Translate this page into:
Correlation study of thyroid nodule cytopathology and histopathology at two institutions in Jordan
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Fine-needle aspiration (FNA) plays a fundamental role in determining the appropriate management for patients presenting with thyroid nodules.
Aims:
The aims of this study are to evaluate thyroid FNA test performance parameters through a cytohistological correlation.
Materials and Methods:
A retrospective analysis of all thyroid FNAs received over a period of 18 months was carried out. The findings were compared to their subsequent definite diagnoses on surgical specimens as well as to their follow-up repeat FNA results. A total of 499 thyroid FNAs were collected and reviewed against The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC). The percentage of each diagnostic category was calculated, and the implied risk of malignancy was determined by comparing the cytology results to their definite diagnoses obtained on the resection specimens. Analytical procedures were performed using Microsoft Excel.
Results:
Out of 499 thyroid FNAs, a benign interpretation was found in 273 patients (54.7%), atypia of undetermined significance in 81 (16.2%), follicular neoplasm in 20 (4%), suspicious for malignancy in 36 (7.2%), malignant in 32 (6.4%) and were nondiagnostic in 57 patients (11.4%). Only 101 patients (20.2%) underwent surgical resection and 47 (9.4%) underwent a follow-up FNA. After cytohistological correlation, FNA test performance, calculated by excluding the inadequate and undetermined categories revealed test sensitivity, specificity, and diagnostic accuracy of 95.6%, 54.8%, and 78.9%, respectively. The positive predictive value was 75.4%, and the negative predictive value was 89.5%.
Conclusions:
Our results are comparable to those previously published figures. The rate of atypia of undetermined significance/follicular lesion of undetermined significance is higher than what is currently recommended in TBSRTC.
Keywords
Bethesda system for reporting thyroid cytopathology
cytohistological correlation
diagnostic test performance
fine needle aspiration
INTRODUCTION
Thyroid fine-needle aspiration (FNA) is reported to be a reliable and highly accurate test; however, review of the literature showed variability in the test performance among different studies.[1234] Technical factors including sampling errors, inadequate sampling and suboptimal preparation of the smears are some of the implicated reasons, in addition to interobserver variability in reporting thyroid smears, particularly in cases with ambiguous cytological features.[5] For that reasons, we aimed in this study to assess our FNA test performance as an initial diagnostic tool to guide the clinical management for patients with thyroid nodules.
MATERIALS AND METHODS
An Institutional Review Board (IRB)-approved retrospective analysis of all thyroid FNA received at a cancer center between January 2013 and June 2014 was conducted (IRB approval numbers: 15KHCC76 at the cancer center and 10/2016/814 at the university hospital). All subsequent surgical pathology and/or follow-up FNA cytology diagnoses for these patients, collected from the databases of both the cancer center and a university hospital from January 2013 to March 2016, were also included in the study.
For the majority of patients, thyroid FNA procedure was performed under ultrasound guidance by the diagnostic radiologists after detailed ultrasonographic examination. Thyroid smears were reported by board-certified pathologists using the six-tiered diagnostic categories proposed by The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) which includes: nondiagnostic or unsatisfactory (ND/UNS [Bethesda system diagnostic categories (BDC I)]), benign (BDC II), atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS [BDC III]), follicular neoplasm or suspicious for a follicular neoplasm (FN/SFN [BDC IV]), suspicious for malignancy (SM [BDC V]), and malignant (BDC VI).[56] All thyroid FNA were prepared by conventional methods with air-dried smears stained by a Romanowsky-type stain and/or Ethanol-fixed smears stained by Papanicolaou stain.
The distribution of thyroid FNA cases among different BDC was assessed by simple statistics. The thyroid FNA test performance as a screening test was assessed for its sensitivity, specificity, diagnostic accuracy, positive predictive value (PPV), negative predictive value (NPV), false-negative rate (FNR), and false-positive rate (FPR). The statistical analysis was performed based on two assumptions: The first one is to include AUS/FLUS (BDC III), in addition to other diagnostic categories (BDC II, IV, V, VI), to evaluate the test performance. The second is to recalculate the same parameters with excluding the AUS/FLUS (BDC III). True-positive group (TP) and false-positive group (FP) were defined as those who had BDC IV, V, and VI (± BDC III) and had a histological diagnosis on the resection specimens as malignant or benign, respectively. The use of the term “positive” is for statistical purposes only and does not indicate the presence of malignancy. On the other hand, the true-negative group (TN) included FNA cases with benign interpretation (BDC II), which were subsequently confirmed benign on the resection specimen, while the false-negative group (FN) included cases that were diagnosed as benign (BDC II) on FNA but confirmed histologically as malignant.
