcinoma of the cervix, minimal deviation carcinoma, clear cell adenocarcinoma, mixed Mullerian mesenchymal tumor, small-cell carcinoma, and large cell neuroendocrine carcinoma [Figures 25 and 26]. The incidence of these neoplasms diagnosed on Pap smear is extremely low. They can always present as a pitfall to diagnosis as they show features similar to other common entities with subtle differences. The use of cell-block can be highly useful in accurate diagnosis of these neoplasms.
- Adenocarcinoma, NOS: Large cell neuroendocrine carcinoma in Pap stained ThinPrep™ from a 24-year-old female. The malignant cells are loosely cohesive. The nuclei are only mildly pleomorphic with one or more prominent nucleoli (Pap stain, ThinPrep, ×400) (Reproduced under Open-Access charter from Ref #28).
- Adenocarcinoma, NOS: adenoma malignum in a liquid-based preparation (SurePath™). The specimen shows large numbers of atypical glandular clusters associated with some single endocervical-like cells with yellow/golden vacuolated cytoplasm. The cells have abnormal nuclei (enlargement, pleomorphism, crowding, visible nucleoli, and loss of polarity) (Pap stain, ×400). Inset: Corresponding cervical biopsy (H and E stain, ×400). (Reproduced under Open-Access charter from Ref #28).
The cytomorphologic features of the other types of carcinomas vary depending on the subtype of carcinoma. A few characteristic features that may help differentiate include:
Glassy cell carcinoma [Figure 27][26]
- Adenocarcinoma, NOS: Glassy cell carcinoma. Sheets of tumor cells with abundant granular (ground glass-like) cytoplasm, large pleomorphic nuclei, coarse irregular chromatin, and prominent nucleoli. An inflammatory cell infiltrate is present (Pap stain, ×400). Inset: Corresponding cervical biopsy showing prominent/large nucleoli (H and E stain, ×400) (Reproduced under Open-Access charter from Ref #28).
Glassy cell carcinoma of the cervix usually affects younger patients. It is a rare variant of poorly differentiated adenosquamous carcinoma. On a low power, tumor cells are seen as sheets and clusters with large abundant finely granular (resembling ground glass-like) cytoplasm with distinct borders. On a high power, they show a large pleomorphic nucleus with coarse irregular chromatin and distinctly prominent nucleoli. Cytoplasmic vacuoles are usually seen. The background tumor diathesis shows inflammatory cells including eosinophils with intimate association with tumor cells forming “granuloepithelial complex.”
The differential diagnosis of this entity includes other poorly differentiated neoplasms involving the cervix such as nonkeratinizing squamous cell carcinoma, poorly differentiated adenocarcinoma, and clear cell carcinoma.
Clear cell adenocarcinoma [Figure 28]
![Adenocarcinoma, NOS: Clear cell carcinoma in a conventional Pap smear. The tumor cells with vacuolated cytoplasm (b) arranged in sheets and papillae with abnormal pleomorphic nuclei and a tigroid background (a) (Pap stain, ×200 [a], and ×400 [b]). (Reproduced under Open-Access charter from Ref #28).](/content/105/2022/19/1/img/Cytojournal-19-31-g028.png)
- Adenocarcinoma, NOS: Clear cell carcinoma in a conventional Pap smear. The tumor cells with vacuolated cytoplasm (b) arranged in sheets and papillae with abnormal pleomorphic nuclei and a tigroid background (a) (Pap stain, ×200 [a], and ×400 [b]). (Reproduced under Open-Access charter from Ref #28).
Clear cell adenocarcinoma of the cervix or the vagina is a rare tumor that can occur in daughters of women who received diethylstilbestrol (DES) during pregnancy.
On a low power, cells are seen arranged in sheets, clusters, or papillae. On a high power, the tumor cells show delicate vacuolated, glycogen-rich cytoplasm, and naked nuclei with “tigroid” background. The nuclei are large, pale, and round with prominent nucleoli.
The main differential diagnosis of this entity includes glassy cell carcinoma and metastatic clear cell carcinomas.
Acknowledgment
Authors thank Dr. Pansare for the contribution of some images.
LIST OF ABBREVIATIONS (In alphabetic order)
AdCa – Adenocarcinoma
AdCa-EM - Adenocarcinoma, endometrial
AEM - AGC endometrial
AGC – Atypical glandular cells
AIS – Adenocarcinoma in situ
ASC – Atypical squamous cells
BIRST-2 – Bethesda inter-observer reproducibility study
DES – Diethylstilbestrol
HCG – Hyperchromatic crowded group
HPV – Human papillomavirus
hrHPV – High-risk
HPV HSIL – High-grade squamous intraepithelial lesion
ICN – Intermediate cell nuclei
LBC – Liquid-based cytology
LSIL – Low-grade squamous intraepithelial lesion
LSIL-H – LSIL, cannot rule out
HSIL N/C – Nuclear/cytoplasmic
NOS – Not otherwise specified
Pap – Papanicolaou
SAPK – Small atypical parakeratotic
yr – Year
References
- Efficacy of the bivalent HPV vaccine against HPV 16 / 18-associated precancer: Long-term follow-up results from the costa Rica vaccine trial. Lancet Oncol. 2020;21:1643-52.
- [Google Scholar]
- Clinical significance of atypical glandular cells in Pap tests: An analysis of more than 3000 cases at a large academic women’s center. Cancer Cytopathol. 2016;124:589-95.
- [Google Scholar]
- Atypical glandular cells of undetermined significance Outcome predictions based on human papillomavirus testing. Am J Clin Pathol. 2004;121:87-92.
- [Google Scholar]
- Risk of invasive cervical cancer after atypical glandular cells in cervical screening: Nationwide cohort study. BMJ. 2016;352:i276.
