Translate this page into:
Ossifying fibromyxoid tumor — Diagnostic challenge for a cytopathologist
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
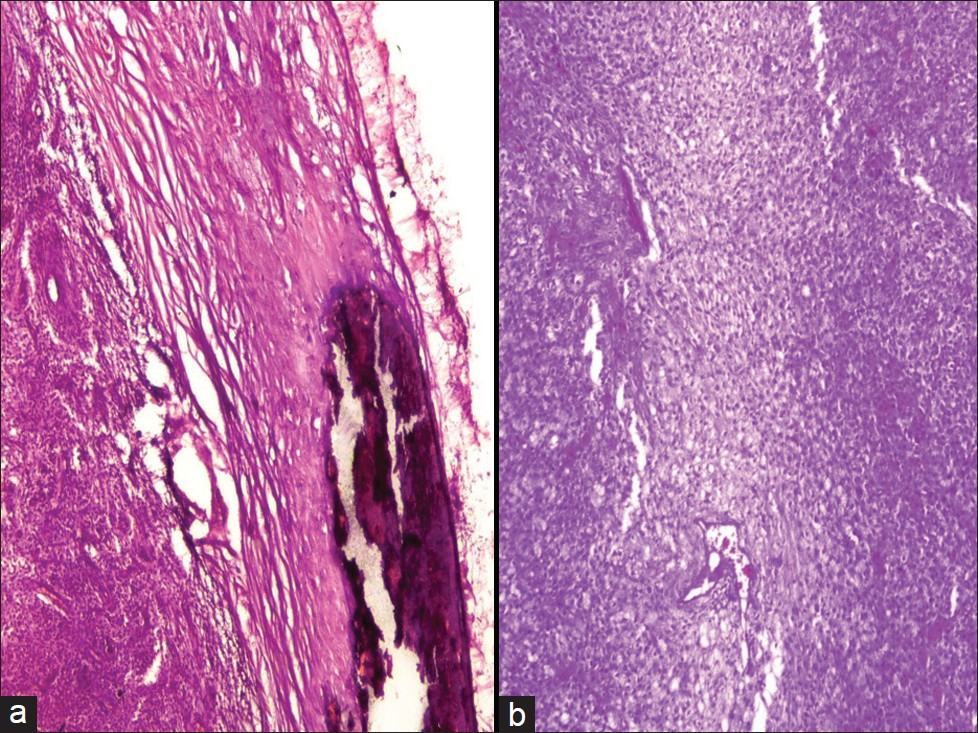
We present an interesting case of a 51-year-old male who presented with a history of a gradually increasing, painless swelling on the right wrist, for the past — three to four months. Local examination showed a firm swelling measuring 3 cm in diameter, free from overlying skin and underlying muscles. The patient did not given any history of trauma. A plain radiograph of the wrist revealed a well-circumscribed soft tissue tumor, with an incomplete shell of calcification. No involvement of the underlying bone was seen. The patient was advised Fine Needle Aspiration (FNA) Cytology. FNA was performed with a 23 gauge needle. Scanty blood mixed aspirate was obtained. Smears were both air-dried and wet-fixed, and stained with May-Grunwald-Giemsa (MGG) and Papanicolaou stains, respectively. The FNA smears were moderately cellular showing predominantly singly scattered dispersed cells and a few cells arranged in clusters [Figures 1 and 2]. At few places, small rosette-like aggregates were also seen [Figure 3]. The tumor cells were polygonal to spindle-shaped, having round-to-oval paracentral nuclei [Figures 2 and 3 inset] and moderate-to-abundant cytoplasm, in the background of scanty myxoid stroma. The nucleus showed bland nuclear chromatin and small inconspicuous nucleoli. No cytological atypia, mitosis, or necrosis was seen. Based on the clinicoradiological and cytological features, a cytodiagnosis of benign mesenchymal tumor with possibility of ossifying fibromyxoid tumor (OFMT) was rendered and histopathological confirmation advised.
