Translate this page into:
“Low-grade squamous intraepithelial lesion, cannot exclude high-grade:” TBS says “Don’t Use It!” should I really stop it?
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The Bethesda System uses a two-tiered approach in the diagnosis of cervical squamous intraepithelial lesions (SILs). Occasionally, Papanicolaou (Pap) tests with evident low-grade SIL (LSIL) also have some features suggestive but not diagnostic of high-grade SIL (HSIL). This study reviews our experience with “Low-grade Squamous Intraepithelial Lesion, Cannot Exclude High-grade” (LSIL-H) and discusses the best approach to report such Paps if the LSIL-H interpretation is abandoned.
Methods:
Abnormal Paps were identified between January and December 2014 that had surgical follow-up within 6 months. Their biopsy outcomes were compared. Statistical analysis was performed using Pearson's Chi-square and McNemar tests in SPSS software version 23. Statistical significance was defined as P ≤ 0.05.
Results:
There were a total of 1049 abnormal Paps with follow-up. High-grade dysplasia/carcinoma (HGD+) was found in 8% of LSIL, 30% of LSIL-H, 52% of atypical squamous cells (ASCs), cannot rule out HSIL (ASC-H), and 77% of HSIL Paps. The detection rate of HGD+ for LSIL-H was between that of LSIL (Pearson's Chi-square test, P = 0.000) and ASC-H (P = 0.04). If LSIL-H cases are reported as ASC-H, the rate of HGD+ for the ASC-H category would decrease from 51.5% to 37.4% (McNemar test, P = 0.000). Alternatively, if LSIL-H cases are downgraded to LSIL, the rate of HGD+ for the LSIL category would rise from 7.7% to 10.4% (McNemar test, P = 0.000). Nearly 86.7% of LSIL-H cases were positive for high-risk HPV (HR-HPV) in comparison to 77.5% of LSILs, 100% of ASC-Hs, and 75% of HSILs. The sample size for HR-HPV and LSIL-H was too small for meaningful statistical analysis.
Conclusions:
“LSIL-H” category detects more HGD+ than LSIL, and fewer than ASC-H and HSIL. If LSIL-H is eliminated, Paps with this finding are best reported as ASC-H to ensure that women with potential HGD+ undergo colposcopy in a timely manner. Reporting LSIL-H as LSIL may delay colposcopy since management of LSIL Paps depends on multiple factors (age, HPV status, etc.).
Keywords
Human papillomaviruses
Papanicolaou test
squamous intraepithelial lesions of the cervix
The Bethesda System
INTRODUCTION
The purpose of cervical cancer screening is to detect high-grade squamous intraepithelial lesions (HSILs). These lesions have an increased risk of progression to cancer as a result of persistent Human papillomavirus (HPV) infection. Conversely, low-grade SILs (LSIL) often reflect transient infection with HPV and regress over time.[123] The Bethesda System (TBS) uses a two-tiered approach to cervical SILs in identifying and clinically managing these two groups.[456] For women with LSIL, management varies from repeat cytology to colposcopy, depending on factors such as age and HPV status. Management of women with HSIL requires colposcopy and/or immediate loop electrosurgical excision procedure (LEEP).[78] Overall, the main difference in the management of LSIL and HSIL is that patients with LSIL may or may not have colposcopy, while those with HSIL should.
