Translate this page into:
High risk human papillomavirus type 16 and 18 infection in the cervical lesions of women with epithelial cell abnormality in Pap smear: A cytohistomorphologic association in Bangladeshi women
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The aim of this study was to find out the extent of high-risk human papillomavirus (hrHPV) type 16/18 infection in the cervical tissue of women with epithelial cell abnormality in Pap smear and to establish an association between hrHPV type 16/18 infection and cytohistomorphology.
Materials and Methods:
A cross-sectional descriptive study was carried out in 1699 patients who went through Pap smear examination. Prevalence of epithelial cell abnormality was calculated. Forty eight of these women underwent routine histopathology and 47 were evaluated for human papillomavirus (HPV) type 16/18 by polymerase chain reaction assay.
Results:
Total 139 women revealed epithelial cell abnormality. Histopathology showed simple inflammation to malignancy. HPV type 16/18 infection was detected in 40.42% (19/47) of the patients. Individually type 16 and 18 were positive in 7 (14.9%) cases each and dual infection with type 16 and 18 were seen in 5 (10.6%) cases. While cervical intraepithelial neoplasia grade 1 (CIN 1) and < CIN 1 lesions showed 18.75% (3 out of 16) and 35% (7 out of 20) positivity respectively, ≥CIN 2 lesions revealed positivity of 81.82% (9 out of 11). Eighty percent HPV 16/18 positivity was seen in women of < 30 years of age.
Conclusion:
The findings of this study will contribute to HPV 16/18 knowledge in Bangladesh that will be useful in assessing the success of current vaccines with limited type spectra and augmenting cervical cancer screening strategies.
Keywords
Cervical cancer
human papillomavirus
Pap smear
INTRODUCTION
Cervical cancer is an important global public health problem and approximately 80% of the cases are diagnosed in developing countries.[1] Human papillomavirus (HPV) is found in virtually 100% of invasive cervical cancer cases and over 60% of cervical intraepithelial neoplasia (CIN).[23] More than 200 types have been reported and 16 types that are commonly isolated from malignant lesions are classified as high risk (hr) types.[4] While the probability of tumorigenesis is different among various hrHPV types, 16 and 18 are more strongly associated with invasive cancer.[5] Various polymerase chain reaction (PCR) based studies have been carried out in different countries for elucidating the clinical implications of HPV infection and the role of HPV in the pathogenesis of cervical carcinoma using cervical tissues and HPV deoxyribonucleic acid (DNA) can be detected successfully in formalin fixed paraffin embedded (FFPE) archival specimens using PCR-based methods.[6–8]
Clinical trials to test the efficacy of prophylactic vaccines targeting two oncogenic HPV types, 16 and 18 has created an immediate need for genotyping of tissues to co-localize HPV infections and their associated lesions. Moreover, as prophylactic vaccines are expected to provide minimal protection against untargeted types, elucidating the attribution of cervical lesions to HPV types can provide insights in vaccine trials. Hence, co-localization of hrHPV type 16/18 infection and cervical lesion in women with abnormal Pap smear results may help in assessing the effectiveness of current prophylactic vaccines with limited type specific spectra.
Bangladesh is a densely populated country. Routine screening of cervical cancer is yet to be developed here and there is little awareness among the general population, health care professionals and policy makers about cervical cancer prevention. Due to lack of an organized cervical cancer screening system and low screening coverage, immunization against the most prevalent hrHPV types affecting the country may be an efficient means to long term prevention. In a hospital based study of Bangladesh, 96.7% of 120 cervical cancer cases, 83.3% of 36 cases of CIN 2/3 cases and 4.1% of 120 control women were HPV positive by hybridization.[9] However, up until now HPV type 16/18 genotype distribution in the cervical lesions of Bangladeshi women is uncertain.[10]
The present study was designed to determine the extent to which hrHPV type 16 and 18 infection was present in the cervical tissues of women with abnormal cytology at a tertiary hospital in Bangladesh and to establish an association between hrHPV 16 and 18 infection and cyto-histomorphology.
MATERIALS AND METHODS
Study setting and specimen collection
The study was carried out in the Department of Pathology of Chittagong Medical College, Chittagong, Bangladesh. A total of 1699 Pap smear slides were received from the Gynae Outpatient Department (GOPD) from February to September, 2010. All these women visited GOPD with various gynecological complaints and not for routine cervical cancer screening purpose. Cervical sample collection and smear preparation was performed at GOPD and Pap staining of the smeared slide, microscopic examination and reporting was done at the Department of Pathology, Chittagong Medical College.
