Translate this page into:
Pattern of epithelial cell abnormality in Pap smear: A clinicopathological and demographic correlation
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
In the low resource settings of a developing country, a conventional Papanicolaou (Pap) test is the mainstay screening system for cervical cancer. In order to counsel women and to organize a public health system for cervical cancer screening by Pap smear examination, it is imperative to know the pattern of premalignant and malignant lesions. This study was undertaken to find out the prevalence of an abnormal Pap smear, in a tertiary hospital of a developing country, and to carry out a clinicopathological and demographical analysis for establishing the pattern of epithelial cell abnormality in a Pap smear.
Materials and Methods:
A cross-sectional descriptive study was carried out in a total of 1699 patients who underwent Pap smear examination. The prevalence of epithelial cell abnormality in the Pap smear was calculated in proportions / percentages. Specimen adequacy and reporting was assessed according to the revised Bethesda system.
Results:
Among the total of 1699 patients who had their Pap smear done, 139 (8.18%) revealed epithelial cell abnormality. Altogether 26 smears revealed high-grade lesions and malignancy, most of which were found to be in women belonging to the 30 – 39 and ≥ 45 age group. A total of 75 (53.96%) women were in the 20 – 44 age group and 64 (46.04%) were in the ≥ 45 age group. A bimodal age distribution was detected in the epithelial cell abnormality, with the bulk being diagnosed in patients aged 45 or above. Overall one-third of the patients with an abnormal Pap smear result showed healthy cervix in per vaginal examination.
Conclusions:
A raised prevalence of epithelial cell abnormality reflects the lack of awareness about cervical cancer screening. Women aged 45 or above harbor the bulk of premalignant and malignant lesions in the Pap smear, signifying that these women are among the under users of cytological screening.
Keywords
Cervical cancer
cytology
Papanicolaou smear
INTRODUCTION
Cervical cancer is considered preventable, as the premalignant stages can be detected by exfoliative cytology like a Papanicolaou (Pap) smear examination. Nowadays, cytology along with Human Papilloma Virus (HPV) testing is being assessed as a screening test for cervical cancer in the developed countries. Similar to other DNA viruses[1] (e.g., Adenovirus, Hepatitis B virus, etc.), HPV is detected by DNA testing with polymerase chain reaction (PCR) or Hybrid capture (HC). However, in the setting of a developing country the Pap test is useful as a screening modality, which is ultimately geared toward the reduction of cervical cancer–related mortality by the earlier detection of premalignant lesions.
Cervical epithelial cell abnormalities in the Pap smear represent a spectrum of intraepithelial lesions that lie along the pathway, from mild-to-severe dyskaryosis to invasive cancer.[2] The significance as well as consequence of cervical cytology with atypia or dyskaryosis has been extensively studied.[34] According to the 2001 Bethesda System[5] for reporting cervical cytological diagnoses, epithelial cell abnormalities originate in the squamous or glandular cells. The category of atypical squamous cells (ASC) includes ASC-US (ASC of undetermined significance) and ASC-H (ASC, cannot exclude high grade squamous intraepithelial lesions). The positive predictive value for HSIL (High-grade squamous intraepithelial lesion) in ASC-H is higher than in ASC-US, but not as high as in the category of HSIL.[6] The generic term squamous intraepithelial lesion (SIL) is subdivided into lesions showing perinuclear halo and mild dyskaryosis, termed as Low-grade squamous intraepithelial lesion (LSIL) and lesions showing moderate-to-severe dyskaryosis and carcinoma in situ, termed as HSIL. The category of “atypical glandular cells” is designated as AGC. Smears showing no epithelial abnormalities are depicted under the category of Negative for intraepithelial lesion or malignancy (NILM), in the revised Bethesda system.
Screening with Pap smear has been seen to be accompanied by a dramatic reduction in the incidence of invasive cervical cancer in different countries of the world. To date two types of Pap tests are in use: conventional and liquid-based cytology. Even as the liquid-based test is popular in the developed countries, in low resource settings, a conventional Pap test is the mainstay screening system. Various studies reveal that a majority of the cervical cancer mortality of the world comes from developing countries.[7–9] This may be attributed to the absence of an efficient cervical cancer screening system. Therefore, it is important to know the overall scenario of epithelial cell abnormality in the Pap smear, in a developing country like Bangladesh. Again, in order to counsel women and to organize a public health system for cervical cancer screening by Pap smear examination, it is imperative to know the pattern of premalignant and malignant lesions.