Based on the aforementioned assumptions, our test performance parameters were calculated according to these equations: Sensitivity (TP/[TP + FN]), specificity (TN/[FP + TN]), diagnostic accuracy ([TP + TN]/[TP + FP + FN + TN]), PPV (TP/[TP + FP]), NPV (TN/[FN + TN]), FPR (FP/[FP + TN]), and FNR (FN/[TP + FN]). In addition, the “real” FPR considering only malignant FNA interpretation; BDC VI, was calculated.
For the purpose of yielding accurate statistical results, patients with ND/UNS (BDC I) have been excluded from the statistical evaluation of the FNA test performance. However, those patients were evaluated separately to assess the risk of malignancy (ROM) among this category. Furthermore, patients with a benign FNA diagnosis (BDC II) who subsequently underwent surgical intervention for other reasons (e. g. clinically/radiologically suspicious or symptomatic lesion) and turned out to have an incidental papillary thyroid microcarcinomas (PMC) were not included in the false-negative group as the latter was not sampled by the FNA procedure. On the other hand, patients with AUS/FLUS, FN/SFN, SM, or malignant initial FNA diagnoses (BDC III, IV, V or VI, respectively) who were found to have PMC on the resection specimens were analyzed carefully in the context of the clinical and radiological findings to determine whether the latter was the sampled FNA lesion to decide in which group to be included.
RESULTS
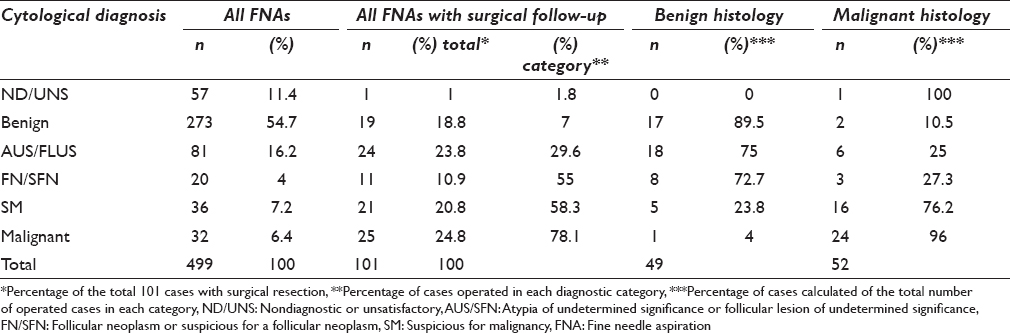
Between January 2013 and June 2014, 499 FNA was performed on 499 patients with thyroid lesion (s). There were 97 men and 402 women aged 15–93 years (mean age 52 years). The initial FNA cytology results were interpreted as benign (BDC II), in the majority of patients (273 patients [54.7%]), followed in terms of frequency by AUS/FLU (BDC III) in 81 patients (16.2%), SM (BDC V) in 36 patients (7.2%), malignant (BDC VI) in 32 patients (6.4%), while the diagnosis of FN/SFN (BDC IV) was the least common to be encountered in 20 patients (4%). Finally, 57 patients (11.4%) with ND/UNS thyroid FNA diagnosis (BDC I) were found [Table 1].

A definite histological diagnosis was available for 101 patients only (20.2%) in our study [Table 2].
The results of the FNA cytology were compared to their corresponding definite histological diagnoses which revealed the following: Of the 19 patients with benign FNA cytology (BDC II) who underwent surgical intervention, 11 patients (57.9%) were diagnosed histologically to have nonneoplastic lesions, two patients (10.5%) had a follicular adenoma, four patients (21.1%) had an incidental PMC, and two patients (10.5%) had malignant neoplasms (including one medullary carcinoma [Figure 1] and one follicular carcinoma).