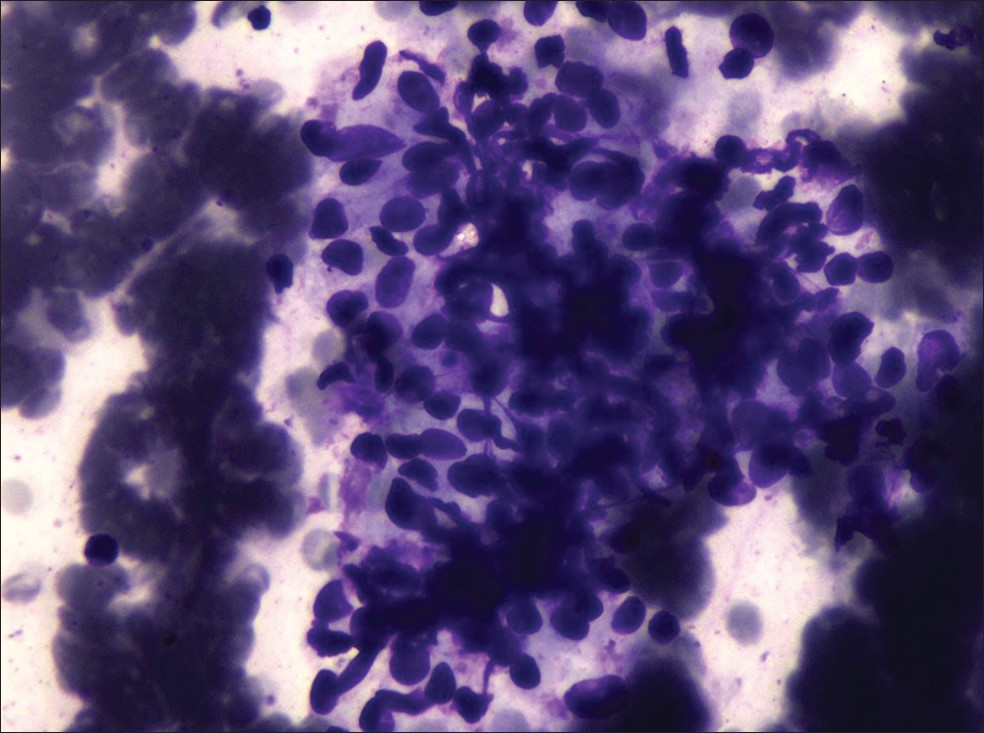
- Cytology smears showing moderate cellularity, cells present in clusters (Giemsa, ×40)
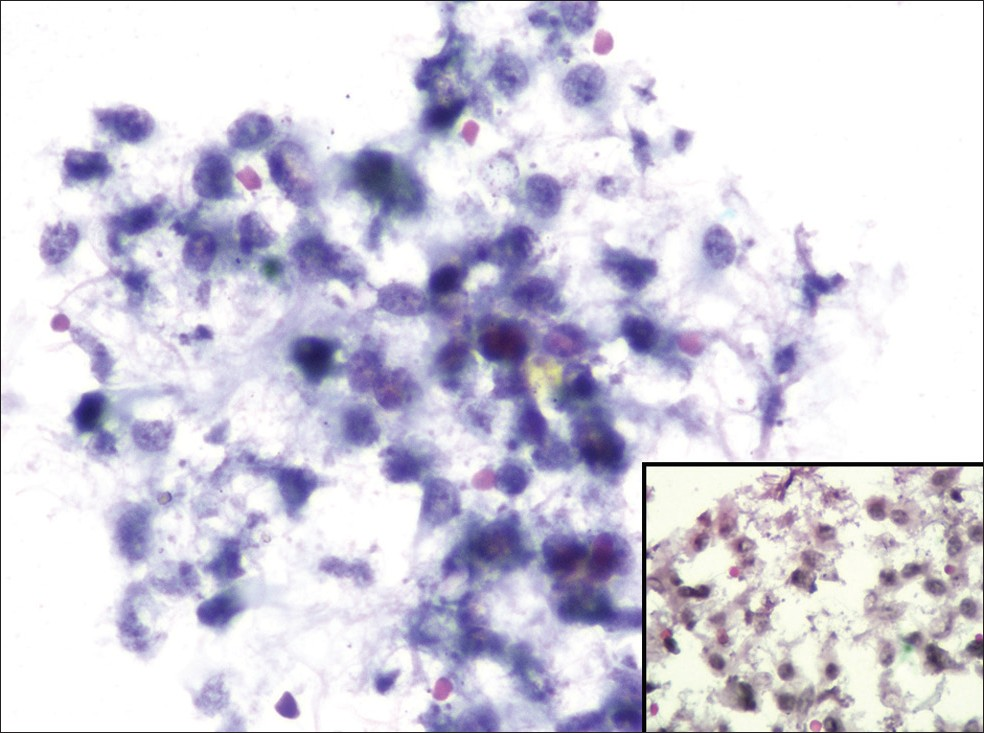
- Cytology smears showing moderate cellularity, cells present in clusters (Papanicolaou, ×40) and inset shows dispersed cells with paracentral nuclei (Papanicolaou, ×40)
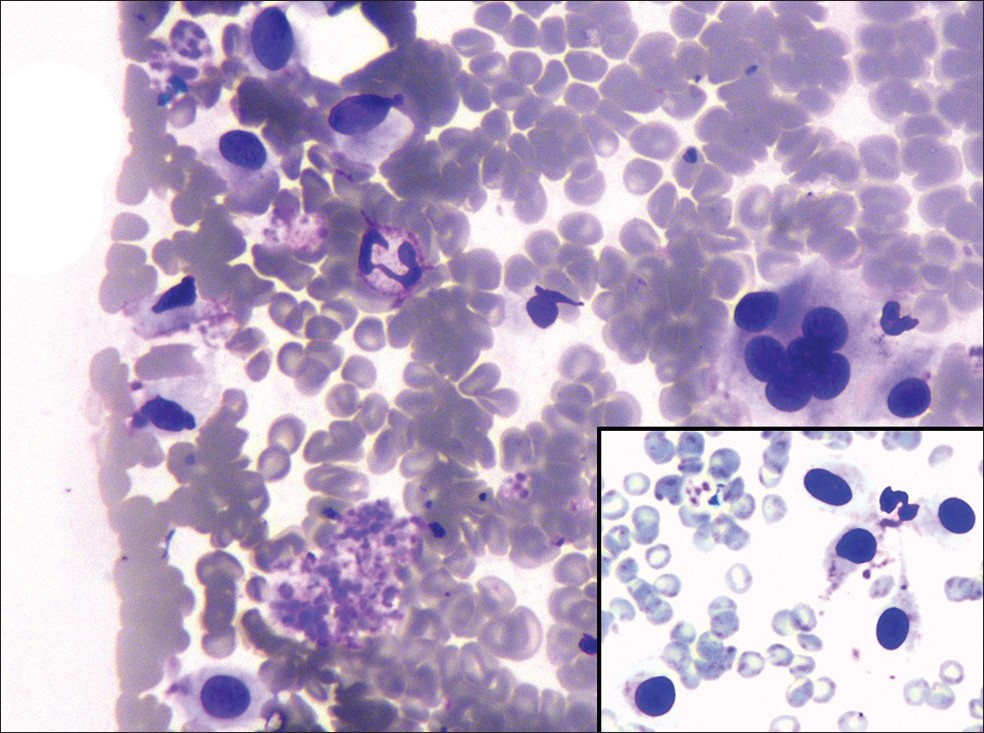
- Cytology smears showing dispersed cells and few cells arranged in rosette-like structure (Giemsa, ×40) and inset shows dispersed cells with paracentral nuclei (Giemsa, ×40)
Subsequently, the excised specimen was received, as a well-circumscribed, encapsulated mass, measuring 3.5 × 3.0 cm. The cut surface was gray-white, solid, homogenous, and firm in consistency [Figure 4], with a gritty sensation near the subcapsular area. Multiple sections showed a well-encapsulated tumor, with a partial shell of calcification [Figure 5a]. The tumor cells were arranged in large diffuse sheets [Figure 5b], cords, and nests, within the myxohyaline matrix [Figure 6]. Individual cells had an epithelioid appearance, with uniform cell-to-cell spacing. The tumor cells were round-to-ovoid, with vesicular nuclei, having small nucleoli and pale moderate cytoplasm [Figure 6 inset]. Few cells showed nuclear grooving. Mitotic counts varied from 0 – 1 / 50 high power field. No area of cytological atypia or necrosis was observed. The panel of immunostains comprising of cytokeratin (CK), Vimentin, S-100, smooth muscle actin (SMA), and epithelial membrane antigen (EMA) was applied using standard protocols, with the streptavidin-biotin complex technique. The tumor cells showed positivity for S-100 and vimentin and negative for the rest of the markers [Figures 7a-7d]. The final diagnosis of OFMT was made, and the patient was kept on follow-up.
