Translate this page into:
Endometrial carcinoma with pleural fluid metastasis: A rare phenomenon
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 74-year-old female presented to the hospital with complaints of sudden-onset breathlessness for the past 1 day along with chest pain. The patient was a known diabetic (type 2 diabetes mellitus, on oral hypoglycemic drugs) and hypertensive. She was under treatment for right leg deep vein thrombosis for the past 6 months.
On detailed evaluation, the patient gave a history of hysterectomy with bilateral salpingo-oophorectomy 5 years back in view of carcinoma endometrium. Magnetic resonance imaging whole abdomen showed enlarged uterus with heterogeneous mass lesion occupying the endometrial cavity with possible myometrial invasion. Histopathological examination (HPE) revealed endometrioid carcinoma, Grade II, pT1N0Mx. She was given two cycles of brachytherapy. On follow-up after 2 years of surgery, she again presented to the hospital with pain in lower abdomen and burning micturition. Contrast-enhanced computed tomography (CECT) abdomen showed recurrence with evidence of heterogeneously enhancing mass along left internal iliac group of vessels causing external compression on adjacent lower ureter [Figure 1a]. Whole-body positron emission tomography-CT was done, which showed evidence of metastatic disease in the left internal iliac nodes and the right lower lobe of the lung with increased Fluorodeoxyglucose (FDG) uptake in these foci. An exploratory laparotomy along with excision of the mass was done. HPE suggested evidence of papillary serous carcinoma [Figure 2a and b] with positivity for estrogen receptor (ER) and progesterone receptor (PR). Further, she was referred for external beam radiotherapy to the pelvic region. She was doing well at the time of discharge.
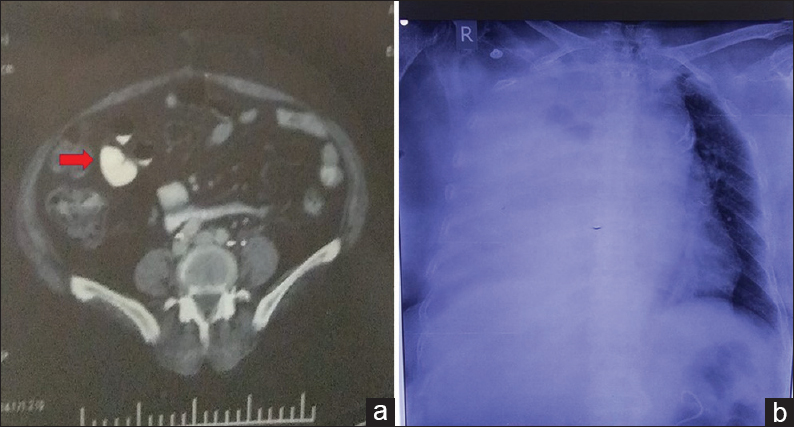
- (a) Contrast-enhanced computed tomography abdomen showing heterogeneously enhancing mass along left internal iliac group of vessels; (b) chest X-ray posteroanterior view with massive right-sided pleural effusion
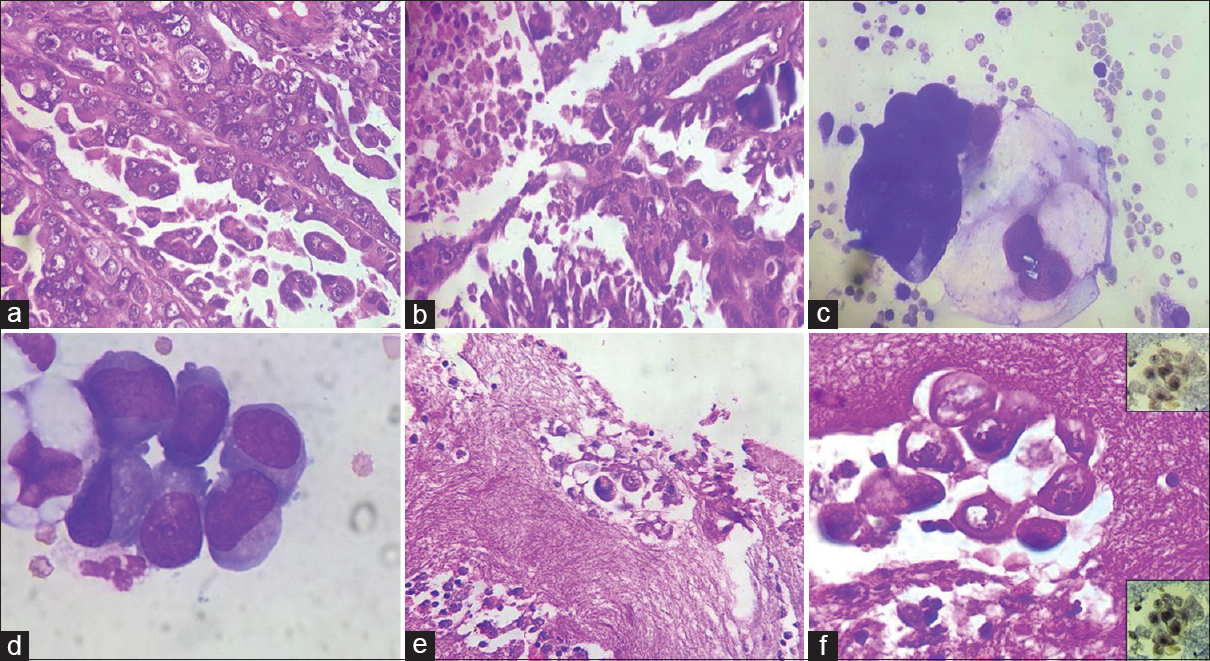
- (a and b) Sections showing papillary serous carcinoma (a, H and E, ×400) with necrosis and calcification (b, H and E, ×400); (c and d) smears from pleural fluid revealing cluster of atypical cells in three-dimensional cluster with tumor cells showing marked pleomorphism, high nucleocytoplasmic ratio, irregular nuclear membrane, hyperchromatic nuclei, prominent nucleoli, and moderate amount of pale cytoplasm (c, Giemsa, ×1000); few with cytoplasmic vacuolation (d, Giemsa, ×1000); (E and F) cell block showing focal cluster of malignant epithelial cells (H and E; e, ×400 and f, ×1000) and estrogen receptor and progesterone receptor positivity (f, right upper and lower insets)
At present, the patient was properly evaluated in view of sudden-onset breathlessness and chest pain. Her blood pressure was increased (140/90 mmHg). Ultrasound abdomen revealed mild hepatomegaly. Chest X-ray posteroanterior view was done, which showed evidence of massive right-sided pleural effusion [Figure 1b]. Complete blood count revealed leukocytosis (total leukocyte count: 24,200/μL), with the rest of the parameters being within normal limits. Her random blood sugar level was 202 mg/dL. The rest of the biochemical investigations were within normal limit.
