Translate this page into:
Falling under the umbrella cells: A single institutional experience and literature review of urothelial carcinoma presenting as a primary pancreatic mass on endoscopic ultrasound-guided fine-needle aspiration
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Metastases to the pancreas are much less common than primary pancreatic lesions, and there are few reports in the literature of metastatic urothelial carcinoma (UC) found in the pancreas. We report two cases of metastatic UC mimicking a primary pancreatic lesion. Two female patients, aged 48 and 83 years, presented with isolated pancreatic lesions causing obstructive jaundice suspicious for pancreatic adenocarcinoma and underwent endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) with rapid on-site evaluation (ROSE). On cytopathology, the lesions were found to be UC, confirmed with immunohistochemical (IHC) staining. UC rarely metastasizes to the pancreas, and diagnosis through EUS-FNA can be challenging. However, the utilization of ROSE, dedicated cell block passes, and IHC have proved to be effective in obtaining this unusual pancreatic diagnosis by EUS-FNA.
Keywords
Endoscopic ultrasound-guided fine-needle aspiration
pancreatic metastases
rapid on-site evaluation
urothelial carcinoma
INTRODUCTION
Obstructive jaundice can be caused by isolated metastases to the pancreas, though it is more commonly associated with primary pancreatic neoplasms. Endoscopic ultrasound-guided fine-needle aspiration, a well-recognized diagnostic modality, can be pivotal in distinguishing metastatic neoplasms presenting as primary pancreatic lesions. In our review of the literature, there were only three other cases where urothelial carcinoma (UC) had been reported to have metastasized to the pancreas: Two diagnosed by EUS-FNA, and one at surgery after no definitive results were obtained from EUS-FNA. Here we present two cases of UC that presented with pancreatic masses and obstructive jaundice diagnosed with EUS-FNA, and review reports of previous cases in the literature.
CASE REPORTS
Case 1
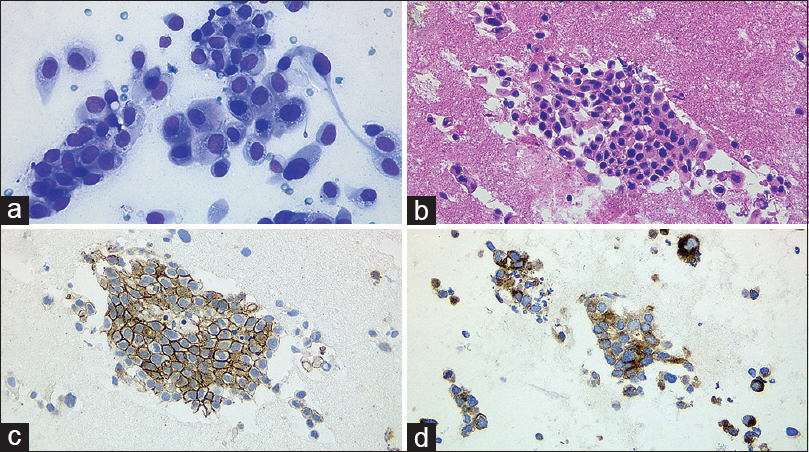
A 48-year-old woman was referred to our institution for endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) for confirmatory diagnosis of a suspected pancreatic mass causing obstructive jaundice. EUS using a linear echoendoscope (UCT180; Olympus America, Center Valley, Pennsylvania, USA) identified a hypoechoic mass in the peripancreatic region with poorly defined borders measuring 30 mm × 20 mm. Three passes were made by transduodenal FNA, with suction, using a 25-gauge needle: The first two for cytology and the third for cell block preparation. Microscopic analysis revealed many malignant cells with a high N:C ratio, irregular nuclear membrane, coarse irregular chromatin, and dense “squamoid” cytoplasm [Figure 1a and b]. An immunohistochemical (IHC) staining panel was performed, and the sample was found to be strongly positive for p63 and GATA3 [Figure 1c and d], proving a diagnosis of malignant urothelial carcinoma (UC) that had metastasized to the pancreas, mimicking the classic clinical picture of a primary pancreatic tumor. After clinical follow-up, this patient later underwent a bladder debulking procedure though follow-up positron emission tomography-computed tomography demonstrated new metastatic disease in the spine as well.