Cytological reporting was done according to the 2001 revised Bethesda System.[11] Epithelial cell abnormality was detected in 139 cases and 48 of them had routine histopathological examination performed. One of the women was advised to undergo repeat biopsy due to tissue inadequacy and as she did not return she was excluded from further study. For the purpose of this study following histopathological categories were used: < CIN 1, CIN 1, ≥CIN 2 (including carcinoma). All cytopathological and histopathological slides were examined and reported by at least three expert pathologists.
DNA extraction and PCR assay
DNA was extracted from 47 FFPE tissue samples with the commercial Extra-DNA-Sorb-B tissue kit (Sacace Biotechnologies Srl 44 Scalabrini Str, 22100 Como, Italy) following the manufacturer’s protocol. The extracted DNA was 50 μl for each sample and stored at −20°C for further analysis.
Multiplex PCR was done with HPV 16/18 Real-TM Quant kit (Sacace Biotechnologies Srl 44 Scalabrini Str, 22100 Como, Italy). The target region was E7 gene. PCR amplification was carried out in 25 μl reaction volume using the Real Time Thermal Cycler (model: RotorGene 6000, Corbett Research, Australia). Thermal cycling consisted of a preliminary hold temperature of 95°C for 15 min, followed by 45 cycles comprising 15 s at 95°C and 35 s at 60°C. Negative control, positive control and internal control were supplied with the kit and used according to the protocol. The β-globin gene was used as internal control. Results were interpreted with software Rotor Gene 6000 version 1.7 Build 34 (Corbett Research, Mortlake, New South Wales, Australia). PCR-safe precautions were taken.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) (SPSS Inc., Wacker Drive, Chicago, US) version 18.0 for windows. To verify the association between HPV 16/18 infection and cervical lesion of women with epithelial cell abnormality, Chi-square test (χ2 test) was performed and P < 0.05 was considered statistically significant.
RESULTS
Epithelial cell abnormality was detected in a total of 139 (8.18%) cases. Age range of these women was 21-70 years (mean age 41.97) with 53.96% (75 out of 139) being < 45 years and 46.04% (64 out of 139) being ≥45 years of age [Table 1].
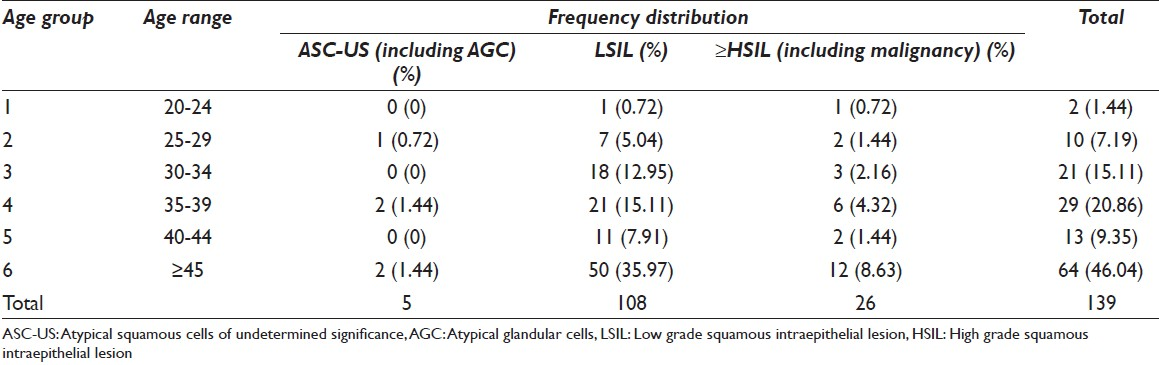
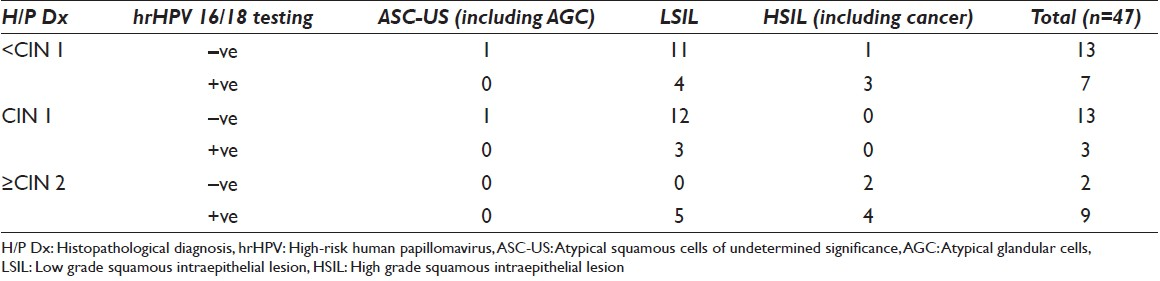
Routine histopathology revealed a wide range of diagnosis from simple inflammation to CIN 3 lesions and frank malignancy [Table 2]. PCR analysis of 47 cervical tissue specimens revealed HPV 16/18 infection in a total of 19 (40.4%) cases while 28 (59.6%) cases turned out to be HPV 16/18 negative. Among the hrHPV 16/18 positive women, 4 out of 5 cases (80%; 4/5) were of 20-29 years, 7 out of 25 cases (28%; 7/25) were of 30-44 years and 8 out of 17 cases (47.06%; 8/17) were of ≥45 years of age [Table 3]. Individually type 16 and type 18 were positive in 7 (14.9%) cases each and dual infection with type 16 and 18 were seen in 5 (10.6%) cases [Figure 1; Table 4 and Table 5].