Standardization of the Pap smear reporting by the use of the revised Bethesda System has unified various overlapping terminologies and has included specific statements regarding specimen adequacy, general categorization, interpretation, and results. Hence, we have undertaken the present study using the revised Bethesda System, with the intention of finding out the prevalence of epithelial cell abnormality in the Pap smear of women visiting the Gynae Outpatient Department (GOPD) of a tertiary hospital in Bangladesh, and to carry out a clinicopathological and demographical analysis, to establish the pattern of epithelial cell abnormality in the Pap smear among the women visiting the hospital.
MATERIALS AND METHODS
A cross-sectional descriptive study was carried out in the Department of Pathology, Chittagong Medical College, Chittagong, Bangladesh, from the months of February to September, 2010. After taking a history (regarding parity, menstrual history, and duration of married life) and recording the findings (healthy or unhealthy) of per vaginal examination of the patients, the Pap smear was collected with the help of a wooden Ayer spatula. The smear was immediately fixed in alcohol for 30 minutes. Then Pap staining was done followed by light microscopy and slide interpretation. A total of 1699 slides were examined. Epithelial cell abnormality was detected in a total of 139 patients. Specimen adequacy as well as reporting was assessed according to the revised 2001 Bethesda system. Unsatisfactory smears were repeated. All patients with epithelial cell abnormalities were referred for colposcopy according to the standard procedure and recommendations.[10]
RESULTS
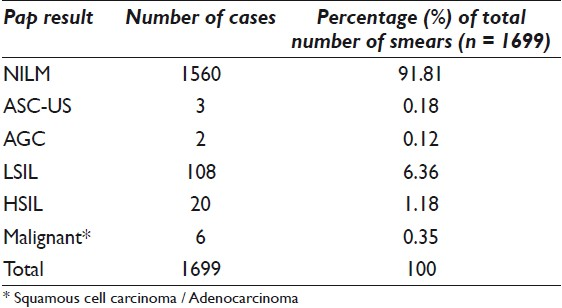
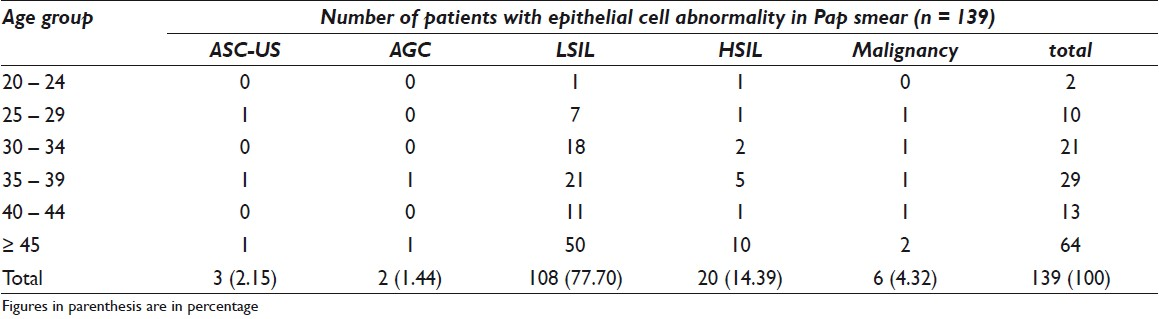
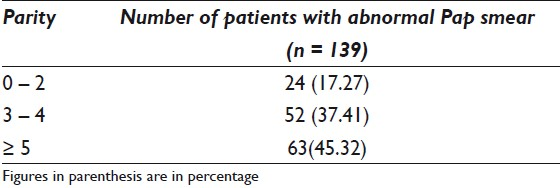
Among the 1699 Pap smears submitted, 139 (8.18%) revealed cervical epithelial cell abnormality [Table 1]. The age range of the 1699 patients was 15 – 82 years. The age of the patients with an abnormal Pap smear was between 21 and 70 years, with the mean age being 41.97 years. The most frequent epithelial cell abnormality was LSIL [Figure 1]. Altogether 26 Pap smears revealed high grade lesions and malignancy, most of which were found to be in women who belonged to the 30 – 39 and ≥ 45 year age group. A total of 75 (53.96%) women were in the 20 – 44 year age group and 64 (46.04%) were in the ≥ 45 year age group [Table 2]. The mean parity was 4.34 and the parity of a majority (45.32%) of patients was ≥ 5 [Table 3].

