Translate this page into:
Primary orbital mantle cell lymphoma: Flow cytometric immunophenotyping as an adjunct to fine-needle aspiration cytology for diagnosis
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 24-year-old male presented with 4 cm × 5 cm-sized polypoidal orbital mass for 8 years, gradually progressive with proptosis of the right eyeball. There was no lymphadenopathy or hepatosplenomegaly. Computed tomography revealed a homogeneous enhancing soft tissue polypoidal mass in the lateral aspect of the right orbit and pushing the eyeball medially. Fine-needle aspiration cytology (FNAC) was performed from the polypoid orbital mass. The diagnosis was offered after cytomorphologic evaluation and flow cytometric immunophenotyping [Figure 1].
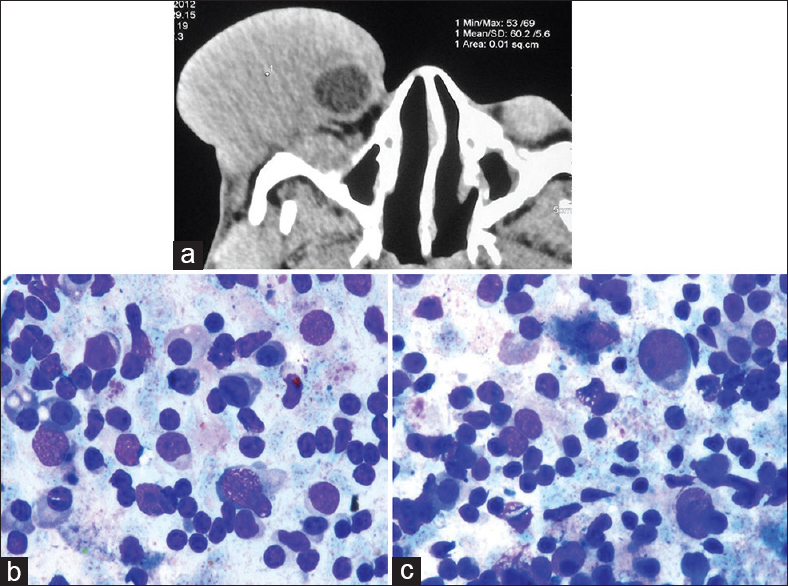
- (a) Computed tomography, axial section showing a homogeneous enhancing soft-tissue swelling in the lateral aspect of the right orbit. A part of eyeball can be seen toward medial aspect; (b and c) Small to medium-sized lymphoid cells with condensed chromatin, inconspicuous nucleoli, and irregular nuclear contours with deep indentations along with many scattered plasma cells (MGG, ×100)