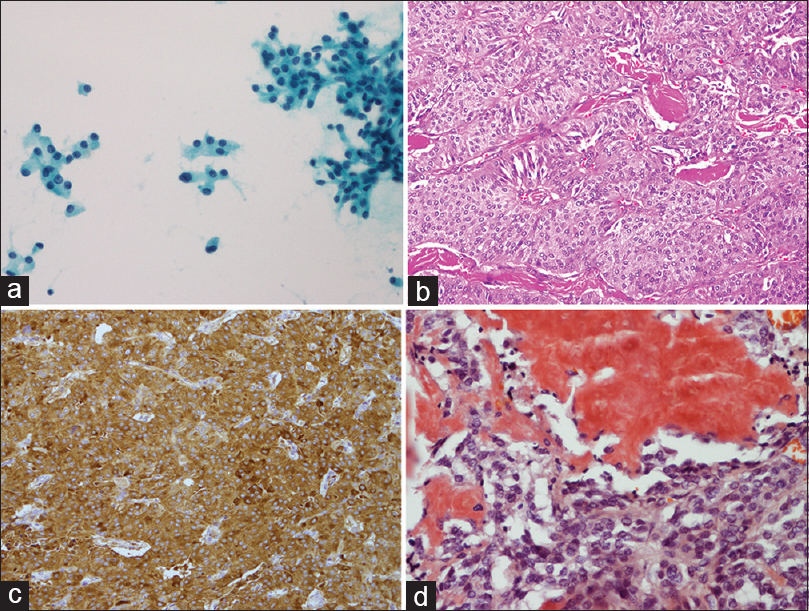
- Medullary thyroid carcinoma. (a) There is a loose group of cells with relatively uniform nuclei; occasional larger nuclei with prominent nucleoli are present. Tumor cells have plasmacytoid appearance (smear, Papanicolaou stain). (b) Low-power microscopic view showing highly vascularized tumor with trabecular pattern of growth and deposition of amyloid (hematoxylin-eosin, original magnifications ×200). (c) Immunostain for chromogranin. The tumor cells are uniformly reactive. (d) Amyloid stains orange-red with the Congo red stain
Of the 11 patients with FNA diagnosis of FN/SFN (BDC IV) who underwent surgical resection, three (27.3%) were found to have a multinodular goiter (MNG), five (45.5%) had a follicular adenoma [Figure 2], and three (27.3%) had a follicular carcinoma. Therefore, the yielded PPV for malignancy within this category is 27.3%.
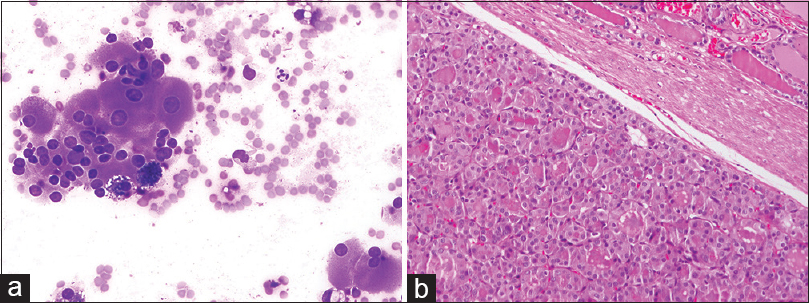
- Follicular adenoma, Hürthle cell type. (a) The aspirate consists of a pure population of Hürthle cells in small, crowded groups and as isolated cells in a background that lacks colloid and lymphocytes. The cells are highly variable in size and amount of cytoplasm (smear, Diff-Quik stain). (b) The tumor is completely surrounded by a thin fibrous capsule. Predominant microfollicular pattern, nuclei are round, uniform, and nonoverlapping. The component cells have deeply eosinophilic, granular cytoplasm (hematoxylin-eosin, original magnifications ×200)
In the diagnostic category of SM (BDC V), all of which were diagnosed as suspicious for papillary thyroid carcinoma (PTC), 16 out of 21 patients (76.2%) were confirmed to have PTC histologically including one with PMC which was confirmed by ultrasound guidance to be the targeted lesion for the FNA procedure. The other five patients (23.8%) within this category were found to have benign histology on surgical resection. Therefore, the PPV for malignancy within this category is 76%.