Occasionally, Papanicolaou (Pap) tests with evident LSIL also have some features suggestive but not diagnostic of HSIL. These Paps have scattered cells that are worrisome for a higher grade lesion but quantitatively or qualitatively fall short of a definitive diagnosis of HSIL. We have historically struggled with the best way to convey these findings on Pap reports and have been using the terms “LSIL, cannot exclude high grade” (LSIL-H) or “LSIL and atypical squamous cells (ASCs), cannot rule out a high-grade intraepithelial lesion (ASC-H).” Studies have reported on the diagnostic challenge these cases represent. Terminology used in these studies shows a wide variation including the following: LSIL with an additional note alerting the provider to the presence of cells suggestive of HSIL, LSIL with ASC-H, LSIL cannot exclude HSIL, SIL, LSIL, and ASC-H.[91011] Emerging data since the publication of TBS 2001 show that LSIL-H cases differ from LSIL and HSIL categories based on both histologic outcomes and HPV prevalence. LSIL-H represents an intermediate risk between LSIL and HSIL for harboring high-grade dysplasia/carcinoma (HGD+) on biopsy, ranging from 24% to 41% of cases.[123911121314151617] In comparison, LSIL's risk of HGD+ on biopsy has been reported to range from 6% to 21%, whereas HSIL's risk ranges from 66% to 81%.[129121417] The prevalence of high-risk (HR)-HPV in LSIL-H has been found to be higher in comparison to LSIL and ASC-H in some studies.[11014]
Based on reported differences in histologic follow-up and HPV data, we anticipated the acceptance of LSIL-H as a separate interpretative category in the 2014 revision of TBS, with a recommendation to limit its use to a small percentage of cases that fall into this intermediary group. However, TBS 2014 continued to discourage the use of LSIL-H, mainly to prevent the re-emergence of a three-tiered reporting system and to maintain the current management guidelines linked to TBS terminology.[6]
The purpose of our study is to share our experience with LSIL-H, including cases with available HPV data, and reiterate its value as an interpretative category. In addition, we discuss the best approach to report such Paps if we abandon using the LSIL-H interpretation as TBS 2014 continues to recommend.
MATERIALS AND METHODS
The Bellevue Hospital Center (New York, NY, USA) pathology database (CoPath) was searched for abnormal Papanicolaou tests results, HPV results, and follow-up surgical pathology results during a 1-year period from January 1, 2014, to December 31, 2014 [Figure 1]. Abnormal Pap test results targeted were ASCs of undetermined significance (ASCUS), LSIL, LSIL-H, ASC-H, and HSIL/positive for carcinoma (HSIL+). Pap tests with glandular abnormalities and cases without histologic follow-up were excluded from the study. Histologic follow-up included cervical and vaginal biopsies, Endocervical curettage (ECC), LEEP, cone excision, and hysterectomy specimens. Surgical pathology diagnoses were categorized as negative/benign (no HPV effect or dysplasia identified), low-grade dysplasia (HPV cytopathic effect and/or cervical intraepithelial neoplasia [CIN] 1), and high-grade dysplasia/carcinoma (CIN 2/3 and squamous cell carcinoma; HGD+). Surgical follow-up data were restricted to 6 months following the abnormal Pap diagnosis. HR-HPV testing, if performed, and patient age were recorded.

- Summary of methods. ASCUS: Atypical squamous cells of undetermined significance, LSIL: Low-grade squamous intraepithelial lesion, LSIL-H: Low-grade squamous intraepithelial lesion; cannot exclude high grade, ASC-H: Atypical squamous cells; cannot rule out high grade, HSIL+: High-grade squamous intraepithelial lesion or carcinoma, CIN: Cervical intraepithelial neoplasia, ECC: Endocervical curettage, LEEP: Loop electrosurgical excision procedure, LGD: Low-grade dysplasia, HGD+: High-grade dysplasia/carcinoma, HPV: Human papillomavirus, HR: High risk
All Pap tests were liquid-based preparations from specimens collected in SurePath (BD Diagnostics, Burlington, NC, USA) or ThinPrep (Hologic, Inc., Marlborough, MA, USA). HPV testing was done with the APTIMA HPV Assay (Hologic, Inc., Marlborough, MA, USA), an in vitro nucleic acid amplification test for the qualitative detection of E6/E7 viral messenger RNA from 14 HR types of HPV using Gen-Probe TIGRIS DTS Technology;[18] the results were recorded as not detected (negative) or detected (positive) (North Shore-LIJ Laboratories, Lake Success, NY, USA).
All Pap tests were reviewed and interpreted by board-certified cytopathologists, and surgical cases by surgical pathologists with subspecialty expertise in gynecologic pathology.
