Translate this page into:
Fine-needle aspiration of bilateral small round blue cell tumors in neck in a 65-year-old man: Significance of a wider differential
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
65-year-old man with progressive bilateral jaw and neck swelling for 1 year. The bilateral neck masses yielded hypercellular aspirates. The monotonous cells were arranged in small clusters and small rosettes with uniformly round nuclei, smooth nuclear contours, coarse - clumped chromatin, and scant delicate cytoplasm. Many groups of cells showed significant nuclear molding. Mitotic figures and necrosis were not readily identified [Figure 1a–e].
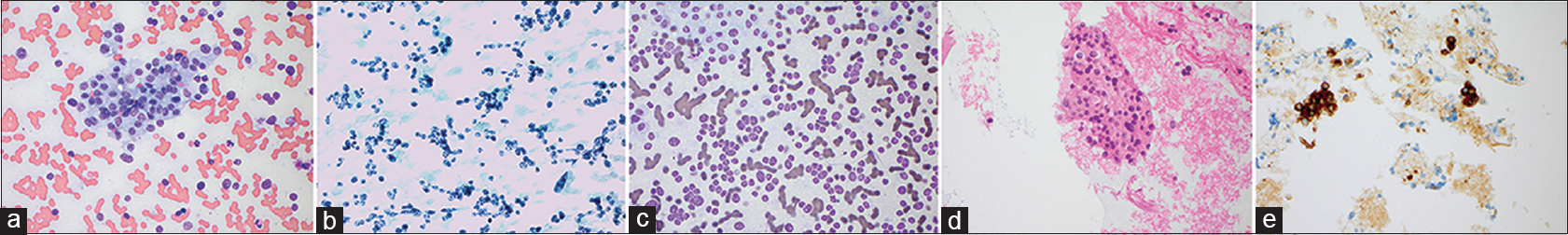
- (a) Monotonous cells were arranged in small rosettes and clusters, as well as dispersed single cells (Diff-Quik, ×400). (b) The tumor cells have round to avoid nuclei with clumped chromatin and scant, delicate cytoplasm (Pap stain, ×400). (c) Many groups of cells showed significant nuclear molding (Diff-Quik, ×400). (d) Cell block was cellular with monotonous cells similar to those seen in the smears (H and E, ×400). (e) Cell block sections showed tumor cell immunoreactivity for synaptophysin (×400)
The tumor cells were immunoreactive for synaptophysin and chromogranin (focally) with non- immunoreactivity for cytokeratin AE1/AE3 and CD45.
QUIZ QUESTION
Q1. What is your interpretation?
-
Small cell carcinoma
-
Diffuse large B-cell lymphoma
-
Human papillomavirus-associated squamous cell carcinoma
-
Olfactory neuroblastoma.
ANSWER
Q1 (d) Olfactory neuroblastoma.
Based on the tumor's cytologic appearance and immunohistochemical profile, as well as the patient's past medical history of a carcinoma in the nasal cavity, a diagnosis of recurrent/metastatic olfactory neuroblastoma was rendered on all specimens obtained.
FOLLOW-UP OF THE PRESENT CASE
The patient had equivocal history of “carcinoma” in the left nasal cavity treated 10 years ago with craniofacial resection, left eye exenteration, and radiation therapy. Follow-up magnetic resonance imaging performed 6 years ago was reportedly negative for recurrence. The patient was lost to follow-up until the current presentation. Ultrasound examination showed a 4.0 cm × 3.8 cm × 2.5 cm complex, right neck mass-posterior and inferior to the ear. 4.0 cm × 3.5 cm ovoid, mobile, Level IB/IIA left neck mass was also present in addition to bilateral, multiple, relatively enlarged cervical lymph nodes.
A subsequent ethmoid sinus biopsy showed similar findings. The patient underwent salvage radiation therapy but presented to the hospital with progressive disease. The patient eventually elected for comfort measures only and was transferred to hospice care 10 months after tumor recurrence (nearly 11 years after initial diagnosis) and expired soon after.