- Pattern of cervical epithelial cell abnormalities in a total of 139 positive Pap smears (February – September, 2010): LSIL 108(77.7%); HSIL 20(14.39%); ASC-US 3(2.15%); AGC 2(1.44%)
In the per vaginal examination, the cervix was taken as unhealthy when it revealed the presence of any of the following features, alone or in any combination: broadening of cervix, hypertrophy, ulceration, erosion, growth, Nabothian cyst, tear, and increased vascularity. A cervix that was smooth, pink, tubular, with a centrally placed external os was considered healthy. Approximately one-third of the patients with an abnormal Pap smear result had a healthy cervix.
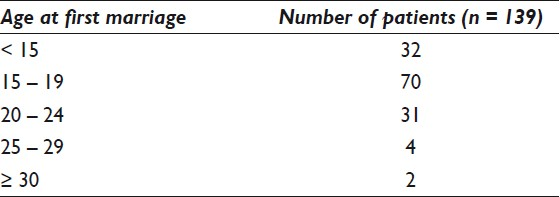
In the context of a country like Bangladesh where premarital sex is forbidden, age at first marriage can be taken as the age at the first sexual intercourse. The present study demonstrated that the average age at first marriage was around 16 [Table 4].
DISCUSSION
To date there are no published data from Bangladesh concerning the pattern of epithelial cell abnormality in Pap smear. In this study, we have applied the revised Bethesda System, which will obviously, to some extent, provide an idea about the overall picture of the epithelial cell abnormality in the Pap smear cytology of a developing country. Various studies on the prevalence of cervical epithelial cell abnormality in the Pap smear revealed 4.3% in a tertiary hospital in Kuwait,[11] 5% in a large referral hospital in Saudi Arabia,[12] 0.95% in Jewish Israeli women,[13] 1.66% in the Western region of Saudi Arabia,[14] and 7.9% in South-western Saudi Arabia.[15] However, unlike the previous studies, our study showed a raised prevalence (8.18%). This may be explained by the fact that these patients did not visit the tertiary health institute for cancer screening purpose, but rather with specific gynecological complaints, such as, something coming down per vaginum, mass descending per vaginum, lower abdominal pain, and abnormal vaginal bleeding or discharge. It is notable that they had come to visit the hospital when the dyskaryotic changes in the cervical epithelium had already occurred. All these patients were married and most of them were multipara, the mean parity being 4.34.
Edelman et al,[16] studied Pap smears from 29295 females over a period of one year and the Pap smear abnormalities were as follows: 9.9% ASC-US, 2.5% LSIL, 0.6% HSIL, and 0.2% invasive cancer. They also showed that adolescents with an age range of 13 – 22 years had a significantly higher rate of LSIL. Another study in Brazil,[11] where 1822 441 Pap smears were examined over a period of five years, showed that low-grade lesions were common among women in the age group of 15 – 30 years, while high-grade lesions were frequently encountered among women in the age group of 25 – 45 years. Patients older than 40 years had the greatest incidence of invasive cancer. In comparison to the previous studies our study revealed the following scenario: 0.18% ASC-US, 0.12% Atypical glandular cells (AGC), 6.36% LSIL, 1.18% HSIL, and 0.35% malignancy. The most frequent finding in our study was LSIL. Age incidence for low-grade lesions was in the reproductive age, with a peak in the 35 – 39 year age range. Another peak was seen in the ≥ 45 year age group. One of the significant discrepancies between our study and the previously published data from other countries is the lower rate of ASC-US and higher rate of LSIL. We assume that as the women included in our study were never routinely screened and / or re-screened, they presented with an advanced / definitive form of cytological interpretation in the cervical smear, and thus, LSIL rate was higher. Following the revised Bethesda System we designated those smears as ASC-US, which showed borderline changes that fell short of a definitive SIL interpretation, that is, the smears that were only suggestive of LSIL or SIL of indeterminate grade, were diagnosed as ASC-US. The overall insubstantial Pap smear screening scenario along with a drop out of some cases to private clinics could be a possible explanation for the significant variation in the percentage of ASC-US and LSIL from other studies of the world. Again, it was speculated that many of the ASC-US cases remained unattended, and if there was a regular, well-organized Pap smear screening system it was not unlikely that the ASC-US rate would have been higher. In addition, the criteria for ASC-US might differ subtly among laboratories due to technical differences in the slide preparation, as described in the revised Bethesda System. High-grade lesions were more common in women of ≥ 45 and 35 – 39 year age groups. Briefly, a bimodal age distribution was detected in the epithelial cell abnormality with the bulk being diagnosed in the ≥ 45 year age group. The present study also showed a wide age range (21 – 70 years). The mean age for these abnormal Pap smears was 41.97 years.
