Translate this page into:
Fine-needle aspiration cytology of eccrine hidrocystoma
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
We present a case of 59-year-old woman who presented with solitary small translucent cystic nodule measuring 1 cm in diameter on the left shoulder which had been present for 3 months. The patient denied any significant complaints associated with the lesion. The physical examination was noncontributory. The patient underwent FNA and scanty, clear fluid was aspirated. May Grunwald Giemsa (MGG) and Papanicolaou stained cytological smears and cytospin preparation showed scanty cellularity comprising small sheets of cuboidal cells against a proteinaceous background [Figures 1 and 2]. The cells were uniformly sized having round-to-oval nuclei with inconspicuous nucleoli and scant-to-moderate pink granular cytoplasm. There was no evidence of any cytological atypia and no papillary structures were seen in our smears. Cytological diagnosis of the cystic lesion with the possibility of benign adnexal neoplasm was rendered and patient was advised excision of the lesion for confirmation and subtyping.
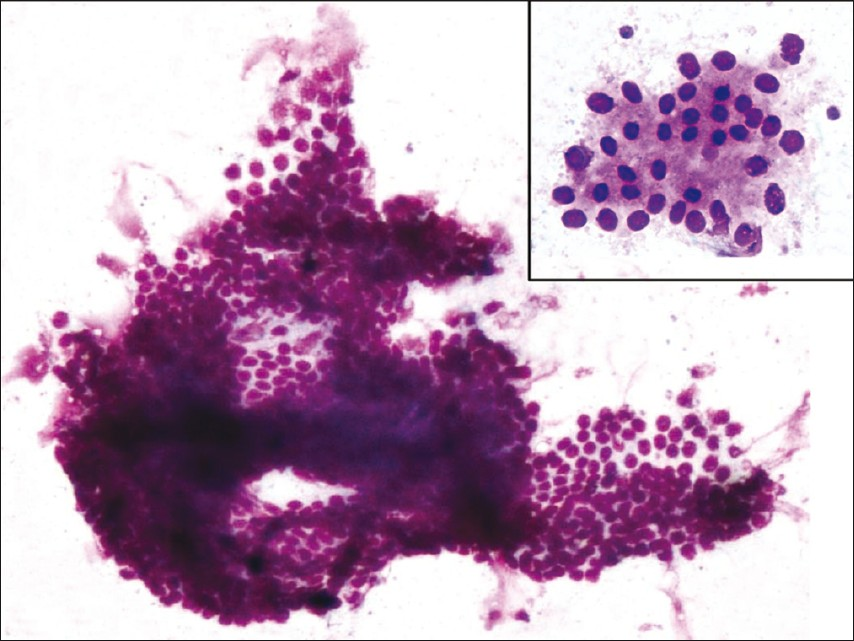
- Photomicrograph showing monolayered sheets of benign ductal cells (MGG, 10×) and inset showing loosely cohesive acini of benign ductal cells with moderate cytoplasm (MGG, 40×)
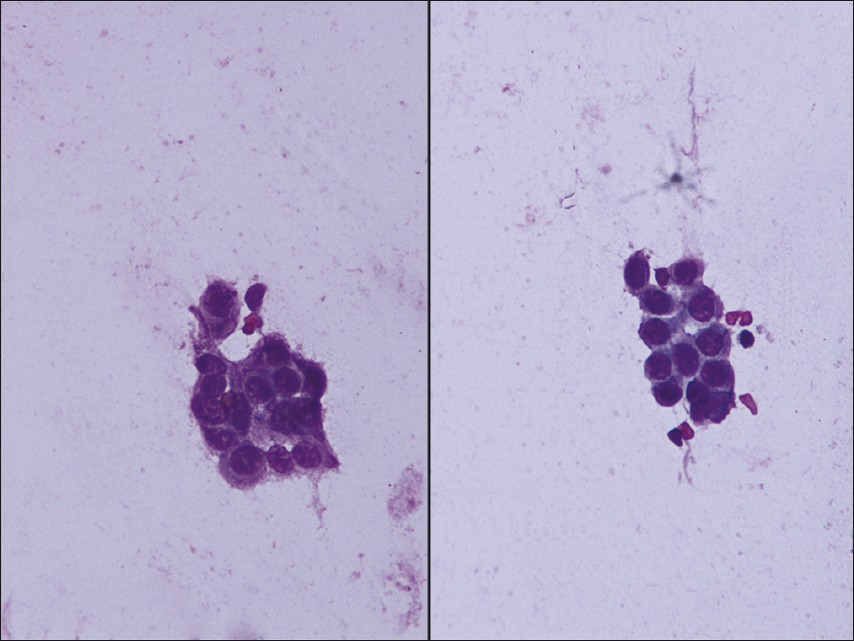
- Photomicrograph showing loosely cohesive cluster of benign ductal cells with moderate cytoplasm (Papanicolaou, 40×)
Subsequently, the excision biopsy was received as fibrofatty tissue measuring 1 × 0.6 × 0.2 cm. Hematoxylin and eosin stained sections revealed a dilated, cystic cavity in lower dermis and subcutis. The cyst wall was lined by a double layer of small cuboidal epithelium [Figure 3]. At places, a single layer of flattened epithelium with nuclei arranged parallel to the cyst wall was present. Small papillary projections extending into the cavity were also identified. Small eccrine ducts were present in close approximation to the cyst. Final diagnosis of eccrine hidrocystoma (EH) was made and the panel of immunostains comprising of CK7 and S100 was applied. The luminal cells stained positive for CK7 [Figure 4a] and abluminal cells showed positivity for S100 [Figure 4b], thus confirming diagnosis of solitary EH.