Statistical analysis was performed using Pearson's Chi-square and McNemar tests in SPSS software version 23 (IBM SPSS Statistics for Windows. IBM Corp. 2015. Armonk, NY, USA).
Statistical significance was defined as P ≤ 0.05.
The Institutional Review Boards at New York University School of Medicine and Bellevue Hospital Center approved this study.
RESULTS
There were 22,415 Pap tests performed during the 1-year period from January 1, 2014, to December 31, 2014. Abnormal Pap test results with diagnoses of ASCUS, LSIL, ASC-H, LSIL-H, or HSIL+ represented 3136 (14%) cases. Surgical follow-up within 6 months was available for 1049 cases including 394 ASCUS, 481 LSIL, 66 LSIL-H, 33 ASC-H, and 75 HSIL+. Of the 1049 Paps with surgical follow-up, 522 (49.8%) had associated HR-HPV testing. All Pap tests were liquid based, including 565 SurePath (53.9%) and 484 ThinPrep (46.1%).
The patients ranged from 21 to 85 years in age, with an average age of 41 years. Three hundred women were aged 30 years or younger (28.6%), while 749 were over the age of 30 years (71.4%). The mean ages of the patients within each diagnostic category were as follows: ASCUS, 44 years (range, 21–85 years); LSIL, 37 years (range, 21–81 years); LSIL-H, 37 years (range, 21–70 years); ASC-H, 41 years (range, 21–71 years); and HSIL+, 47 years (range, 21–74 years).
Table 1 and Figure 2 provide the abnormal Pap categories with their follow-up surgical diagnoses. HGD+ was found in 8% of LSIL, 30% of LSIL-H, 52% of ASC-H, and 77% of HSIL+ Paps. Low-grade dysplasia was found in 76% of LSIL, 62% of LSIL-H, 33% of ASC-H, and 15% of HSIL+ Paps. The detection rate of HGD+ for LSIL-H was between that of LSIL (Pearson's Chi-square test, P = 0.000) and ASC-H (P = 0.04) [Table 2 and Figure 3]. If the LSIL-H category is abandoned and LSIL-H cases are reported as ASC-H, the rate of HGD+ for the ASC-H category would decrease from 51.5% to 37.4% (McNemar test, P = 0.000). Alternatively, if LSIL-H cases are downgraded to LSIL, the rate of HGD+ for the LSIL category would rise from 7.7% to 10.4% (McNemar test, P = 0.000).

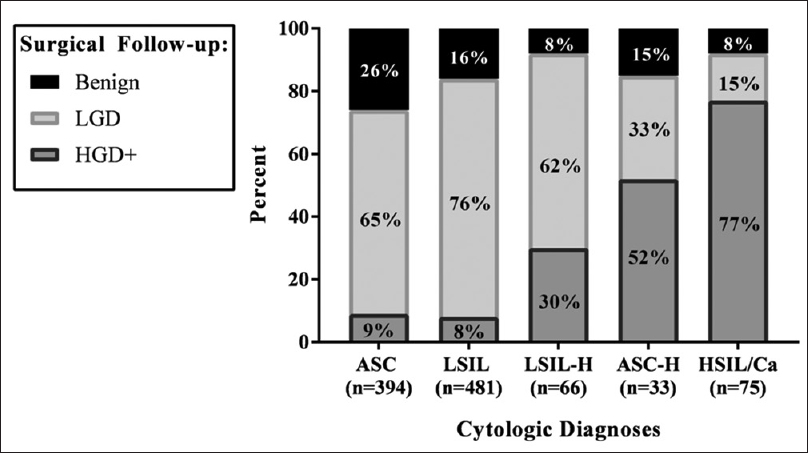