Twenty-five of 26 patients (96.2%) with malignant initial thyroid FNA diagnosis (BDC VI), all of them diagnosed as PTC showed concordant results on their corresponding resection specimens [Figure 3]. The remaining patient (3.8%) in this category was found to have MNG on surgical excision. Therefore, the PPV for malignancy within this category is 96.2%.
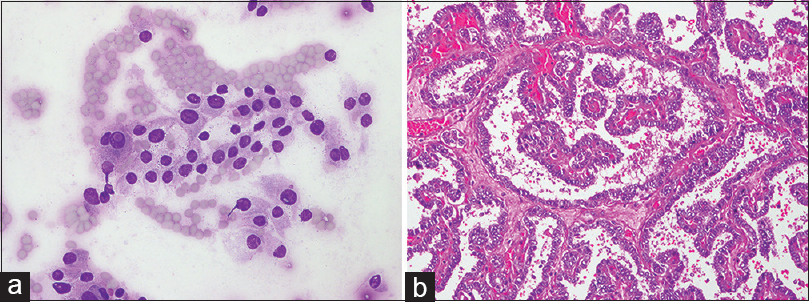
- Papillary thyroid carcinoma. (a) Intranuclear cytoplasmic pseudoinclusions and nuclear grooves are shown. The remaining nuclei show variation in size and shape (smear, Diff-Quik stain). (b) Complex branching papillary architecture. The papillae are covered by epithelium with disturbed polarity. Nuclear enlargement, overlapping, irregular nuclear contour, and clearing are seen (hematoxylin-eosin, original magnifications ×200)
Among the 24 patients who had thyroid FNA diagnosis of AUS/FLUS (BDC III) and underwent follow-up surgical resections, their final pathology revealed the following: 15 patients (62.5%) had nonneoplastic lesions, two (8.3%) had a follicular adenoma, four (16.7%) had a PTC, one (4.2%) had a poorly differentiated carcinoma, and 2 (8.3%) had a PMC. On review of the cytology and pathology slides for the last two patients in the context of clinical and radiological findings, we found that the PMC was sampled in only one of them by the FNA as it was the sole lesion present in the thyroid gland which was around 8 mm in greatest dimension. On the contrary, the other patient was found to have multiple large thyroid nodules which were sampled by FNA, while his 2 mm PMC was an incidental finding. Accordingly, for this category, the PPV for malignancy is 25%.
Only one patient with ND/UNS thyroid FNA cytology (BDC I) underwent surgical excision which revealed PTC.
Of note that, re-reviewing the slides of all histology cases encountered in this cohort to account for the recent update of TBSRTC did not reveal any tumor qualifying for reclassification as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP).[6]
Our thyroid FNA test performance as a screening test was evaluated by comparing the definite results obtained on the surgical resection specimens with the initial FNA diagnoses. The test parameters were calculated twice with and without including the AUS/FLUS category (BDC III). Accordingly, with including the AUS/FLUS (BDC III), our thyroid FNA test sensitivity, specificity and diagnostic accuracy are 96%, 34.7%, and 66%, respectively. The PPV is 60.5%, and the NPV is 89.5%. The FNR and FPR are 3.9% and 65.3%, respectively. On the other hand, excluding the AUS/FLUS (BDC III) revealed a test sensitivity, specificity, and diagnostic accuracy of 95.6%, 54.8%, and 78.9%, respectively. The PPV is 75.4%, and the NPV is 89.5%. The FNR and FPR are 4.4% and 45.2%, respectively. The “real” test FPR including only those patients with malignant FNA interpretation (BDC VI) is 5.6%.
Follow-up by repeating the FNA test after an appropriate interval was performed for 16 out of 254 patients (6.3%) with benign initial thyroid cytology (BDC II) who did not undergo surgical resection which confirmed the initial diagnosis in all of them.
Fourteen out of 57 patients (24.6%) with thyroid cytology diagnosis of AUS/FLUS (BDC III) who were not treated surgically underwent repeat FNA procedure. Of them, six (42.9%) were recategorized as benign (BDC II), one (7.1%) as FN/SFN (BDC IV), three (21.4%) as SM (BDC V), and two (14.3%) as malignant (BDC VI). The remaining two cases (14.3%) had persistent AUS/FLUS category (BDC III).
Fifteen patients with ND/UNS thyroid FNA cytology (BDC I) underwent repeat FNA which revealed a diagnostic benign result (BDC II) in nine out of 15 cases (60%), while it showed persistent inadequacy (BDC I) in six cases (40%).