- Obviously malignant cells with high N:C ratios, anisocytosis, and anisonucleosis are observed at rapid on-site evaluation (Diff-Quik, ×400) (a), the cell block shows several malignant epithelial tissue fragments (H and E, ×200) (b), P63 and GATA3 are strongly positive (×200) (c and d) supporting a diagnosis of urothelial carcinoma
Case 2
An 83-year-old female with a medical history of hypertension presented with jaundice and abdominal pain to our institution while on vacation. On admission, she was found to have a bilirubin of 30 mg/dL. Subsequent biliary cannulation was unsuccessful due to a large obstructing mass. The patient underwent EUS utilizing a linear echoendoscope (UCT180; Olympus America, Center Valley, Pennsylvania, USA) and was found to have an irregular, hypoechoic, ill-defined mass in the head of the pancreas. Four passes without suction were made by transduodenal approach using a 25-gauge FNA needle: The first two for cytological on-site evaluation and the latter two passes dedicated for cell block preparation. Microscopically, the cells were overtly malignant with urothelial features [Figure 2a and b]. An extensive IHC panel was performed, and the sample was found to be strongly positive for thrombomodulin and uroplakin [Figure 2c and d], diagnostic of metastatic UC. This patient unfortunately died a month later from extensive disease.
- Malignant cells with nuclei more than four times the size of the background red blood cells were readily identifiable on cytology (Diff-Quik, 400) (a), cell block obtained from two dedicated passes shows numerous malignant cells surrounded by red blood cell (×400) (b), thrombomodulin and uroplakin stains (c and d) confirmed the diagnosis of urothelial carcinoma (×400)
DISCUSSION
Classically, obstructive jaundice is associated with primary tumors of the pancreas as isolated pancreatic metastases are very rare, accounting for <5% of pancreatic tumors.[1] With therapeutic advances, it is important to distinguish primary pancreatic malignancies, such as ductal adenocarcinoma or neuroendocrine tumor, from metastatic neoplasms. EUS-FNA, a well-recognized diagnostic modality, can be pivotal in distinguishing metastatic neoplasms presenting as primary pancreatic lesions. However, EUS-FNA performed with thin caliber needles has been shown to limit cell block yield and definitive diagnoses albeit these needles are often more flexible and easier to use in the pancreatic head and uncinate locations. One study has shown that the 25-gauge needle during EUS-FNA yielded diagnostic cell blocks only 81% of the time; this may have significant implications if a metastatic malignancy is suspected.[2] Despite using a thin (25-gauge) needle, sufficient diagnostic material was obtained in both cases at our institution by making dedicated passes for cell block (one pass with suction in the first case and two without suction in the second) which improved cellular yield and by utilizing rapid on-site evaluation (ROSE). ROSE has been shown to have concordance rate >98% with final cytopathology while considerably decreasing the number of repeat procedures performed,[34] further improving the utility of EUS-FNA for diagnosis.
As metastatic UC portends a poor prognosis, with a recent meta-analysis demonstrating a median survival of 68 weeks with chemotherapy,[5] it is important to ensure an accurate diagnosis and subsequently appropriate treatment. To this end, the definitive diagnoses of metastatic UC in the cases above were assisted by IHC studies. As seen in the first case, GATA3, a zinc finger transcription factor, has been shown to be very sensitive and highly expressed in low-grade, high-grade, and micropapillary variants of UC; likewise, p63 is expressed in most low-grade other UC but is not as reliable in other cancer variants.[6] Uroplakin is normally expressed in healthy urothelial cells and is useful as an ancillary study in UC although its expression tends to decrease as malignant transformation progresses; one study only found it expressed in 51.5% of invasive UC.[7] Likewise, thrombomodulin is also utilized in IHC for UC though it is also found in multiple types of tumors.[8]
Metastases to the pancreas are uncommon, and renal cell carcinoma is the most common tumor found as metastatic disease to the pancreas.[910] As stated above, it is very unusual for UC to metastasize to the pancreas, with only rare reports diagnosed by FNA in the literature in addition to those we reported [Table 1]. Canter et al. documented one case of micropapillary carcinoma of the bladder, a very aggressive variant of UC, which had appeared to have metastasized to the pancreas based on imaging, after the patient had presented for hematuria.[11] In this case, EUS-FNA of the pancreas demonstrated poorly differentiated carcinoma, though it could not be determined with certainty whether the tissue obtained originated from pancreatic or urothelial cells. However, during an exploratory laparotomy, intraoperative biopsies of the pancreatic mass and lymph nodes favored metastatic UC, and the patient was offered appropriate chemotherapy afterward.