- Year 2014 abnormal Papanicolaou tests with 6-month tissue follow-up. ASCUS: Atypical squamous cells of undetermined significance, LSIL: Low-grade squamous intraepithelial lesion, LSIL-H: Low-grade squamous intraepithelial lesion; cannot exclude high grade, ASC-H: Atypical squamous cells; cannot rule out high grade, HSIL: High-grade squamous intraepithelial lesion, LGD: Low-grade dysplasia, HGD+: High-grade dysplasia/carcinoma
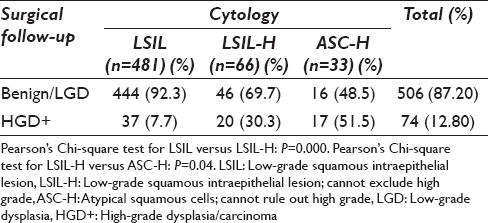

- Tissue (histologic) outcomes in abnormal Papanicolaou tests. LSIL: Low-grade squamous intraepithelial lesion, LSIL-H: Low-grade squamous intraepithelial lesion; cannot exclude high grade, ASC-H: Atypical squamous cells; cannot rule out high grade, LGD: Low-grade dysplasia, HGD+: High-grade dysplasia/carcinoma
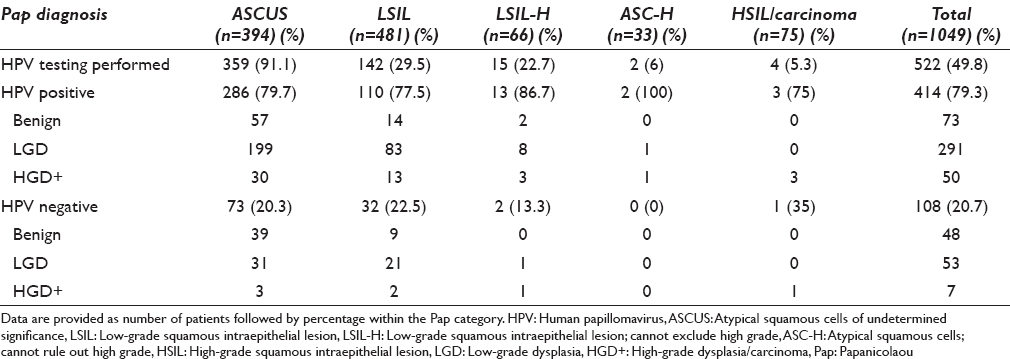
Table 3 shows the HPV detection rates for the abnormal Pap tests, including breakdown of cases by follow-up surgical diagnosis. Of the 1049 Paps with surgical follow-up, 522 (49.8%) had associated HR-HPV testing. Within the 522 cases, 414 (79.3%) were positive for HR-HPV. Regarding the 66 cases of LSIL-H, 15 (23%) had associated HR-HPV testing. Of these 15 cases, 13 (86.7%) were positive for HR-HPV, while 2 (13.3%) were negative. In comparison, LSIL (n = 481) had 110 (77.5%) cases positive, ASC-H (n = 2) had both cases positive (100%), and HSIL+ (n = 4) had 3 cases positive (75%). These numbers are too small for meaningful statistical analysis.
DISCUSSION
Our study shows that a diagnosis of LSIL-H on Pap test carries an intermediate risk for harboring cervical high-grade lesions or carcinoma, falling between LSIL and ASC-H or HSIL interpretative categories. The incidence of HGD+ shows an incremental increase in each respective category. Our rate of HGD+ on follow-up is 8% for LSIL, 30% for LSIL-H, 52% for ASC-H, and 77% for HSIL. These findings are not new to literature. Several studies reported similar results since the late 1990s before the publication of TBS 2001 revisions.[123911121314151617] Despite the mounting evidence indicating that the LSIL-H diagnosis leads to increased detection of HGD+ compared to LSIL, TBS 2014 excluded LSIL-H as a distinct interpretative category. Our study is the first after the implementation of TBS 2014 that emphasizes the importance of LSIL-H and recommending its use in clinical practice.