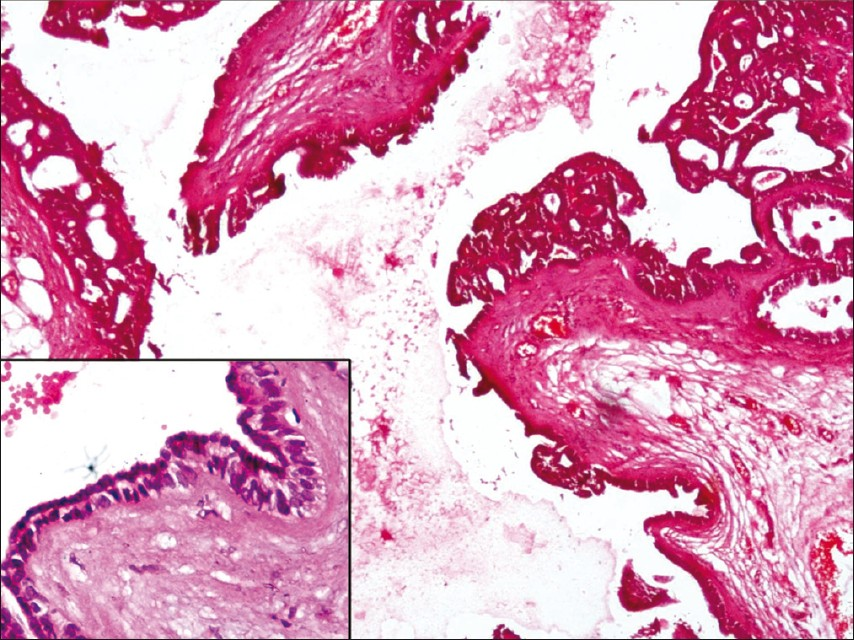
- Photomicrograph showing cystic spaces lined by a double layer of cuboidal epithelium thrown into small papillae at places (H and E, 10×) and inset showing cystic spaces lined by a double layer of cuboidal epithelium (H and E, 40×)
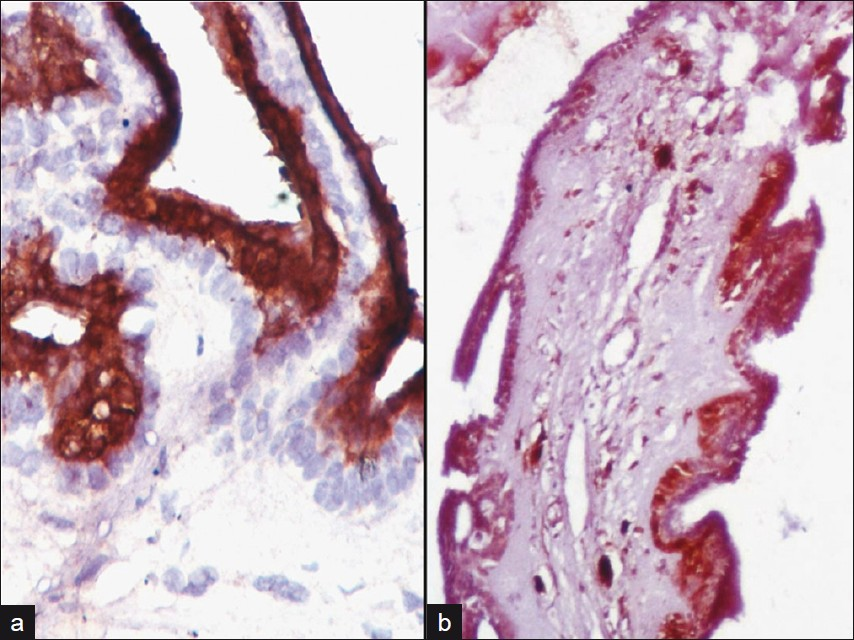
- (a) Photomicrograph showing cytoplasmic CK7 positivity in luminal cells (CK7, DAB, 40×), (b) Photomicrograph showing cytoplasmic S100 positivity in abluminal cells (S100, DAB, 10×)
Hidrocystomas are rare, benign cystic lesions of the skin. They can be either eccrine or apocrine and are found predominantly on the head and neck region. EH are small and tense thin-walled cysts ranging from 1 mm to 6 mm in diameter and can occur as single or multiple lesions. They are found predominantly in adult females and are located mostly on periorbital and malar regions.[12] In our case the lesion was located on the left shoulder, which is relatively a rare site for EH.