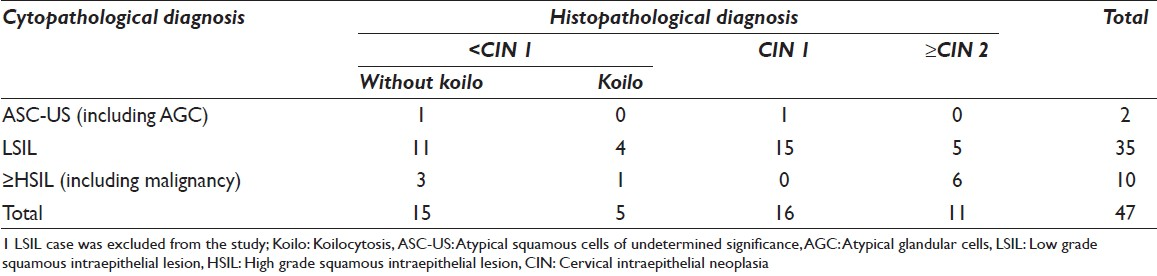



While < CIN 1 and CIN 1 lesions showed 35% (7 out of 20) and 18.75% (3 out of 13) positivity, ≥CIN 2 cases revealed positivity of 81.82% (9 out of 11). Of the 28 negative cases 92.86% were in < CIN 1 and CIN 1 category. However, two negative cases were diagnosed as ≥CIN 2 lesions [Table 6].
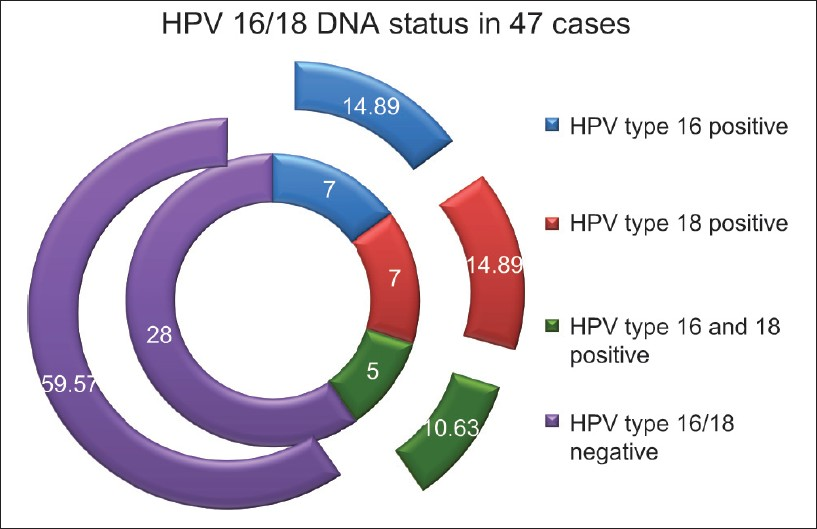
- Human papillomavirus 16/18 deoxyribonucleic acid status in 47 cervical tissues of Pap positive cases
DISCUSSION
To date there is no published data from Bangladesh regarding HPV genotype distribution in cervical premalignant and malignant lesions. A study by Khatun et al.,[12] revealed that 27% of the various cervical lesions ranging from inflammation, koilocytic changes to invasive cancer were positive for hrHPV types that included type 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68 by hybrid capture method. However, type-specific involvement could not be ascertained. Herein, we report for the first time on the distribution of hrHPV type 16/18 infection in Bangladeshi women with epithelial cell abnormality in Pap smear. The study included 1699 women who had undergone cervical cytology at a tertiary hospital in Bangladesh and 139 (8.18%) of them were found to have epithelial cell abnormality with bulk of the abnormality being found in the ≥45 years of age and low grade squamous intraepithelial lesion (LSIL) being the most frequent abnormality detected.[13] Forty eight of these women had their tissue examination done. PCR was done to find out the extent of HPV 16/18 infection and its association with cytohistomorphology. Around 40% of women with epithelial cell abnormality in Pap smear were associated with hrHPV 16/18 infection.