Table 4 highlights selected studies showing the frequency of HGD+ on follow-up of women with LSIL-H Pap test results.[123911121314151617] The incidence varies from 24% to 41% with most studies clustering between 30% and 40%. All these studies support the use of LSIL-H as a separate category, warranting appropriate management and follow-up to rule out HGD+.[15] They conclude that while LSIL-H may not represent a unique biologic entity, it does prove to have clinical usefulness in its high positive predictive value (PPV) for high-grade lesions.[12] Ince et al. looked at histologic outcomes and the PPV for high-grade dysplasia on biopsy over a 5-year period and found a HGD+ detection rate of 40% for LSIL-H. As a result of its intermediate status, they recommended that LSIL-H should be considered in its own distinct category and must be given clear cytomorphologic criteria to aid in the more rapid detection and treatment of some women with high-grade dysplasia.[9] Finkelstein et al. and Thrall et al. agreed with similar results, detecting high-grade lesions in 35% and 32% of LSIL-H Paps, respectively.[316] Owens et al. also found that LSIL-H offered an intermediate risk of high-grade dysplasia (40%) compared to LSIL (11%), ASC-H (27%), and HSIL (66%).[1] Al-Nourhji et al. and Alsharif et al. reported an intermediate detection rate of HGD+ for LSIL-H (24% and 33%, respectively), with LSIL-H being more similar to ASC-H (26%); they recommended management with colposcopy for LSIL-H similar to ASC-H.[213] Shidham et al. found high-grade dysplasia in 33% of their LSIL-H cases, similar to ASC-H at 31%, higher than LSIL at 10%, and lower than HSIL at 69%.[17] In our study, LSIL-H detected more HGD+ lesions than LSIL and fewer than ASC-H.

Owens et al. compared HR-HPV status in LSIL-H and ASC-H and found a significant difference, with increased prevalence of HR-HPV in LSIL-H (100%) compared to ASC-H (59%).[1] Shidham et al. reported HPV testing for 34 of 88 LSIL-H cases, finding 94% positive for HR-HPV; they concluded that since HPV is expected to be positive in these cases, it may not be a useful ancillary test to guide management.[17] Zhou et al. found the prevalence of HR-HPV in LSIL-H (92%) to be closer to HSIL (91%), when compared to LSIL (74%) and ASC-H (78%).[10] And most recently, Barron et al. found similar detection rates for high-grade dysplasia in LSIL-H (29.4%), with distinct HR-HPV associations, including a detection rate of 91% for LSIL-H, 96% for HSIL, and 80% for LSIL; they concluded that LSIL-H is a unique category of cytologic abnormality with distinct HR-HPV and high-grade dysplasia rates.[14] We have too few LSIL-H cases with HR-HPV results (n = 15) to report statistically significant differences between HR-HPV status among different categories of SIL. Despite this limitation, 87% of our LSIL-H cases were positive for HR-HPV compared to 78% of LSILs and 100% of ASC-Hs.
There are very few reports in literature arguing against the validity of LSIL-H as a separate category since the publication of LSIL-H-related studies. Some argue that an LSIL-H category should not be created because it would not improve patient care and outcomes based on the fact that colposcopy would be required in these patients anyway.[19] Furthermore, it was noted that LSIL-H is not a reliable category due to lack of studies on interobserver agreement and its overall rare incidence.[19] We argue that patient care would improve from earlier detection of HGD+ if LSIL-H were to be uniformly reported rather than potentially downgraded to LSIL. With the addition of HR-HPV as a co-test to Pap screening for women above the age of 30 years, it is not uncommon that women will not undergo colposcopy if HR-HPV is negative in certain clinical circumstances such as postmenopausal status. The overall incidence of LSIL-H is low because TBS recommends not using it. In addition, interobserver variability studies cannot be done if the diagnosis is not accepted and uniformly used. The fact that studies from many different institutions and practice settings have confirmed the intermediate risk for LSIL-H and its association with HR-HPV speaks to the agreement on and the consistency of the diagnosis. Of course, periodic review of such a diagnosis would be essential in comparison to other diagnostic categories. Walavalkar et al. looked at the temporal use of LSIL-H and other categories over a 6-year period and found increased use of LSIL-H due to a higher threshold for diagnosing HSIL. They concluded that to ensure the proper use of LSIL-H, monitoring and feedback of its use is essential, but overall would benefit from being its own category.[11]