The pleural fluid sample was sent for cytological examination. Smears prepared showed malignant epithelial cells arranged in three-dimensional cluster and singly scattered. Tumor cells showed marked pleomorphism, with high nucleocytoplasmic ratio, irregular nuclear membrane, hyperchromatic pleomorphic nuclei, prominent nucleoli, and mild-to-moderate amount of pale cytoplasm [Figure 2c and d]. Few cells showed eccentrically placed nuclei and cytoplasmic vacuolation [Figure 2d]. Also noted were occasional reactive mesothelial cells and scattered histiocytes. The cellblock section also showed tumor cells with ER and PR positivity [Figure 2e and f and inset]. Cytopathological features in conjunction with immunohistochemistry (IHC), radiological and clinical details of history of carcinoma endometrium, a diagnosis of metastatic adenocarcinoma was given.
There are a limited number of studies giving the exact incidence of pleural metastasis from tumors of the female genital tract. Although endometrial carcinoma (EC) is the most common invasive neoplasm of the female genital tract in the Western world, only 2%–4% of neoplasms are disseminated at the time of presentation.[123] Usually, the uterine cancer spreads to pelvic and para-aortic nodes by the lymphatic system or to distant organs by the hematogeneous system. In our case, distant metastases from serous papillary EC might have occurred through hematogeneous spread, and the detection of metastatic carcinoma was noted in the pleural effusion. In our case, neoplastic cells were also widespread throughout the lymphatic system, as in her last recurrence, pelvic lymph nodes were found to have metastatic deposits. In literature, the unusual sites of distant metastasis from EC are scalp, brain, heart, and paranasal sinuses.[345]
Thoracic metastases from gynecologic malignancies exhibit various imaging patterns. Metastases from endometrial cancer typically manifest as pulmonary nodules and lymphadenopathy, whereas ovarian cancer often manifests with small pleural effusions and subtle pleural nodules.[45] If a solitary lung lesion is found, it is always important to consider the possibility of primary lung cancer.
Histomorphology alone is sufficient to diagnose the metastatic deposits in majority of the cases. However, various diagnostic approaches are sometimes necessary to distinguish the primary tumor from the metastatic lesion. The ovarian or EC metastasis to pleura or lung must be differentiated from the mesothelioma. In such cases, the role of IHC becomes crucial. For example, BerEp4-defined surface glycoprotein is positive in carcinoma but is negative in mesothelioma. Calretinin, thrombomodulin, and cytokeratin 5 immunostaining, which is positive in mesothelioma, are negative in serous papillary carcinoma originating in the female genital tract. In our patient, carcinoma cells were identified in the pleural effusion with cells showing positivity for ER and PR and negativity for calretinin, confirming the metastatic deposits from EC.
The primary management of patients with a gynecological malignancy is usually protocol driven and is seldom controversial, but the management of patients with recurrent disease is often critical.[345] Hence, a multidisciplinary approach is required including surgery, chemotherapy, radiation therapy, or hormonal therapy.
To conclude, although the pleura are an uncommon site of widespread EC, we should always keep in mind the possibility of pleural spread from a female genital tract malignancy. Cytopathologic examination of pleural fluid and the presence of malignant cells help in recognition of recurrent disease and further guide the clinicians in starting the treatment accordingly.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
COMPETING INTEREST STATEMENT BY ALL THE AUTHORS
The authors declare that they have no competing interest.
AUTHORSHIP STATEMENTS BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE. Each author has participated sufficiently in work and takes public responsibility for appropriateness of content of this article.
ETHICS STATEMENT BY ALL AUTHORS
As this is a letter to editor, this case does not require approval from the Institutional Review Board.
LIST OF ABBREVIATIONS (In alphabetic order)
-
CECT - Contrast enhanced computed tomography
-
EC - Endometrial carcinoma
-
ER - Estrogen receptor
-
HPE - Histopathological examination
-
IHC - Immunohistochemistry
-
PR - Progesterone receptor.
REFERENCES
- Endometrial carcinoma with pleural metastasis: A case report. Acta Cytol. 2006;50:697-700.
- [Google Scholar]
- Treatment of pulmonary recurrences in patients with endometrial cancer. Gynecol Oncol. 2007;107:242-7.
- [Google Scholar]
- Thoracic manifestations of common nonpulmonary malignancies of women. Clin Chest Med. 2004;25:379-90.
- [Google Scholar]
- Comparative Z. ;22:122-6.