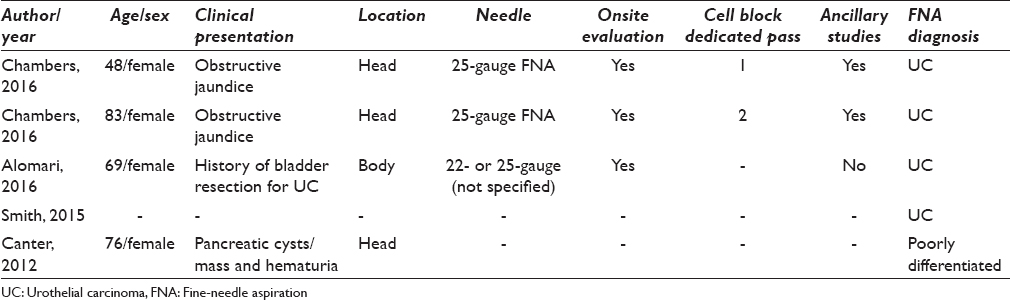
Last year, Smith et al. described only one case of UC metastasis to the pancreas between 2000 and 2014 at the Cleveland Clinic, out of the 2327 patients for whom pancreatic FNA was performed.[9] Of note, only 22 patients were determined to have metastatic disease to the pancreas in this study, further reinforcing the rarity of this presentation. In this study, however, it is not clear whether ROSE was utilized in the diagnosis.
Recently, Alomari et al. also only described one case of UC that had metastasized to the pancreas between 2005 and 2012, out of the 1346 patients who had undergone EUS-FNA with ROSE for pancreatic lesions at Yale University.[10] This patient was a 69-year-old female who apparently had a known prior history of malignancy and previous bladder resection and presented with a solitary lesion of the pancreatic body after a 2-year latent period. Due to prior resection, this patient had histological evidence of the primary malignancy which confirmed the cytological diagnosis, so no ancillary studies were performed.
SUMMARY
While making up a very small portion of pancreatic masses, the clinical presentations in these cases were similar to that of primary pancreatic lesions, which should give the clinician pause in the diagnosis of a lesion of the pancreas and keep the possibility, albeit rare, of metastatic disease in mind. The cases presented here were promptly diagnosed by EUS-FNA utilizing ROSE and dedicated passes for cell block preparation as well as ancillary studies, all of which enabled these patients to be offered timely and targeted therapy.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author. Each author has participated sufficiently in this work and takes public responsibility for appropriate portions of the content of this article.
MC performed the literature review and drafted the manuscript. KK performed the cytological preparation and provided images for the manuscript. SHM performed the diagnosis in the cases reported, conceived, coordinated, and helped draft the manuscript. All authors read and approved the final manuscript.
ETHICS STATEMENT BY ALL AUTHORS
Institutional Review Board approval has been obtained for this report.
LIST OF ABBREVIATIONS (In alphabetic order)
EUS-FNA: Endoscopic ultrasound-guided fine needle aspiration
IHC: Immunohistochemical
ROSE: Rapid on-site evaluation
UC: Urothelial carcinoma
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
ACKNOWLEDGMENTS
We would like to acknowledge Shyam Varadarajulu, MD, for acquisition of diagnostic material through EUS-FNA.
REFERENCES
- Secondary tumors of the pancreas: An analysis of a surgical and autopsy database and review of the literature. Virchows Arch. 2004;444:527-35.
- [Google Scholar]
- The 25-gauge EUS-FNA needle: Good for on-site but poor for off-site evaluation? Results of a randomized trial. Gastrointest Endosc. 2014;80:1056-63.
- [Google Scholar]
- Rapid on-site evaluation for endoscopic ultrasound-guided fine-needle biopsy of the pancreas decreases the incidence of repeat biopsy procedures. Cancer Cytopathol. 2013;121:518-24.
- [Google Scholar]
- Onsite cytopathology evaluation and ancillary studies beneficial in EUS-FNA of pancreatic, mediastinal, intra-abdominal, and submucosal lesions. Diagn Cytopathol. 2015;43:278-86.
- [Google Scholar]
- Third-line chemotherapy for metastatic urothelial cancer: A retrospective observational study. Medicine (Baltimore). 2015;94:e2297.
- [Google Scholar]
- The utility of p63, p40, and GATA-binding protein 3 immunohistochemistry in diagnosing micropapillary urothelial carcinoma. Hum Pathol. 2014;45:1824-9.
- [Google Scholar]
- Persistent uroplakin expression in advanced urothelial carcinomas: Implications in urothelial tumor progression and clinical outcome. Hum Pathol. 2007;38:1703-13.
- [Google Scholar]
- Immunohistochemical diagnosis of renal neoplasms. Arch Pathol Lab Med. 2011;135:92-109.
- [Google Scholar]
- Solid tumor metastases to the pancreas diagnosed by FNA: A single-institution experience and review of the literature. Cancer Cytopathol. 2015;123:347-55.
- [Google Scholar]
- Endoscopic ultrasound-guided fine-needle aspiration diagnosis of secondary tumors involving the pancreas: An institution's experience. Cytojournal. 2016;13:1.
- [Google Scholar]
- Clinical stage T1 micropapillary urothelial carcinoma presenting with metastasis to the pancreas. Urology. 2012;79:e9-10.
- [Google Scholar]