EH is currently classified in two major groups: the Smith type, which is more prevalent solitary type and Robinson or multiple types. The individual lesions of multiple types are similar to Smith type, except they are smaller.[3] EH usually result from dilation of cystic excretory eccrine glands due to retention of sweat and blockade and dilation of sweat duct.[1] Tokura et al.[4] suggested that solitary EH is derived from the secretory coil and multiple ones are derived from the duct.
Apocrine hidrocystoma (AH) is closest differential which needs to be ruled out before making final diagnosis of EH.[15–8] AH are also cystic lesions found mostly on the head and neck and arise from proliferation of apocrine gland. AH is usually solitary with diameter of 3-15 mm. AH also affects the same age group as EH. However, AH should be regarded as cystic adenoma rather than a retention cyst as the secretory cells do not appear flattened. Also, the cyst wall in AH is composed of inner layer of secretory, columnar epithelium which lies above the outer myoepithelial cell layer. At places, the secretory epithelium shows decapitation and papillary projections, which is not usually seen in EH. PAS positive granules are observed in AH unlike EH which are negative on PAS staining.[1] On IHC, solitary EH, typically shows CK7 positivity in luminal cells and S100 positivity in abluminal cells.[189] AH and multiple EH are negative on S100 staining. In contrast, AH shows positivity for GCDFP15 suggesting origin from glandular secretory spirals.[13]
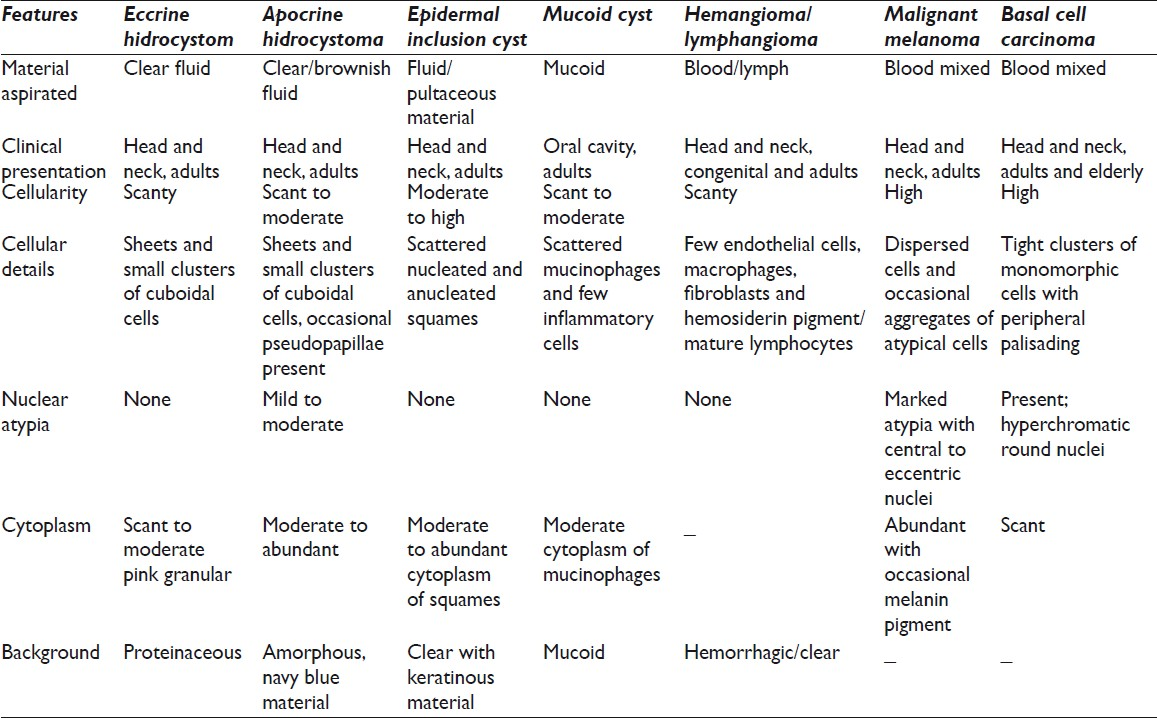
Clinically, other cystic lesions such as epidermal inclusion cyst, comedone, mucoid cyst, hemangioma, lymphangioma, and steatocystoma multiplex are considered in differential.[1] But all these lesions differ from EH both cytological [Table 1] and histologically. Very often, hidrocystomas (mostly AH) present as blue-black colored nodules and hence its differentiation from melanoma and basal cell carcinoma Table 1 is important.[10] We suggest that prior to excision biopsy needle aspiration can successfully establish diagnosis of EH and helps to rule out other common benign cystic and malignant skin conditions. Cytologic reports describing EH are relatively rare and few case reports that exist describe cytomorphology of AH only.[1112] Hence, cytopathologist needs to be aware of the FNA picture of this benign cystic lesion to be able to make a correct diagnosis.