DISCUSSION
FNA test plays an important role in the evaluation of thyroid nodules. Its result, in addition to other clinical and sonographic findings, provides a reliable and highly accurate guidance for patient's management. It has markedly reduced the number of unnecessary surgical intervention and increased the malignancy detection rate in patients undergoing thyroid surgery.[7] For clarity of communication between cytopathologists, treating physicians, and other health-care providers, TBSRTC was proposed in 2007 and revised in 2017 which mandates reporting of thyroid cytology according to their morphologic criteria into one of the six recommended diagnostic categories with provision of further subcategorization if appropriate.[5689] On the other hand, pathologic examination of thyroid resected specimens establishes the definite diagnosis and provides important information for risk stratification of cancer and postsurgical management.[310]
Since the inception of TBSRTC in 2007, many studies have been published to assess its utility in guiding the clinical management for patients with thyroid nodules.[411121314] Recently, a revised version of TBSRTC has been released taking into consideration the new data and developments in the field of thyroid pathology.[689] One of the modifications that have significant implication in predicting the ROM and influences patient's management is the reclassification of the noninvasive follicular variant of PTC as NIFTP. The latter is now considered as nonmalignant neoplasm, and therefore, the implied ROM published in the revised TBSRTC for each diagnostic category has been calculated two ways: when NIFTP is not considered a malignancy, and when NIFTP is still included among the “carcinoma.”[6]
We carried out this study to document our own experience and to assess our thyroid test performance by comparing the obtained results to published international data.
The benign FNA interpretation (BDC II) usually constitutes the majority of thyroid FNA cases, representing 60% to 70% of the total thyroid FNA.[5] Bongiovanni et al. in their meta-analysis review of eight published studies found that 59% of the cases were within this category.[4] In comparison, our study reveals 55% of the enrolled patients were found to have a benign cytological diagnosis. This figure is slightly lower than published data which is expected in view of the selection bias imposed by the fact that our cohort was obtained from a referral cancer center.
The implied ROM in the benign category (BDC II) is reported to be 0%–3%.[57] Bongiovanni et al. review showed that 10.4% of cases within this category underwent surgical intervention which revealed a 3.7% mean ROM, with a range of 1%–10%.[34] Our study showed that 7% of the cases within this category underwent surgery, with an associated ROM of 10.5% which is on the higher end of the reported range.
According to the American Thyroid Association guideline, a follow-up repeat FNA for cases with benign initial FNA interpretation (BDC II) may be done based on the clinical and radiological findings.[3] In our cohort, a repeat FNA test was performed for 16 patients with a benign initial cytological diagnosis (BDC II) which confirmed the initial results in all of them.
Regarding the diagnostic category of AUS/FLUS (BDC III), the original TBSRTC recommended a limit of 7% for its use; however, the revised version extended this limit to 10% with emphasis on making this interpretation as the last resort.[56] Furthermore, the newly published TBSRTC updates highlighted the issue of overestimating the ROM for this category if calculated based on the histologic follow-up alone. This is because of the selection bias as patients within this category will go for surgery if they have other suspicious clinical or sonographic features, abnormal repeat FNA cytology, or abnormal molecular testing results.[614] Another issue that was highlighted in the revised TBSRTC is the overestimation of the ROM for this category in the pre-NIFTP era (10%–30%) as this tumor constitutes a large proportion of “malignancy” hidden in this category. Considering NIFTP as a nonmalignant neoplasm reduces the ROM to 6%–18%.[6] For this category, persistent inconclusive result is expected in 20% of repeated FNA.[7]
Interestingly, Bongiovanni et al. found the percentage of this category to be 9.6% of all thyroid FNA with 39.2% of the cases surgically resected and a 15.9% ROM.[4] Our study revealed overrepresentation of this category (16.2%) with 29.6% of cases surgically resected and 25% ROM. This indicates that there is an overuse of this category in cases which might have been diagnosed as SM (BDC V).