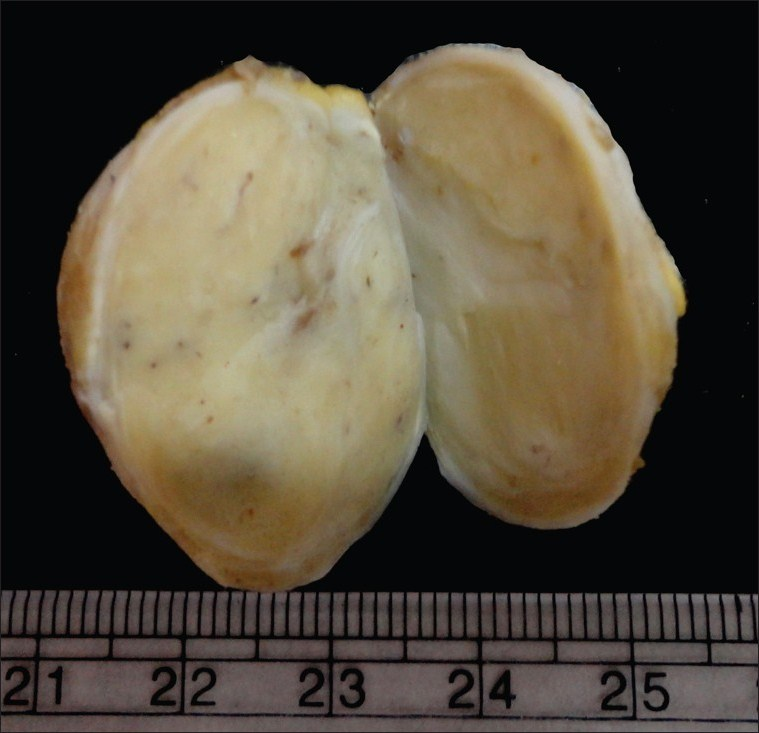
- Gross specimen showing a well-circumscribed, encapsulated mass with a homogenous cut surface
- (a) Section showing tumor with calcification in the capsule (H and E, ×10) (b) Section showing tumor cells arranged in diffuse sheets (H and E, ×10)
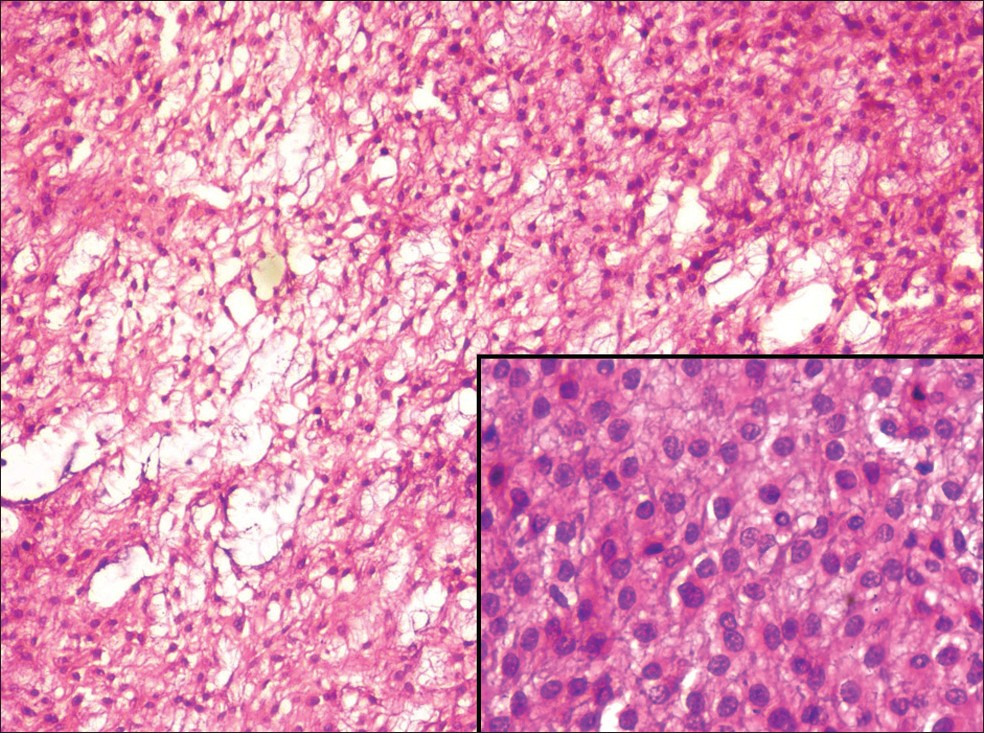
- Section showing tumor cells embedded in myxoid stroma (H and E, ×10) and inset shows rounded-to-ovoid cells with vesicular nuclei and moderate cytoplasm (H and E, ×40)
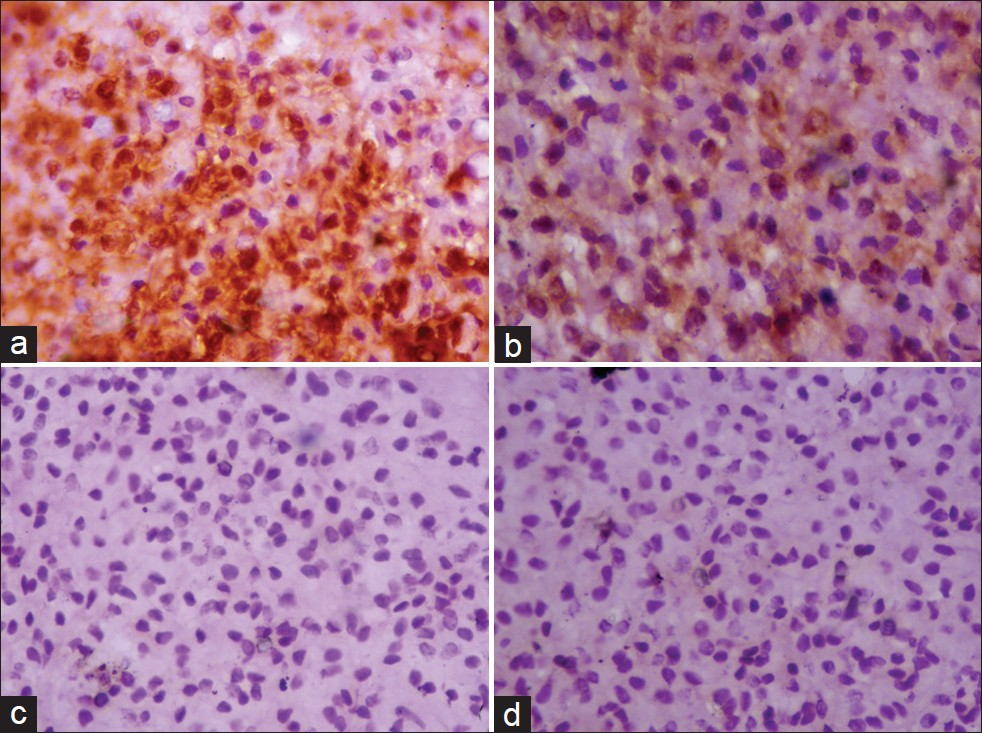
- (a) Section showing cytoplasmic and nuclear S-100 positivity in tumor cells (S-100, DAB, ×40) (b) Section showing focal vimentin positivity in tumor cells (Vimentin, DAB, ×40) (c) Section showing tumor cells negative for CK (CK, DAB, ×40) (d) Section showing tumor cells negative for SMA (SMA, DAB, ×40)
Ossifying fibromyxoid tumor of the soft tissue was first described in a series of 59 cases from the Armed Forces Institute of Pathology, by Enzinger, in 1989.[1] It is a rare tumor of uncertain differentiation. OFMT almost exclusively affects adults (mean age of 50 years), with only rare examples documented in children.[2] There is a slight male predominance. OFMTs are present as relatively small (mean size 3 cm), painless, well-defined subcutaneous masses, which involve the extremities, in approximately 70% of the cases. Radiologically, OFMT presents as a well-circumscribed mass, with an incomplete rim of calcification / ossification in the periphery.[3]
The cytomorphological features of OFMT have not been adequately described in literature. To the best of our knowledge, there are only four cytological descriptions[4–7] of OFMT to date. Out of which one is that of a malignant variant of OFMT[7] and another has been misdiagnosed as a follicular neoplasm, because the lesion had a pre-thyroid location, and FNAC showed epithelioid cytomorphology in rosette-like aggregates.[5] The remaining case reports have shown moderate-to-high cellularity and myxoid matrix material, with small clusters and dispersed oval-to-spindle cells embedded in the matrix. We also report similar findings; however, the matrix material was relatively less in our smears, as compared to the previously mentioned case reports. Histopathology and immunohistochemistry (IHC) further confirm the diagnosis of OFMT. Typical OFMT shows a tumor composed of lobules and cords of small bland cells in a myxohyaline background, with frequent peripheral ossification.