Q1: WHAT IS YOUR INTERPRETATION?
-
Reactive lymphoid proliferation
-
Low-grade non-Hodgkin's lymphoma (NHL)
-
High-grade NHL
-
Hodgkin's lymphoma.
ANSWER
A1: Low-grade NHL [Figure 2].
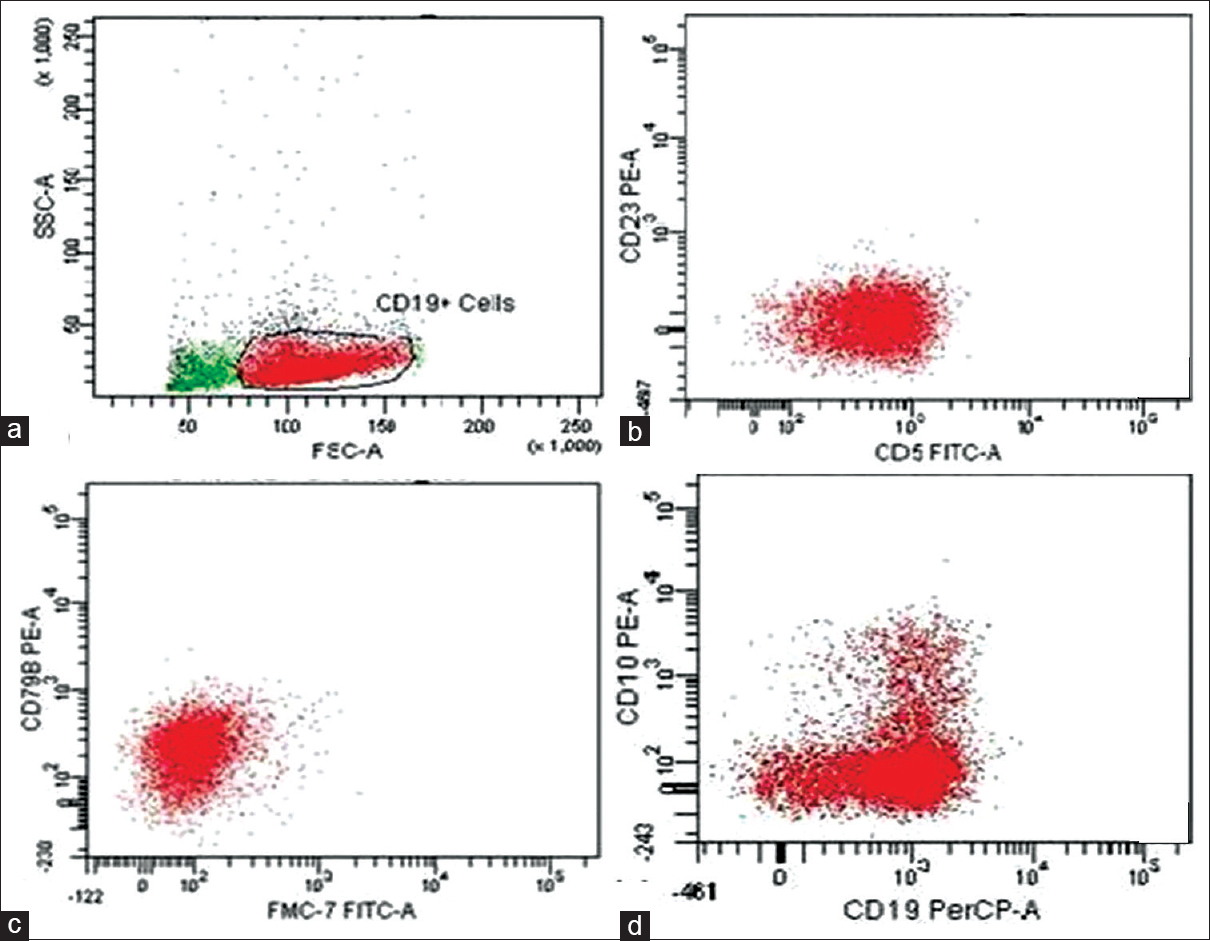
- Flow cytometric immunophenotyping; (a) CD19-positive events were gated for further analysis; (b) Selected CD19-positive population of cells were CD5-positive and negative for CD23; (c) CD19-positive cells were positive for CD79a; (d) CD19-positive cells were negative for CD10. There was clonal proliferation (with lambda light chain restriction) of B-lineage lymphoid cells (CD19-positive) and these cells were also negative for CD23, CD10, CD3, and kappa light chain
Q2: WHAT IS YOUR INTERPRETATION AFTER FLOW CYTOMETRY?
-
Diffuse large B-cell lymphoma
-
Chronic lymphocytic lymphoma
-
Mantle cell lymphoma
-
Hodgkin's lymphoma.
ANSWER
A2: Mantle cell lymphoma.
The correct cytological interpretation is - This is a case of primary mantle cell lymphoma of the orbit.