Thyroid FNA with ND/UNS interpretation (BDC I), excluding samples composed exclusively of macrophages, ideally should be < 10% of thyroid FNA but reported in 2% to 20% in literature, with 5%–10% implied ROM.[61516] Repeating FNA procedure with ultrasound guidance is diagnostic in 50%–88% of cases; however, cases with persistent inadequacy mandate surgical excision as the ROM in the resected specimens is 10%.[17] Interestingly, Bongiovanni et al. found the average percentage of cases in this category to be 12.9%, ranging from 1.8% to 23.6% with 16.2% of them surgically resected and 16.8% ROM.[4] In our study, 11% of the cases were within this category with only one of them had a follow-up surgical intervention which revealed a PTC. However, follow-up by repeating FNA was performed for 15 cases, with persistent inadequacy (BDC I) in six cases (40%) and benign interpretation (BDC II) in the rest 9 cases (60%).
FNA procedure is considered as a screening test when it comes to FN/SFN diagnosis (BDC IV), leading to a diagnostic surgical procedure, usually lobectomy. The majority of resected nodules turn out to be follicular adenoma or non-neoplastic adenomatoid nodule of MNG. The implied ROM for this category is 25%–40% if NIFTP is considered as carcinoma and 10%–40% if it is considered as nonmalignant neoplasm.[6] Our study revealed 4% of our FNA cases are within this category. More than half of them (55%) had undergone diagnostic surgery, with a 27.3% ROM. This data are also comparable to that published in the review by Bongiovanni et al., wherein 10.1% of their cohort received this diagnosis, in which 69.7% underwent surgery with 26.1% ROM.[4]
Most of the resected nodules with FNA diagnosis of SM (BDC V) proved surgically to be papillary carcinoma (50%–75% in the pre-NIFTP era), and the rest are usually follicular adenomas.[615] The recent TBSRTC revision decreased the ROM to 45%–60% considering the NIFTP as nonmalignant neoplasm.[6] Our data showed 7.2% of the study cases are within this category with 58.3% of them treated surgically and 76.2% ROM. In comparison, this category was the least encountered in Bongiovanni et al. review (2.7%), in which 73.7% underwent surgical treatment with ROM of 75.2%.[4]
Conclusive features of malignancy are seen in approximately 3% to 7% of thyroid FNA with 97%–99% or 94%–96% implied ROM whether NIFTP is considered as a malignant neoplasm or not, respectively.[6] This is concordant with our results which showed 6.2% of the study sample received a malignant diagnosis, in which 78.1% were treated surgically, with a ROM of 96%. Bongiovanni et al. review revealed close figures with 5.4% of the FNA cases within this category, 74% of the cases surgically removed and 98.6% ROM.[4]
Table 3 shows a comparison of the implied ROM by 2017 TBSRTC, ROM in Bongiovanni et al. meta-analysis, and the current study ROM.[46]

The diagnostic performance of FNA test is defined by its sensitivity, specificity, diagnostic accuracy, PPV, NPV, FNR, and FPR. In a published paper by Gharib and Goellner in 1993, FNA diagnostic error and accuracy were calculated based on review of seven large series using four cytologic diagnostic categories (benign, suspicious, malignant, and nondiagnostic).[15] Their analysis revealed a FNR of 1% to 11% (mean 5%), a FPR of 1% to 8% (mean 3%), a sensitivity of 65% to 98% (mean 83%), and a specificity of 72% to 100% (mean 92%).[15] The data published by Bongiovanni et al. based on review of a large cohort reported using the TBSRTC 2007 (BDC II, IV, V, and VI) revealed a sensitivity, specificity and diagnostic accuracy of 97%, 50.7%, and 68.8%, respectively.[4]
Their PPV and NPV are 55.9% and 96.3%, respectively, and the FNR and FPR (for BDC VI only) are 3% and 0.5%, respectively.[4] Our test performance was evaluated two ways with and without AUS/FLUS (BDC III) and always excluding the ND/UNS (BDC I) from the calculation. Excluding AUS/FLUS (BDC III) revealed test sensitivity, specificity, and diagnostic accuracy are 96%, 34.7%, and 66%, respectively. The PPV is 60.5% and the NPV is 89.5%. The FNR and FPR are 3.9% and 65.3%, respectively. However, including the AUS/FLUS (BDC III) revealed test sensitivity, specificity, and diagnostic accuracy of 95.6%, 54.8%, and 78.9%, respectively, which are comparable to what is published in literature. FNR and FPR are 4.4% and 45.2%, respectively. The “real” test FPR including only those patients with malignant FNA interpretation (BDC VI) is 5.6%.
