Translate this page into:
Tuberculous lymphadenitis: Comparison of cytomorphology, Ziehl–Neelsen staining, and rapid mycobacterial culture at a pediatric superspecialty hospital
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
To evaluate and compare the role of Ziehl–Neelsen (ZN) staining and mycobacterial culture in diagnosis of tuberculous lymphadenitis.
Materials and Methods:
A total of 56 fine needle aspirations (FNAs) from patients who were clinically suspected to have tuberculous lymphadenitis were included. Acid-fast Bacilli detection was attempted by ZN staining on smears as well as culture on Middlebrook 7H9 broth. Percentage positivity of both smears and culture was calculated.
Results:
Of the 56 cases, 46 showed cytomorphological features consistent with tuberculosis (TB). The most common pattern was only necrosis in 37 cases followed by necrotizing granulomas in 13 cases. ZN-stained smears were positive in 40 cases while culture was positive in only 27 cases. The highest smear and culture positivity was noted in cases with only necrosis. In six cases, diagnosis of TB was made on culture alone since smear was negative in these cases.
Conclusion:
FNA is a reliable technique for early and accurate diagnosis of tuberculous lymphadenitis in many cases. Mycobacterial culture by newer rapid techniques can assist in bacillary detection in smear-negative cases and also allows for drug sensitivity testing. Hence, culture should be resorted to in such cases.
Keywords
Aspiration cytology
culture
lymphadenitis
tuberculosis
INTRODUCTION
Tuberculosis (TB), a notifiable disease in India, is a major global health problem.[1] TB involves respiratory tract as well as extrapulmonary sites, lymph nodes being most common among the latter.[2] Since TB usually affects superficial lymph nodes, fine needle aspiration (FNA) is established as a simple, less expensive outpatient procedure for obtaining diagnostic material. Diagnosis is made by cytomorphology and Ziehl–Neelsen (ZN) staining for acid-fast Bacilli (AFB). Mycobacterial culture is not done in most cases due to the long time the Bacilli take to grow (6–8 weeks in conventional Lowenstein–Jensen medium and 3–4 weeks in Middlebrook liquid medium).[3]
The present study was aimed at comparing the utility of ZN staining and mycobacterial culture in bacterial detection in cases of suspected tuberculous lymphadenitis.
MATERIALS AND METHODS
The present study included cases of clinically suspected tuberculous lymphadenitis attending our hospital from January 2014 to December 2014, who were referred for FNA cytology (FNAC). In all these cases, FNAC was performed under aseptic conditions using 23G needle with or without suction, as per requirement. A minimum of two smears were prepared in each case – one for Giemsa stain and other for ZN stain. The residual material was submitted for mycobacterial culture.
A record was made of all relevant findings, including site and size of the swelling, multiplicity of lesions, and character of the aspirate. The character was described as caseous for cheesy or yellow-white aspirate, pus for greenish yellow or yellow aspirate, and blood mixed for hemorrhagic material.
The Giemsa- and ZN-stained smears were examined for presence of epithelioid cell granulomas with or without necrosis and presence of AFB, respectively.
For mycobacterial culture, the specimens were digested, decontaminated, and concentrated using N-acetyl-L-cysteine-sodium hydroxide method. Of the suspension thus obtained, 0.5 ml was inoculated into BBL MGIT™ mycobacteria growth indicator tube containing 7 ml of Middlebrook 7H9 broth base and 0.8 ml PANTA antibiotic mixture. These tubes were inoculated at 37°C for 8 weeks, during which the cultures were examined regularly by MicroMGIT Instrument (BD Biosciences, USA) for fluorescence. Tubes generating a reading of ≥14 were labeled as positive, as per the manufacturer’s instructions. Contamination was excluded by ZN staining of smear and sheep blood agar culture from positive tubes. Further, the positive tubes were tested with rapid immunochromatographic test for MPT 64 antigen (SD Bioline, Republic of Korea) to identify the species as Mycobacterium TB complex.
A diagnosis of tuberculous lymphadenitis was confirmed using the following criteria: Presence of epithelioid cell granuloma with necrosis and/or positive AFB on ZN stain and/or positive mycobacterial culture.