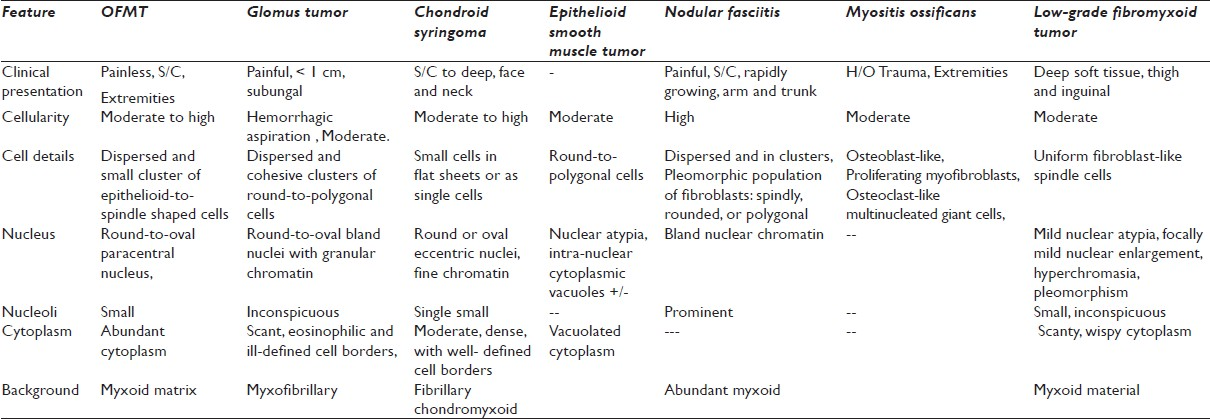
The cytological differential diagnosis includes lesions with fibromyxoid stroma and epithelioid-to-spindle cell cytomorphology.[8] The list includes glomus tumor, chondroid syringoma, epithelioid schwannoma, epithelioid smooth muscles tumors, and tumors with pseudosarcomatous differentiation, such as, nodular fasciitis, proliferative fasciitis, myositis ossificans, and low-grade fibromyxoid sarcoma [Table 1].[9–13] None of these lesions shows the characteristic rim of calcification in the capsule, which is characteristic of the radiological picture and sections of OFMT. Further immunohistochemistry with a panel comprising of CK, EMA, Vimentin, SMA, and S-100, can aid in rendering the correct diagnosis and ruling out the differentials. The malignant variant of OFMT needs to be differentiated from the extra-skeletal myxoid chondrosarcoma, extra-skeletal osteosarcoma, and epithelioid malignant peripheral nerve sheath tumor (MPNST).
The clinical behavior in most cases is that of a benign tumor, but almost 22% show local recurrence[14] and distant metastases have been seen in 6% of the cases.s[15] Hence, it is now considered to be a tumor with intermediate malignancy. The histogenesis of this rare tumor is debatable, although recent studies have suggested neuroectodermal differentiation.[16] Features associated with aggressive behavior are high cellularity, high nuclear grade, mitotic activity > 2 / 50 hpf, area of necrosis, vascular invasion, prominent spindling, and deposition of centrally placed osteoid.[17] Such a lesion, with aggressive morphology, has higher chances of local recurrence. Folpe et al.[18] proposed the criteria for diagnosis of atypical and malignant OFMT.