We presented this paper with the aim to document cytologic picture of EH. In our case we report sheets and small groups of benign ductal cells with scant-to-moderate granular cytoplasm. No papillary structures were seen in our case. AH, on the other hand, show papillae and loosely cohesive cells with abundant cytoplasm suggesting secretory activity. Other benign cystic and malignant skin lesions can also be successfully ruled out on needle aspiration, thus guiding the clinician regarding extend of excision needed and further course of treatment. EH are completely benign and successfully treated on excision biopsy without any recurrence after the excision.[13–15]
To conclude, hidrocystomas are benign cystic lesions that typically occur in the facial region. Eccrine and apocrine hidrocystoma comprise two main groups and are closest mimics clinically. However, EH can be differentiated from apocrine counterpart on needle aspiration and also from other common benign cystic and malignant skin lesions [Table 1]. The cytopathologist should, therefore, keep in mind this entity while considering differentials for benign cystic lesions of skin. Histopathology and IHC may be used to further confirm the diagnosis.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
All the authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship. Each author has participated sufficiently in the work and take public responsibility for appropriate portions of the content of this article. ShS drafted the idea and manuscript. RA participated in drafting of manuscript along with technical help in immunostaining. SoS was involved in photography, case reporting and final proofreading of the manuscript, PG participated in searching the literature and photography. Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
This manuscript is a case description in form of a letter. Therefore, IRB approval was not mandatory.
EDITORIAL / PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through automatic online system.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2012/9/1/6/93283
REFERENCES
- Large pedunculated eccrine hidrocystoma: a case report. South Med J. 2010;103:262-4.
- [Google Scholar]
- Eccrine hidrocystoma in a child: an atypical presentation. Ann Dermatol. 2010;22:69-72.
- [Google Scholar]
- Apocrine cystadenoma, apocrine hidrocystoma, and eccrine hidrocystoma: three distinct tumors defined by expression of keratins and human milk fat globulin 1. J Cutan Pathol. 1997;24:249-55.
- [Google Scholar]
- Histochemical and immunohistochemical markers for human eccrine and apocrine sweat glands: an aid for histopathologic differentiation of sweat gland tumors. J Investig Dermatol Symp Proc. 2001;6:49-53.
- [Google Scholar]
- A reappraisal of eyelid eccrine and apocrine hidrocystomas: microanatomic and immunohistochemical studies of 40 lesions. Am J Ophthalmol. 2011;151:358-74.e2.
- [Google Scholar]
- Pigmented hidrocystoma of the eccrine secretory coil in the vulva: clinicopathologic, immunohistochemical and ultrastructural studies. J Cutan Pathol. 1999;26:145-9.
- [Google Scholar]
- Giant eccrine hidrocystoma presenting with unilateral ptosis and epiphora. Int Ophthalmol. 2008;28:429-31.
- [Google Scholar]
- Fine-needle aspiration of apocrine hidrocystoma- A potential mimic of papillary neoplasms metastasizing to the skin. Diagn Cytopathol. 2004;30:275-9.
- [Google Scholar]
- Hidrocystoma: surgical management of cystic lesions of the eyelid. An Bras Dermatol. 2010;85:368-71.
- [Google Scholar]
- Multilocular eyelid hidrocystoma: an anatomical and clinical observation. J Fr Ophtalmol. 2003;26:106-9.
- [Google Scholar]