- [Google Scholar]
- Detection of endometrial adenocarcinoma with the ThinPrep Pap test. Diagn Cytopathol. 2000;23:260-5.
- [Google Scholar]
- 2019 ASCCP risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2020;24:102-31.
- [Google Scholar]
- Estimation of the duration of the preclinical phase of cervical adenocarcinoma suggests that there is ample opportunity for screening. Gynecol Oncol. 1999;75:55-61.
- [Google Scholar]
- Diagnosis and management of adenocarcinoma in situ A society of gynecologic oncology evidence-based review and recommendations. Obstet Gynecol. 2020;135:869-78.
- [Google Scholar]
- Risk of residual disease and invasive carcinoma in women treated for adenocarcinoma in situ of the cervix. Gynecol Oncol. 2013;129:513-6.
- [Google Scholar]
- Glandular lesions of the cervix on thin-layer Pap tests. Validity of cytologic criteria used in identifying significant lesions. Acta Cytol. 2004;48:372-9.
- [Google Scholar]
- Evaluation and significance of hyperchromatic crowded groups (HCG) in liquid-based paps. Cytojournal. 2007;4:2.
- [Google Scholar]
- Atypical glandular cells of undetermined significance (AGUS): Cytopathologic features, histopathologic results, and human papillomavirus DNA detection. Hum Pathol. 1999;30:816-25.
- [Google Scholar]
- HPV prevalence and genotypes in different histological subtypes of cervical adenocarcinoma, a worldwide analysis of 760 cases. Mod Pathol. 2014;27:1559067.
- [Google Scholar]
- Value of HPV-DNA test in women with cytological diagnosis of atypical glandular cells (AGC) Eur J Obstet Gynecol Reprod Biol. 2011;159:160-4.
- [Google Scholar]
- International endocervical adenocarcinoma criteria and classification (IECC): A new pathogenetic classification for invasive adenocarcinomas of the endocervix. Am J Surg Pathol. 2018;42:214-26.
- [Google Scholar]
- Papanicolaou tests associated with cervical mucosal endometriosis: An analysis of cellular features and comparison to endocervical adenocarcinoma in situ. Diagn Cytopathol. 2010;38:551-4.
- [Google Scholar]
- Cytomorphological features of hyperchromatic crowded groups in liquid-based cervicovaginal cytology: A single institutional experience. J Pathol Transl Med. 2019;53:393-8.
- [Google Scholar]
- Hyperchromatic crowded cell groups in gynaecological liquid-based cytology samples. Br J Biomed Sci. 2010;67:154-63. quiz 165
- [Google Scholar]
- Glandular lesions of the cervix. Validity of cytologic criteria used to differentiate reactive changes glandular intraepithelial lesions and adenocarcinoma. Acta Cytol. 1996;40:1127-35.
- [Google Scholar]
- Tubal metaplasia. A frequent potential pitfall in the cytologic diagnosis of endocervical glandular dysplasia on cervical smears. Acta Cytol. 1992;36:1-10.
- [Google Scholar]
- Microglandular endocervical hyperplasia and tubal metaplasia: Pitfalls in the diagnosis of adenocarcinoma on cervical smears. Diagn Cytopathol. 1997;16:168-73.
- [Google Scholar]
- Microglandular hyperplasia has a cytomorphological spectrum overlapping with atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesion (ASC-H) Diagn Cytopathol. 2004;30:57-61.
- [Google Scholar]
- Hyperchromatic Crowded Groups (HCGs) in the Pap Test In: Khalbuss W, Means M, eds. Gynecological and Breast Cytopathology Board Review and Self-Assessment. New York: Springer; 2013.
- [Google Scholar]
- Endocervical adenocarcinoma and its variants: Their morphology and differential diagnosis. Histopathology. 2002;41:185-207.
- [Google Scholar]
- Characteristic cytological findings of lobular endocervical glandular hyperplasia associated with adenocarcinoma of the uterine cervix. Acta Cytol. 2020;64:556-62.
- [Google Scholar]
- Glassy cell carcinoma of the uterine cervix. Cytologic features and expression of estrogen and progesterone receptors. Acta Cytol. 2000;44:551-6.
- [Google Scholar]
- Atypical endometrial cells and atypical glandular cells favor endometrial origin in Papanicolaou cervicovaginal tests: Correlation with histologic follow-up and abnormal clinical presentations. Cytojournal. 2014;11:29.
- [Google Scholar]
- Primary fallopian tubal transitional cell carcinoma with exfoliation of malignant cells in cervical Pap smear. Cytojournal. 2005;2:20.
- [Google Scholar]
- Cytologic patterns of cervical adenocarcinomas with emphasis on factors associated with underdiagnosis. Cancer Cytopathol. 2018;126:950-8.
- [Google Scholar]
- Squamous intraepithelial lesions (SIL: LSIL, HSIL, ASCUS, ASC-H, LSIL-H) of uterine cervix and Bethesda system. Cytojournal. 2021;18:16.
- [Google Scholar]
- Prevalence and significance of psammoma bodies in cervicovaginal smears in a cervical cancer screening program with emphasis on a case of primary bilateral ovarian psammocarcinoma. Cytojournal. 2008;5:7.
- [Google Scholar]
- The Bethesda System for Reporting Cervical Cytology (3rd ed). Berlin: Springer; 2015.
- [Google Scholar]
- ASC-H in Pap test--definitive categorization of cytomorphological spectrum. Cytojournal. 2006;3:14.
- [Google Scholar]
- Evaluation and significance of hyperchromatic crowded groups (HCG) in liquid-based paps. Cytojournal. 2007;4:2.
- [Google Scholar]