Determination of type specific HPV prevalence constitutes an important step towards guiding the selection of vaccine candidates for cervical cancer prevention and studying the oncogenic function of each genotype. It is well known that HPV 16 and 18 are the most predominant hrHPV type found in cervical cancer tissue around the world, while the prevalence of the other hrHPV types varies widely among different population and from one region to another. Again geographical differences also contribute to HPV type distribution in CINs globally.[14] However, worldwide estimates showed that HPV 16 accounted for 45.4% of all high grade lesions.[15] Greater variability can be seen in the other HPV type ranking positions. While world-wide, in Africa and Europe HPV 31 and HPV 33 were the second and the third most common types, these ranking positions corresponded to HPV 58 and HPV 18 in Latin America and the Caribbean, HPV 6 and HPV 18 in Northern America, HPV 58 and HPV 52 in Asia and HPV 31 and HPV 18 in Oceania.[15]
In our study, 19 of 47 women revealed hrHPV type 16 and/or 18 DNA. Twenty-eight (around 60% cases) patients were negative for hrHPV type 16/18 DNA. The raised prevalence of HPV 16/18 infection in women of ≥45 years of age may be related to reactivation of latent infection due to immune senescence and to new infection acquired in middle age. An interesting finding of our study is an equal prevalence of type 16 and 18 infection. Furthermore, it is to be noted that this study was carried out in women who were never screened for cervical cancer and all had epithelial cell abnormality in Pap smear.
In this study, among the 35 LSIL cases, 30 (85.7%) were in the < CIN 1 (15 cases) and CIN 1 (15 cases) category and 5 showed ≥CIN 2 lesions. Routine histopathology of the 10 cytologically high grade lesions, revealed 4 < CIN 1 and 6 ≥ CIN 2 lesions. In three high grade squamous intraepithelial lesion (HSIL) cases, histologically included in < CIN 1 lesion, PCR was positive for hrHPV 16/18 infection. This may be linked to sampling error and/or latent infection. In our study the prevalence of ≥CIN 2 lesions identified among women with LSIL and HSIL was 14.29% and 43%, respectively. This may vary considerably from study to study and be influenced by factors like patient population, methodology used and cytological interpretation.[16] Although useful clinically, the traditional CIN gradation is limited by subjectivity and poor reproducibility. Besides, histopathological interpretation may be limited by incorrect biopsy placement or failure to select the lesional area from the resected specimens. While visual patterns are not very helpful in guiding biopsy placement, obtaining more biopsies might increase the chance of finding the worst lesion. Again, the required number of biopsies for most efficient and reliable disease detection is still an issue of debate.[17]
Among the 11 histologically confirmed high grade lesions and malignancy, HPV type 16 and 18 was found in 3 (27.27%) and 2 (18.18%) cases, respectively with dual infection being present in 4 (36.36%). Around 80% positivity was found in ≥CIN 2 lesions. In our study, a total of 6 malignant cases were diagnosed in the Pap smear cytology of which we received tissue from only 3 cases. Histopathologically 1 was carcinoma in situ (CIS) and 2 were invasive cancer. One invasive cancer was HPV 18 positive and the other had double infection with HPV type 16 and 18. However, the CIS case turned out to be negative. Overall 92.86% of the negative cases (26 out of 28) were in the < CIN 1 and CIN 1 category. Interestingly, two negative cases were in the ≥CIN 2 category indicating the presence of other hrHPV type. Again, the possibility of a different prevalence pattern of HPV type 16/18 infection cannot be ruled out in this population. A significant association was noted between hrHPV 16/18 infection and high grade cervical lesions of women with epithelial cell abnormality in Pap smear.