DISCUSSION
Lymphomas primarily involve the axial lymph node groups; although the NHL may also involve extranodal tissues such as nasopharynx, tonsils, gastrointestinal tract, brain, heart, and skin. Ten percent of systemic lymphomas have orbital involvement; however, in <1% cases, lymphoma develops primarily in the orbit.[1] Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT)-type is a common type of NHL affecting eye and orbit. Mantle cell lymphoma is a rare entity at this site, which is characterized by the presence of small to medium-sized lymphoid cells with irregular nuclear outlines, often cleaved with condensed chromatin, tiny to absent nucleoli, and scanty slightly basophilic cytoplasm. It is a rare subtype of B-cell NHL occurring in an orbital region with only a few reported cases and case series in literature.[2345678] Rasmussen et al.[8] identified 21 patients of mantle cell lymphoma in the orbital and adnexal region comprising 9% of all lymphomas in the ocular region. Elderly males were more commonly affected. The orbit (71%) and eyelids (64%) were the most commonly affected sites. Another report[7] has shown similar results that orbital mantle cell lymphoma has an aggressive clinical course and patients usually present with advanced disease. The present case is a young male with a long history of orbital mass, without any associated systemic findings or peripheral lymphadenopathy. Another case of orbital mantle cell lymphoma has been reported in a 31-year-old female from Nepal, who presenting with orbital swelling of 9-month duration.[9] The various modalities useful for differentiating lymphoproliferative disorders involving orbital region include histopathological examination, immunochemistry, flow cytometry, cytogenetics, and new technologies such as real-time polymerase chain reaction and fluorescence in situ hybridization. The final diagnosis can be given based on combined results of various ancillary techniques. In the present case, FNAC of the orbital mass revealed a population of atypical lymphoid cells having irregular indented nuclei, admixed with plasma cells, histiocytes, and reactive mature lymphocytes. FCI was performed on the aspirated material, which confirmed a clonal population of B lymphoid cells with CD5-positive and CD23-negative cells, the most compatible diagnosis being mantle cell lymphoma. The tumor cells of MALT lymphoma are positive for CD19, CD20, CD79a and negative for CD23; however, they are also negative for CD5, thus differentiating it from mantle cell lymphoma. A definitive diagnosis of mantle cell lymphoma should be offered after demonstration of t(11;14) (q13;q32) translocation or cyclin D1 overexpression, which could not be performed in the present case.
ADDITIONAL CME QUESTIONS
Q3: Which translocation is common in mantle cell lymphoma?
Q4: Mantle cell lymphomas are positive for all of the following, except
-
CD 20
-
CD 5
-
CD 23
-
CD 43.
Q5: The best diagnostic marker for mantle cell lymphoma is to demonstrate
-
Overexpression of p53
-
Beta-catenin expression
-
Bcl-6 expression
-
Overexpression of cyclin D1.
ANSWERS
A3: t(11;14) (q13;q32) translocation.
A4: CD 23; Mantle cell lymphomas are CD23-negative.
A5: Overexpression of cyclin D1.
SUMMARY
Primary orbital mantle cell lymphoma is an uncommon neoplasm. It is valuable to subtype NHL as orbital mantle cell lymphoma has relatively poor prognosis as compared to other more common MALT lymphomas of the same region.[2] FNAC combined with flow cytometry gives rapid and accurate results and can be very useful in directing timely management.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE. Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
ETHICS STATEMENT BY ALL AUTHORS
As this is a quiz case, this case does not require approval from the Institutional Review Board.
LIST OF ABBREVIATIONS (In alphabetic order)
FCI - Flow cytometric immunophenotyping
FNAC - Fine-needle aspiration cytology
H and E - Hematoxylin and eosin
MALT - Mucosa-associated lymphoid tissue
MGG - May–Grünwald–Giemsa
NHL - Non-Hodgkin's lymphoma.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Primary orbital non-Hodgkin's lymphoma – Management and outcome from a single institution. Am Soc Clin Oncol 2002 Abstr. No. 2638
- [Google Scholar]
- Lymphomatous proptosis as a novel feature of mantle cell lymphoma. Leuk Lymphoma. 2006;47:71-5.
- [Google Scholar]
- Lymphoproliferative disease of the ocular adnexa: A clinical and pathologic study with statistical analysis of 69 patients. Ophthal Plast Reconstr Surg. 2005;21:177-88.
- [Google Scholar]
- Orbital and adnexal involvement in systemic non-Hodgkin's lymphoma. Cancer. 1994;73:2395-9.
- [Google Scholar]
- Ocular adnexal lymphomas: Five case presentations and a review of the literature. Surv Ophthalmol. 2002;47:470-90.
- [Google Scholar]
- Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology. 1998;105:1430-41.
- [Google Scholar]
- Mantle cell lymphoma in the orbital and adnexal region. Br J Ophthalmol. 2009;93:1047-51.
- [Google Scholar]
- Mantle cell lymphoma of orbit in a middle aged female – a case report. Nepal Med Coll J. 2010;12:275-6.
- [Google Scholar]