To conclude, OFMT is a rare soft tissue neoplasm of intermediate malignant potential. With increasing use of aspiration cytology in the preoperative diagnosis of soft tissue neoplasms, a cytopathologist needs to be aware of the cytological features of this uncommon neoplasm in order to facilitate an accurate diagnosis.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
The author(s) declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this case report and declare that they qualify for authorship. Each author has participated sufficiently in the study and take public responsibility for the appropriate portions of the content of this article. PG drafted the idea and manuscript. ShS participated in the drafting of the manuscript along, with technical help in immunostaining. RA participated in searching the literature and photography. SoS was involved in photography, case reporting, and final proofreading of the manuscript. RuG coordinated in the drafting of the manuscript, along with its final proofreading. AK provided technical help in carrying out the immunostaining and assisted in the literature review and photography. Each author acknowledges that this final version was read and approved by them.
ETHICS STATEMENT BY ALL AUTHORS
This manuscript is a case description in form of a letter. Therefore IRB approval was not mandatory.
EDITORIAL / PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through an automatic online system.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2012/9/1/17/99169
REFERENCES
- Ossifying fibromyxoid tumor of soft parts: A clinicopathological analysis of 59 cases. Am J Surg Pathol. 1989;13:817-27.
- [Google Scholar]
- Ossifying fibromyxoid tumor of soft parts in a child: a case report. J Pediatr Surg. 1999;34:1294-6.
- [Google Scholar]
- Radiographic appearance of an ossifying fibromyxoid tumor of soft parts. Skeletal Radiol. 1997;26:615-8.
- [Google Scholar]
- Cytologic diagnosis of ossifying fibromyxoid tumor of soft tissue: a case report. Diagn Cytopathol. 2004;30:41-5.
- [Google Scholar]
- Ossifying fibromyxoid tumor misdiagnosed as follicular neoplasia-a case report. Acta Cytol. 1997;41(4 Suppl):1261-4.
- [Google Scholar]
- Ossifying fibromyxoid tumor of soft parts: report of a case diagnosed on fine needle aspiration cytology. Cytopathology. 2012;23:126-8.
- [Google Scholar]
- Fine needle aspiration cytology of the malignant variant of ossifying fibromyxoid tumor of soft parts. Acta Cytol. 2001;45:745-55.
- [Google Scholar]
- Tumors of Uncertain or Unknown Origin. In: Orell SR, ed. The Cytology of Soft Tissue Tumors (1st ed). Switzerland: S Karger AG; 2003. p. :88.
- [Google Scholar]
- Chondroid syringoma diagnosed by fine needle aspiration cytology. Diagn Cytopathol. 2010;38:38-40.
- [Google Scholar]
- Fine needle aspiration in nodular fasciitis of the face. Cytopathology. 2002;13:128-32.
- [Google Scholar]
- Fine needle aspiration cytology of myositis ossificans. Diagn Cytopathol. 2011;39:432-4.
- [Google Scholar]
- Low grade fibromyxoid sarcoma: report of a case with fine needle aspiration cytology and histologic correlation. Acta Cytol. 2006;50:208-12.
- [Google Scholar]
- Ossifying fibromyxoid tumor of soft parts -a clinicopathologic and immunohistochemical study of 104 cases with long-term follow-up and a critical review of the literature. Am J Surg Pathol. 2008;32:996-1005.
- [Google Scholar]
- Tumors of Miscellaneous Type or Uncertain Lineage. In: Goldblum JR, ed. Bone and Soft Tissue pathology (1st ed). Philadelphia, PA: Saunders Company; 2010. p. :285-6.
- [Google Scholar]
- Ossifying Fibromyxoid Tumor May Express CD56 and CD99: A Case Report. Int J Surg Pathol. 2007;15:437-440.
- [Google Scholar]
- Atypical and malignant variants of ossifying fibromyxoid tumor: Clinicopathologic analysis of six cases. Am J Surg Pathol. 1995;19:1039-46.
- [Google Scholar]
- Ossifying fibromyxoid tumor of soft parts: a clinicopathologic study of 70 cases with emphasis on atypical and malignant variants. Am J Surg Pathol. 2003;27:421-31.
- [Google Scholar]