Although this study helped us to evaluate our FNA test performance in stratifying ROM in patients with thyroid nodules, its limitation include a small sample size of the patients who underwent surgical excision among all diagnostic categories. This is likely because many patients in our study were lost to follow-up, and they most probably underwent resection at institution different from our study center.
CONCLUSIONS/SUMMARY
A correct interpretation of the FNA cytology to evaluate thyroid nodules is critical yet challenging with variable results reported in literature regarding the test performance. Although our study indicates that we are overusing the diagnostic category of AUS/FLUS (BDC III), the ROM in this group seems to be reasonable compared to published studies. The overall test performance is acceptable which ensures confident clinical utilization of FNA as a reliable diagnostic/screening tool in patients with thyroid nodule.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The author (s) declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author.
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
NA carried out data collection at King Hussein Cancer Center, interpreted the results and performed the statistical analysis. MS carried out reviewing the slides of the FP and false negative cases and helped to draft the manuscript. LA and MH participated in the data collection from Jordan University Hospital and they helped in reviewing the drafted manuscript. All authors read and approved the final manuscript.
Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
This study was conducted with approval from IRB of all the institutions associated with this study as applicable. Authors take responsibility to maintain relevant documentation in this respect.
LIST OF ABBREVIATIONS (In alphabetic order)
-
AUS/FLUS – Atypia of undetermined significance or follicular lesion of undetermined significance
-
BDC – Bethesda system diagnostic categories
-
FN/SFN – Follicular neoplasm or suspicious for a follicular neoplasm
-
MNG – Multinodular goiter
-
ND/UNS – Nondiagnostic or unsatisfactory
-
NIFTP – Noninvasive follicular thyroid neoplasm with papillary-like nuclear features
-
PMC – Papillary thyroid microcarcinoma
-
SM – Suspicious for malignancy
-
TBSRTC- Thyroid Bethesda System for Reporting Thyroid Cytopathology.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- The significance of nontoxic thyroid nodules. Final report of a 15-year study of the incidence of thyroid malignancy. Ann Intern Med. 1968;69:537-40.
- [Google Scholar]
- Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest. 2009;39:699-706.
- [Google Scholar]
- 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1-33.
- [Google Scholar]
- The Bethesda system for reporting thyroid cytopathology: A meta-analysis. Acta Cytol. 2012;56:333-9.
- [Google Scholar]
- The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009;132:658-65.
- [Google Scholar]
- The 2017 Bethesda system for reporting thyroid cytopathology. J Am Soc Cytopathol. 2017;6:217-22.
- [Google Scholar]
- Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer. 2007;111:508-16.
- [Google Scholar]
- The Bethesda system for reporting thyroid cytopathology II. Acta Cytol. 2016;60:397-8.
- [Google Scholar]
- The Bethesda system for reporting thyroid cytopathology: Proposed modifications and updates for the second edition from an international panel. Acta Cytol. 2016;60:399-405.
- [Google Scholar]
- Update to the college of American pathologists reporting on thyroid carcinomas. Head Neck Pathol. 2009;3:86-93.
- [Google Scholar]
- Diagnostic accuracy of fine needle aspiration cytology in thyroid lesions. J Egypt Natl Canc Inst. 2012;24:63-70.
- [Google Scholar]
- A large multicenter correlation study of thyroid nodule cytopathology and histopathology. Thyroid. 2011;21:243-51.
- [Google Scholar]
- The Bethesda system for reporting thyroid fine needle aspirates: A cytologic study with histologic follow-up. J Cytol. 2013;30:94-9.
- [Google Scholar]
- Diagnosis of atypia/follicular lesion of undetermined significance: An institutional experience. Cytojournal. 2014;11:23.
- [Google Scholar]
- Fine-needle aspiration biopsy of the thyroid: An appraisal. Ann Intern Med. 1993;118:282-9.
- [Google Scholar]
- Usefulness of fine-needle aspiration in the diagnosis of thyroid carcinoma. Cancer Cytopathol. 2000;90:357-63.
- [Google Scholar]
- Non-diagnostic fine needle aspiration biopsy: A dilemma in management of nodular thyroid disease. Am Surg. 1993;59:415-9.
- [Google Scholar]