ADDITIONAL QUIZ QUESTION
Q2. What is the genetic abnormality found in NUT midline carcinomas?
-
13q14 (FOXO1) rearrangement
-
(15;19), BRD4-NUT gene fusion
-
EWSR1 rearrangements
-
t(X;18), SYT-SSX1.
Q3. What are the benefits of rapid on-site evaluation (ROSE) of fine needle aspiration samples?
-
Increase tumor yield
-
Assist in efficient triage for ancillary testing
-
Give a preliminary diagnosis
-
A and B
ANSWERS TO ADDITIONAL QUIZ QUESTIONS
Q2: B; Q3: D.
BRIEF REVIEW OF THIS TOPIC
Small round blue cell tumors (SRBCTs) are characterized by generally uniform small- to medium-sized, round, and relatively undifferentiated cells with hyperchromatic nuclei and a high nuclear to cytoplasmic ratio. FNA of SRBCTs typically leads to highly cellular smears that are amenable to ancillary testing techniques.
An initial branch point we used in this case of a SRBCT was the age of the patient, as well as the bilateral locations of the tumor. Tumor masses in the neck are more commonly metastatic in nature, highlighting the importance of the patient's past medical history. Because of the patient's history of a solitary tumor in the nasal cavity and these subsequent bilateral neck masses, it was more likely for the neck masses to represent metastasis from a nasopharyngeal or sinonasal primary cancer.[1]
Olfactory neuroblastoma/esthesioneuroblastoma is primarily found in the submucosa of the sinonasal cavity and may present as a metastatic lesion in the head/neck. Smears are hypercellular, with monotonous cells arranged in small rosettes, sheets, and singly. As with neuroendocrine tumors and Merkel cell carcinoma, the cells have small round nuclei, “salt-and-pepper” chromatin, small to inconspicuous nucleoli, and nuclear molding. Necrosis, pleomorphism, and high mitotic activity may be absent in lower grade lesions, as in case 3 above. Tumor cells are positive for synaptophysin and chromogranin and negative for epithelial markers including cytokeratins and epithelial membrane antigen. The neurofibrillary cell processes that surround tumor cells may present as fibrillary background material on fine needle aspiration cytology (FNAC) smears and stain for S100.[2]
NUT midline carcinoma (NMC) is a poorly-differentiated carcinoma originating in midline locations. The tumor has a particular translocation t(15;19), most commonly resulting in the BRD4-NUT fusion gene.[3] While the cytogenetic presentation is unique, the cytologic appearance is not. Smears show monomorphic cells with high nuclear: cytoplasmic ratios, scant cytoplasm, and prominent nucleoli. Across cases of confirmed NMC, tumor cells have ranged from undifferentiated to well differentiated with keratinization. Diagnosis of NMC has historically been made by demonstration of NUT rearrangement through FISH. An immunohistochemical antibody exists but is not widely available.
Metastatic melanoma must always remain in the differential for round blue cell tumors of the head and neck, as it frequently presents after initial resection or as the first sign of malignancy. Melanoma cells are medium- to large-sized and can have epithelioid or round cell appearance, with prominent nucleoli and pleomorphic or irregular nuclei. The cells can be arranged in many forms, either as cohesive groups or as dispersed single cells. Melanoma cells can variably express S100, Melan-A (MART-1), HMB45, and SOX10. Use of a wide panel of as many markers as possible, along with a pan-cytokeratin cocktail and CD45, is essential when attempting to rule in or rule out metastatic melanoma in a patient with no prior history of melanoma.[4]
Although less common, metastatic or primary sarcomas can present as solitary neck masses consisting of small round blue cells on FNAC. In young- to middle-aged adults, the differential diagnosis includes synovial sarcoma, desmoplastic small round cell tumors, small cell osteosarcoma, mesenchymal chondrosarcoma, and round cell liposarcomas.[15] A prior history is especially helpful in this regard, as metastatic lesions may represent a higher grade or dedifferentiated recurrence of the sarcoma.
SUMMARY OF QUIZ CASES
Over the course of three quiz cases, we have shown three cases of round cell tumors that presented initially for FNAC, in which the diagnosis and workup significantly altered management and treatment decisions.