Ours is a hospital based study done in a microenvironment. It was not feasible to assess the association of hrHPV type 16/18 infection in the cervical tissue of all the 139 women and there is every chance that those who did not undergo DNA testing can be harboring the infection. Long-term follow-up of CIN 3 cases showed that most do not develop into cervical cancer.[18] Therefore, future research on hrHPV DNA analysis of the cancer cases could be of great importance. Even then, in an over populated country like Bangladesh where women are usually married in their teens, have a high parity and are unaware of the importance of cervical cancer screening system, this study can provide an indication of the burden of hrHPV 16/18 infection prevailing here. Advanced, multi centered, large scale, nationwide genotyping studies including all hrHPV types are in demand for future epidemiological study and selection of vaccine strains.
CONCLUSION
Finally, this study suggests that the current HPV vaccination is expected to trim down the burden of hrHPV type 16/18 related cervical lesions in our population. Though, the analyses of this study relied on a limited number of cases the findings will contribute to HPV 16/18 knowledge in Bangladesh that will be useful in assessing the success of current vaccines with narrow type spectra and augmenting cervical cancer screening strategies.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE. Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
UB is responsible for conceiving, execution and analysis of the work and drafting the manuscript.
SA and PB are responsible for reporting of the cytopathology and histopathology slides.
AA is responsible for planning, PCR analysis and revising the article critically for important intellectual content.
ZR is responsible for reporting of the cytopathology and histopathology slides, coordinating the whole work and final approval of the version to be published.
Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
This study was conducted with approval from the Ethical Committee, Chittagong Medical College, Chittagong, Bangladesh. Authors take responsibility to maintain relevant documentation in this respect
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind mode (authors are blinded for reviewers and vice versa) through automatic online system
ACKNOWLEDGMENT
The authors wish to thank the CHEVRON, Clinical Laboratory Private Ltd., Chittagong, Bangladesh, for providing PCR facilities.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2013/10/1/14/115088
REFERENCES
- Distribution of HPV genotypes in cervical intraepithelial lesions and cervical cancer in Tanzanian women. Infect Agent Cancer. 2011;6:20.
- [Google Scholar]
- Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12-9.
- [Google Scholar]
- Natural history of cervical human papillomavirus infection in young women: A longitudinal cohort study. Lancet. 2001;357:1831-6.
- [Google Scholar]
- Comparison of HPV type distribution in high-grade cervical lesions and cervical cancer: A meta-analysis. Br J Cancer. 2003;89:101-5.
- [Google Scholar]
- Comprehensive study of several general and type-specific primer pairs for detection of human papillomavirus DNA by PCR in paraffin-embedded cervical carcinomas. J Clin Microbiol. 1996;34:745-7.
- [Google Scholar]
- Novel short-fragment PCR assay for highly sensitive broad-spectrum detection of anogenital human papillomaviruses. Am J Pathol. 1998;153:1731-9.
- [Google Scholar]
- Multiple HPV genotypes in cervical carcinomas: Improved DNA detection and typing in archival tissues. J Clin Virol. 2004;29:271-6.
- [Google Scholar]
- Human papillomavirus infection and cervical cancer prevention in India, Bangladesh, Sri Lanka and Nepal. Vaccine. 2008;26(Suppl 12):M43-52.
- [Google Scholar]
- Human Papillomavirusand Related Cancers in Bangladesh. 2010. Summary Report. Available from: http://www.who.int/hpvcentre
- [Google Scholar]
- Human papillomavirus and other risk factors in carcinoma cervix. Bangladesh Med J. 2009;38:22-7.
- [Google Scholar]
- Pattern of epithelial cell abnormality in Pap smear: A clinicopathological and demographic correlation. Cytojournal. 2011;8:8.
- [Google Scholar]
- World Cancer Report. Lyon: IARC Press; 2003.
- Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine. 2008;26(Suppl 10):K1-16.
- [Google Scholar]
- Prevalence of high-grade cervical lesion in women with LSIL and HSIL cytology and prevalence of invasive cancer in women cytologically positive for malignancy. Asian Pac J Cancer Prev. 2008;9:715-8.
- [Google Scholar]
- Grading the severity of cervical neoplasia based on combined histopathology, cytopathology, and HPV genotype distribution among 1,700 women referred to colposcopy in Oklahoma. Int J Cancer. 2009;124:964-9.
- [Google Scholar]
- Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: A retrospective cohort study. Lancet Oncol. 2008;9:425-34.
- [Google Scholar]