RESULTS
The present study included 56 cases of clinically suspected tubercular lymphadenopathy attending the outpatient department of our pediatric superspecialty hospital from January 2014 to December 2014.
Majority (66.1%) of the aspirates were from cervical lymph nodes. Five patients (8.9%) had axillary lymph nodes and seven (12.5%) presented with supraclavicular lymph nodes. A cytological diagnosis suggestive of tuberculous lymphadenitis was given in 46 (82.14%) cases having epithelioid cell granulomas with necrosis and/or AFB. Ten (17.8%) cases were reported as suspicious on the basis of granulomas alone without necrosis or AFB or presence of acute inflammatory cells with necrosis.
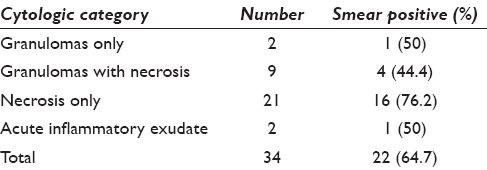
On categorization of cytological smears, six cases had granulomas without necrosis, 13 showed granulomas with necrosis, and 37 had necrosis with or without acute inflammatory cells [Figure 1]. A comparison of positive ZN stain in these categories is given in Table 1.

- Aspirate from a case showing only caseous necrosis (a, Giemsa ×200) with positive (arrow) Ziehl–Neelsen stain (b, ×100). Another case showing epithelioid cell granuloma and necrosis (c, Giemsa ×200). Ziehl–Neelsen stain shows acid-fast Bacillus (arrow) within granulomas (d, ×100)
Mycobacterium TB could be isolated by culture in a total of 27 cases (48.2%). The comparison of ZN stain and culture positivity in various cytological categories is given in Table 2. The highest culture positivity was noted in the cases with mainly necrosis (18 of 27 positive cases) while cases with only granulomas did not yield positive cultures.
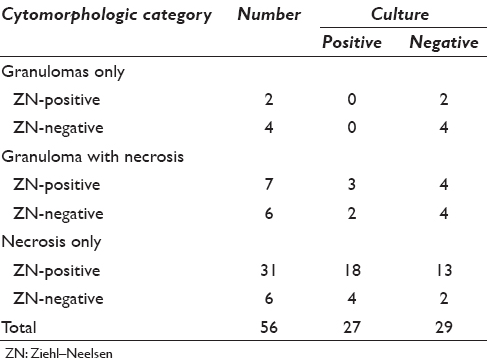
As can be seen from Table 2, six cases (10.7%) were positive by culture but negative on ZN stain (two cases with necrotizing granulomas and four with only necrosis). Adding these to the 40 smear positive cases takes the total confirmed tuberculous cases to 46 of 56 cases (82.14%).
DISCUSSION
TB, a contagious disease caused by Mycobacterium TB, affects respiratory tract as well as extrapulmonary sites. Tuberculous lymphadenitis is the most common form of extrapulmonary TB in regions with high prevalence of mycobacterial infection.[2]
Tissue diagnosis is the mainstay of diagnosis of tuberculous lymphadenitis. For this purpose, FNAC is established as a cheap, simple, rapid, and minimally invasive method to avoid excision biopsy in a large number of cases.[4]
The cytological diagnosis of tuberculous lymphadenitis is usually based upon demonstration of epithelioid cell granulomas with necrosis and/or AFB. Smears with only granulomas without necrosis and AFB need to be clinically correlated with microbiological assessment.[4]
Though culture isolation of the organism is considered the gold standard in most infections, culturing Mycobacterium TB is often not feasible in clinical set up due to the long time taken for culture (6–8 weeks in conventional Lowenstein–Jensen medium, 3–4 weeks in Middlebrook medium).[5]
In the present study, the most common cytological pattern was the presence of necrosis only in 66.1% of cases followed by necrotizing granulomas in 23.2% of cases. This is similar to earlier reports by Nidhi et al.[4] Other studies have reported granulomas with necrosis as the most commonly observed cytological pattern.[6]
The highest AFB positivity was seen in smears with necrosis only (83.7%), similar to results of Nidhi et al., Bezabih et al., Mistry et al., and Dua et al.[2478]
The overall AFB positivity in the present study was 71.4%, which is similar to the rate reported by Nidhi et al. (71%) but higher than other authors such as Mistry et al. (22.9%), Dua et al. (27.1%), and Aggarwal et al. (19.6%).[2489] The frequency of AFB positivity in FNA smears in various studies has ranged from 10% to 70%.[910]
High AFB positivity in our study may be a result of extensive screening done on ZN-stained smear, especially in cases with high cytological suspicion of TB.