The first quiz case, published in December 2017[6], discussed the diagnostic considerations of a unilateral neck mass in the pediatric patient. The eventual diagnosis of rhabdomyosarcoma was aided by triage of the subsequent surgical pathology specimen for cytogenetic and immunohitochemical studies. The second quiz case, published in January 2018[7], showed the evaluation of a unilateral neck mass in an immunosuppressed older adult patient. The use of flow cytometry at the time of FNA narrowed the diagnostic focus and eliminated lymphoma as a possibility. The current quiz case changes the clinical scenario to bilateral neck masses in an older adult patient with a significant but vague medical history. The current case highlight the importance of obtaining medical history even prior to FNA assessment. Taken together, this series illustrates the wide and varying diagnoses and patient population that can present as small round blue cell tumors in the head and neck.
As with all cases of FNAC, sampling tumor limits the ability to definitively diagnose SRBCTs based on microscopic examination alone. While some SRBCTs can display helpful or characteristic features such as rosette formation in neuroblastoma, many SRBCTs can exhibit pseudorosettes. In small biopsies and FNAC, architectural features may not be present in a limited sampling of the tumor. Although there may be temptation or pressure to arrive at a definitive diagnosis, cytopathologists must exercise caution when working with limited material.
A multimodal approach is key when working up SRBCTs. The workup includes correlation with clinical history and radiology findings and the use of immunohistochemical studies, molecular studies, flow cytometry, and cytogenetic karyotyping and/or fluorescence in situ hybridization (FISH) cytogenetic studies when indicated. A multidisciplinary approach with close communication with clinical colleagues and integration of multifaceted data is necessary to arrive at the correct diagnosis.
An important final consideration in FNAC evaluation of SRBCTs is the use of rapid on-site evaluation (ROSE) of the FNA sample. Whether it is the pathologist or the radiologist obtaining the sample, ROSE can increase tumor yield and assist in efficient triaging for ancillary testing. Given the ever-increasing possible ancillary testing available to the pathologist, thoughtful specimen allocation can mitigate unnecessary testing or need for repeat sampling.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
For all authors, the authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
SC carried out literature review, coordinated submission, and drafted and edited the manuscript.
SH collected clinical cases, performed additional literature review, and edited the manuscript.
DYL collected clinical cases and edited the manuscript.
RCM photomicrographs and drafted the manuscript.
MVL collected cases, and helped draft and edit the manuscript.
NAM conceived of the quiz case, collected clinical cases, performed additional literature review, and edited the manuscript.
All authors read and approved the final manuscript.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from Institutional Review Board (IRB) (or its equivalent).
LIST OF ABBREVIATIONS (In alphabetic Order)
FISH - Fluorescence in situ hybridization
FNA – Fine-needle aspiration
NUT – Midline Carcinoma
NUT – Nuclear protein in testis
PNET - Primitive neuroectodermal tumor
ROSE - Rapid on-site evaluation
SRBCT - Small round blue cell tumor.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted through automatic online system.
REFERENCES
- Approach to the diagnosis of soft tissue tumors. In: Goldblum JR, Weiss SW, Folpe AL, eds. Enzinger and Weiss's Soft Tissue Tumors (5th ed). New York: Elsevier; 2013.
- [Google Scholar]
- Sinonasal small round blue cell tumors: An approach to diagnosis. Semin Diagn Pathol. 2016;33:91-103.
- [Google Scholar]
- Cytology: Diagnostic Principals and Clinical Correlates. (4th ed). New York: Elsevier; 2014.
- [Google Scholar]
- Fine-needle aspiration of a right neck mass in a 10-year-old boy: Diagnostic clues and workup for tumors with small round blue cells. CytoJournal. 2017;14:30.
- [Google Scholar]
- Fine-needle aspiration of a slowly enlarging neck mass in a 61-year-old woman: An interesting adult blue cell tumor in an unusual location. CytoJournal. 2018;15:1.
- [Google Scholar]