Although it was not the aim of this study to review and describe the morphologic features leading to the diagnosis of LSIL-H, we would like to expand on the difficulty in accurately classifying a small portion of Paps showing such changes in daily practice. These Paps have unequivocal criteria fulfilling LSIL interpretation. In addition, they show cells suggesting an HSIL but fall short of a definitive diagnosis of HSIL either quantitatively or qualitatively. The most common scenario in our experience is the presence of scattered smaller cells with nuclear-to-cytoplasmic ratios higher than would be acceptable for LSIL, showing variable degrees of hyperchromasia and nuclear contour irregularities. Nasser et al. reported that three cell types were prominent in promoting suspicion of a high-grade lesion in LSIL-H Paps. These included atypical metaplastic squamous cells, atypical keratinized cells, and dysplastic cells with borderline nuclear-to-cytoplasmic ratios.[15] The dilemma is whether to report these Paps as LSIL, ASC-H, or HSIL. None of these interpretative categories convey the cytologic findings accurately. Unfortunately, with the current TBS, the pathologist is forced to choose a reporting category that does not adequately communicate the cytologic findings, creates difficulties in quality assurance statistics, and may not be managed appropriately.[17]
Based on our experience and results reported by others, we believe LSIL-H should be a distinct interpretative category in TBS. When a Pap exists that has clear-cut LSIL and rare cells suggestive of HSIL, it creates a diagnostic dilemma with either an undercall as LSIL or an overcall as HSIL or ASC-H without regard for the LSIL component. We found, similar to other studies, that LSIL-H does detect more HGD+ compared to LSIL, offering promise to this category's usefulness.[123911121314151617] If LSIL-H is eliminated and not used, Paps with this finding may be best reported as ASC-H to ensure that women with potential high-grade dysplasia undergo colposcopy in a timely manner. Reporting LSIL-H as LSIL may delay colposcopy since the management of LSIL Pap depends on multiple factors (age, HPV status, etc.). HR-HPV testing may prove helpful in triaging women with LSIL-H, considering some studies have reported higher rates of positive HR-HPV cases.[11014]
SUMMARY
Based on our experience and results reported by others, we recommend LSIL-H to be a distinct interpretative category in TBS. When a Pap exists that has clear-cut LSIL and findings suggestive of HSIL, it creates a diagnostic challenge resulting in either an undercall as LSIL or an overcall as HSIL or ASC-H without regard for the LSIL component. LSIL-H detects more HGD+ compared to LSIL, offering promise to this category's usefulness.[1239111213141516] If LSIL-H is not used, Paps with this finding are best reported as ASC-H to ensure that women with potential high-grade dysplasia undergo colposcopy in a timely manner. Reporting LSIL-H as LSIL may delay colposcopy since the management of LSIL Pap depends on multiple factors (age, HPV status, etc.). HR-HPV testing may prove helpful in triaging women with LSIL-H, considering some studies have reported higher rates of positive HR-HPV cases.[11014] Further studies focusing on clinical management and interobserver agreement are needed before excluding LSIL-H as a distinct category in the upcoming revisions of TBS.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The author(s) declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author.
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
AS conceived the study and, with JMC and MA, participated in the design of the study. JC, MA, RR, PE, and MYC participated in data retrieval and organization. FZ participated in data and statistical analyses. JMC, AS, FZ, MYC, and JC participated in drafting and editing the manuscript. All authors read and approved the final manuscript.
Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
This study was conducted with approval from the Institutional Review Board of the institution associated with this study as applicable. This study was a retrospective study not directly involving the patients. Authors take responsibility to maintain relevant documentation in this respect.