Mycobacterium could be isolated only in 27 cases (48.2%) which was lower than the smear ZN positivity. This is in contrast to the earlier studies.[28] This may be explained by two reasons: Extensive screening leading to higher ZN positivity and technical failure during culture or presence of nonculturable Bacilli.[11]
Of note, however, there are the six cases where smear for AFB was negative and culture was positive. Of these six cases, two showed epithelioid cell granulomas with necrosis and TB was the most likely diagnosis, considering the endemicity in our region. In the remaining four cases, smears showed only necrosis, on which confirmed diagnosis of TB was not possible on cytology alone and culture clinched the diagnosis.
CONCLUSION
FNAC combined with microbiological examination of the aspirates is a reliable technique for diagnosis of tuberculous lymphadenitis. Culture should be resorted to in all suspected cases to enhance mycobacterial detection, especially in smear-negative aspirates. In addition, culture provides an opportunity to determine the species as Mycobacterium TB or atypical mycobacterial and also, sensitivity to various antituberculous drugs. This, in turn, assists in appropriate management and disease control.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
SM and RA were involved in FNAC of these patients, data collection, compilation, literature search and critical review of the manuscript. RT and RG were involved in idea generation, reporting of FNAC of these patients, data analysis, writing, and critically reviewing the manuscript. RS and VM helped in microbiological assessment of the samples along with drafting and critical review of the manuscript
ETHICS STATEMENT BY ALL AUTHORS
All the authors declare that they have no conflict of interest to declare.
LIST OF ABBREVIATIONS (In alphabetic order)
AFB - Acid-Fast Bacilli
FNA - Fine Needle Aspiration
FNAC - FNA Cytology
TB - Tuberculosis
ZN - Ziehl-Neelsen.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- A minimum 5.0 ml of sputum improves the sensitivity of acid-fast smear for Mycobacterium tuberculosis. Am J Respir Crit Care Med. 2000;161:1559-62.
- [Google Scholar]
- Efficacy of fine needle aspiration cytology, Ziehl-Neelsen stain and culture (BACTEC) in diagnosis of tuberculous lymphadenitis. Natl J Med Res. 2012;2:77-80.
- [Google Scholar]
- Evaluation of biphasic culture system for mycobacterial isolation from the sputum of patients with pulmonary tuberculosis. Indian J Med Microbiol. 2005;23:111-3.
- [Google Scholar]
- FNAC in tuberculous lymphadenitis: Experience from a tertiary level referral centre. Indian J Tuberc. 2011;58:102-7.
- [Google Scholar]
- Diagnosis of tuberculous lymphadenitis: Combining cytomorphology, microbiology and molecular techniques – A study from Sri Lanka. Indian J Pathol Microbiol. 2008;51:195-7.
- [Google Scholar]
- Critical appraisal of fine needle aspiration cytology in tuberculous lymphadenitis. Acta Cytol. 1992;36:391-4.
- [Google Scholar]
- Fine needle aspiration cytology of suspected tuberculous lymphadenitis. Cytopathology. 2002;13:284-90.
- [Google Scholar]
- Correlation of cytomorphology with AFB positivity by smear and culture in tuberculous lymphadenitis. Indian J Tuberc. 1996;43:81-4.
- [Google Scholar]
- A clinico-bacteriological study of peripheral tuberculous lymphadenitis. J Assoc Physicians India. 2001;49:808-12.
- [Google Scholar]
- Acid fast Bacilli in aspiration smears from tuberculous patients. Ethiop J Health Dev. 2000;14:99-104.
- [Google Scholar]
- Culturability of Mycobacterium tuberculosis cells isolated from murine macrophages: A bacterial growth factor promotes recovery. FEMS Immunol Med Microbiol. 2000;29:233-40.
- [Google Scholar]