Previous studies indicate that the most common age to develop carcinoma cervix is between 40 and 50 years and the precursor lesions occur 5 – 10 years prior to developing invasive cancer.[17] It is interesting to note that 46.04% of the patients included in our study are in the ≥ 45 year age group, and are in the peri-/postmenopausal age. Both low- and high-grade lesions of the cervix were more commonly seen in these patients than in any other age group. This finding can be explained by the fact derived from previous studies that older age groups are among the under users of pap screening.[18] In the perspective of a developing country like Bangladesh, the reasons may be illiteracy, lack of awareness about cancer screening, and expenditure of the test. Besides, unavailability of cytological screening in the rural and suburban areas adds to the problem. The average life expectancy of people has increased and therefore if the low-grade cervical lesions persist and progress, then there is every chance that these women are at risk of developing higher grade lesions in the future. Again it is documented that the rate of progression of most lesions destined to become invasive cancer is generally considered to be slow, and one might therefore anticipate that a negative history before the age of 50 would considerably reduce the risk of positive cytology or histology in women of age 50 – 64 years, which is considered the upper age range in developed countries.[19] Our findings call attention to the need for cytological screening in this older age group of patients and the need to create awareness about cervical cancer for motivating them to attend screening.
A total of 45 patients with abnormal Pap results had a healthy-looking cervix. Eighteen of these patients were in the age group of 45 years or above. It is interesting to note that while 39 of these patients showed LSIL, four showed HSIL, and two showed malignancies in the Pap smear. This signifies that cervical cancer screening, based only on clinical impression and visual examination, is quite unpredictable in relation to cytological screening. This also connotes the value of universal cervical cancer screening, irrespective of an unhealthy or healthy looking cervix. In a large randomized controlled trial in India, Visual Inspection with Acetic acid (VIA) significantly prevented cervical cancer incidence and mortality in women aged 30 – 39 years. However, the same was not seen in case of older ages.[20] VIA may be the only screening approach applicable in many low-resource settings like ours. Nevertheless, the poor performance of this test due to non-visualization of the squamocoloumnar junction in the older age group indicates that it should be used in screening of women before they are of an age when the retreat of the transformation zone into the endocervix renders it invisible to the visual method.
It is to be noted that all the patients included in our study had never undergone Pap smear screening for cervical cancer. This shows that ever-increasing participation in the screening program must be given priority, to decrease the incidence of cervical premalignant and malignant lesions. Routine screening in Bangladesh is not well-developed and there are no clear cut national health policies for a cervical cancer screening program by Pap smear cytology. There is little awareness among the general population, healthcare professionals, and policy makers about cervical cancer prevention by Pap smear cytology. Environmental disasters such as floods, hurricanes, along with other causes of death such as diarrheal diseases, respiratory tract infections, and high maternal mortality concern national policy makers more than the deaths caused by cervical cancer. Therefore, failure of Pap test-based cervical cancer screening in preventing otherwise preventable deaths may be attributed to lack of proper national healthcare policy, limited access to healthcare centers by a major subset of the population, failure of the eligible women to come for screening with follow-up, and last but not the least lack of patient compliance.
Most of the patients included in our study were married when they were in their teens. These patients had increased risk of HPV as there was a biological predisposition of the immature cervix of the adolescent to persistent HPV infection, which augmented the risk of cancer development.[21] Therefore, family planning, sexual education, and HPV vaccination should be targeted toward this early age group. However, information provided in this study will in addition encourage further utilization of Pap smear as a screening method for cervical cancer in peri- / postmenopausal women.
From this study it is evident that unlike in the developed countries, Pap smear cytology-based screening is not well-organized enough in Bangladesh. Those who are being detected by the screening process are the symptomatic ones. The Pap test is done as a part of investigations related to the management of these patients. Therefore, facilities for cytological screening should be extended up to the primary health care level. If possible HPV testing should be included too. All the women who were reported as LSIL / HSIL in our study were counseled and advised for colposcopic biopsy and histopathology. Regrettably, so far, only a very small percentage (34.5%) has undergone biopsy and histopathology. Ours is a hospital-based study and an advanced study under a well-organized screening system, with a large number of cases, is in demand, to reveal the exact statistics of premalignant and malignant cervical lesions, in Bangladesh.