LIST OF ABBREVIATIONS (In alphabetic order)
ASCs - Atypical squamous cells
ASCUS - Atypical squamous cells of undetermined significance
ASC-H - Atypical squamous cells, cannot rule out high-grade squamous intraepithelial lesion
HGD+ - High-grade dysplasia/carcinoma
HPV - Human papillomavirus
HR-HPV - High-risk human papillomavirus
HSIL - High-grade squamous intraepithelial lesion
LGD - Low-grade dysplasia
LSIL - Low-grade squamous intraepithelial lesion
LSIL-H – Low-grade squamous intraepithelial lesion, cannot exclude high grade
Pap(s) - Papanicolaou test(s)
SIL(s) - Squamous intraepithelial lesion(s)
TBS - The Bethesda System.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- “Low-grade squamous intraepithelial lesion, cannot exclude high-grade squamous intraepithelial lesion” is a distinct cytologic category: Histologic outcomes and HPV prevalence. Am J Clin Pathol. 2007;128:398-403.
- [Google Scholar]
- Clinical significance of the diagnosis of low-grade squamous intraepithelial lesion, cannot exclude high-grade squamous intraepithelial lesion. Cancer. 2009;117:92-100.
- [Google Scholar]
- The utility of ‘low-grade intraepithelial lesion, cannot exclude high grade’ diagnosis: A single institution's experience. Acta Cytol. 2012;56:383-7.
- [Google Scholar]
- The Bethesda System for Reporting Cervical Cytology Definitions, Criteria and Explanatory Notes. New York: Springer-Verlag; 2004.
- The 2001 bethesda system: Terminology for reporting results of cervical cytology. JAMA. 2002;287:2114-9.
- [Google Scholar]
- The Pap test and bethesda 2014: “The reports of my demise have been greatly exaggerated.(After a quotation from Mark Twain)”. J Low Genit Tract Dis. 2015;19:175-84.
- [Google Scholar]
- 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. Am J Obstet Gynecol. 2013;17:S1-27.
- [Google Scholar]
- American Society for Colposcopy and Cervical Pathology-Sponsored Consensus Conference. 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. Am J Obstet Gynecol. 2007;197:340-5.
- [Google Scholar]
- Clinical importance of “low-grade squamous intraepithelial lesion, cannot exclude high-grade squamous intraepithelial lesion (LSIL-H)” terminology for cervical smears 5-year analysis of the positive predictive value of LSIL-H compared with ASC-H, LSIL, and HSIL in the detection of high-grade cervical lesions with a review of the literature. Gynecol Oncol. 2011;121:152-6.
- [Google Scholar]
- Evidence for increasing usage of low-grade squamous intraepithelial lesion, cannot exclude high-grade squamous intraepithelial lesion (LSIL-H) Pap test interpretations. Cancer. 2014;122:123-7.
- [Google Scholar]
- The significance of “low-grade squamous intraepithelial lesion, cannot exclude high-grade squamous intraepithelial lesion” as a distinct squamous abnormality category in Papanicolaou tests. Cancer. 2006;108:277-81.
- [Google Scholar]
- Pathology correlates of a Papanicolaou diagnosis of low-grade squamous intraepithelial lesion, cannot exclude high-grade squamous intraepithelial lesion. Cancer. 2008;114:469-73.
- [Google Scholar]
- Low-grade squamous intraepithelial lesion/cannot exclude high-grade squamous intraepithelial lesion (LSIL-H) is a unique category of cytologic abnormality associated with distinctive HPV and histopathologic CIN 2+detection rates. Am J Clin Pathol. 2014;141:239-46.
- [Google Scholar]
- The significance of the Papanicolaou smear diagnosis of low-grade squamous intraepithelial lesion cannot exclude high-grade squamous intraepithelial lesion. Cancer. 2003;99:272-6.
- [Google Scholar]
- The impact of LSIL-H terminology on patient follow-up patterns: A comparison with LSIL and ASC-H. Diagn Cytopathol. 2013;41:960-4.
- [Google Scholar]
- Should LSIL with ASC-H (LSIL-H) in cervical smears be an independent category? A study on SurePath specimens with review of literature. Cytojournal. 2007;4:7.
- [Google Scholar]
- Aptima HPV Assay [package insert]. Marlborough, MA: Hologic, Inc; 2015.