CONCLUSIONS
The present study highlights that women of age 45 years or above harbor the bulk of premalignant and malignant lesions in Pap smears. This signifies that these women are among the under users of cytological screening. Hence, they should be efficiently brought under the cervical cancer screening program.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
No competing interest to declare by any of the authors.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Each author acknowledges that this final version was read and approved. All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author Each author has participated sufficiently in the work and take public responsibility for appropriate portions of the content of this article.
ETHICS STATEMENT BY ALL AUTHORS
This study was conducted with approval from Institutional Review Board (IRB) (or its equivalent) of all the institutions associated with this study as applicable. Authors take responsibility to maintain relevant documentation in this respect.
EDITORIAL / PEER-REVIEW STATEMENT
To ensure integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model(authors are blinded for reviewers and reviewers are blinded for authors)through automatic online system.
The authors would like to thank Dr Arun Kumar Adhikary, PhD, Head % Associate Professor, Department of Microbiology, BGC Trust Medical College, Chandanaish, Chittagong, Bangladesh, for giving the support and valuable suggestions in manuscript preparation.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2011/8/1/8/80527
References
- Heterogeneity of the fibre sequence in subgenus C adenoviruses. J Clin Pathol. 2004;57:612-7.
- [Google Scholar]
- The abnormal pap smear: A rationale for follow up. Can Fam Physician. 1983;29:759-62.
- [Google Scholar]
- Bethesda 2001. Impact on the reporting of gynecologic cytology. Acta Cytol. 2004;48:355-62.
- [Google Scholar]
- The forum group membersThe Bethesda 2001 workshop. The 2001 Bethesda System: Terminology for reporting results of cervical cytology. JAMA. 2002;287:2114-9.
- [Google Scholar]
- ASCUS LSIL Triage Study Group. Qualifiaction of ASCUS. A comparison of equivocal LSIL and equivocal HSIL in cervical cytology in the ASCUS LSIL Triage Study. Am J Clin Pathol. 2001;116:386-94.
- [Google Scholar]
- Viet/American Cervical Cancer Prevention Project.Papanicolaou screening in developing countries: An idea whose time has come. Am J Clin Pathol. 2004;121:315-20.
- [Google Scholar]
- Systems analysis of real-world obstacles to successful cervical cancer prevention in developing countries. Am J Public Health. 2006;96:480-7.
- [Google Scholar]
- Treatment of the patients with abnormal cervical cytology: A “see-and-treat” versus three-step strategy. J Gyecol Oncol. 2009;20:164-8.
- [Google Scholar]
- Changing Spectrum of Squamous Cell Abnormalities Observed on Papanicolaou Smears in Mubarak Al-Kabeer Hospital, Kuwait, over a 13-Year Period. Med Pnic Pract. 2006;15:253-9.
- [Google Scholar]
- Pattern of abnormal Pap smears in developing countries: A report from a large referral hospital in Saudi Arabia using the revised 2001 Bethesda System. Ann Saudi Med. 2007;27:268-72.
- [Google Scholar]
- Premaliganant lesions of the uterine cervix in a large cohort of Israeli Jewish women. Arch Gynecol Obstet. 2004;269:188-91.
- [Google Scholar]
- Profile of Pap smear cytology in the western region of Saudi Arabia. Saudi Med J. 2003;24:1225-9.
- [Google Scholar]
- Cytopathological pattern of cervical Pap smear according to the Bethesda system in Southwestern Saudi Arabia. Saudi Med J. 2005;26:588-92.
- [Google Scholar]
- Cervical Papanicolau smear abnormalities in inner Bronx adolescents: Prevalence, progression, and immune modifiers. Cancer (cancer cytopathology). 1999;87:184-9.
- [Google Scholar]
- Cervical cancer: Evolving prevention strategies for developing countries. Reprod Health Matters. 1995;6:60-71.
- [Google Scholar]
- Sociodemographic factors of Pap smear screening in Taiwan.Taipei Wanhwa District Health Center, Taiwan. Public Health. 1996;110:123-7.
- [Google Scholar]
- Risk of cervical abnormality after age 50 in women with previously negative smears. Br J Cancer. 2009;100:1832-6.
- [Google Scholar]
- Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: A cluster-randomised trial. Lancet. 2007;370:398-406.
- [Google Scholar]
- Different risk factor patterns for high-grade and low-grade intraepithelial lesions on the cervix among HPV positive and HPV-negative young women. Int J Cancer. 1998;76:613.
- [Google Scholar]








