Translate this page into:
Cervical intraepithelial lesions in females attending Women's Health Clinics in Alexandria, Egypt
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Data from Egyptian studies provide widely varying estimates on the prevalence of preinvasive cervical lesions. The aim of this study was to estimate the rate of cervical intraepithelial neoplasia (CIN) in Egyptian women living in Alexandria to clarify the need for implementing a national organized screening program and a vaccination program in our community.
Materials and Methods:
The study was conducted over a 6 years period and covered the different socioeconomic levels to have a representative sample for women living in Alexandria. All women included did not have any cervical disorder related complaints. Conventional Pap smears were obtained and diagnosed using the Bethesda system. Women with abnormal Pap smears were managed according to the 2006 consensus guidelines within the available facilities. Persistent abnormal cytological results were referred for colposcopic biopsy. Histological results were grouped into: Reactive changes, CIN 1, CIN 2/CIN 3 and adenocarcinoma in-situ (AIS).
Results:
Out of the 6173 smears included in the study 6072 (98.36%) were normal and only 101 (1.63%) were abnormal. After colposcopic biopsies, 0.08% had CIN 1, 0.03% had CIN 2, 3 and 0.01% had AIS.
Conclusion:
We concluded that cervical cancer screening programs, although life-saving for a number of women, are not a sufficiently high priority in our community. Money for national health screening programs should preferably be directed more towards recruiting women for breast cancer screening, since breast cancer accounts for about 33% of all female cancers in Egypt ranking number one, while cervical cancer ranks number 13.
Keywords
Cervical cancer
cervical intraepithelial neoplasia
Egypt
priority
screening
INTRODUCTION
Cervical cancer is the fourth most common cancer affecting women worldwide, after breast, colorectal, and lung cancers. It is also the fourth most common cause of cancer death in women worldwide.[1]
In Egypt, according to the World Health Organization (WHO) most recent estimates, every year 866 women are diagnosed with cervical cancer and 373 die from the disease. Cervical cancer ranks as the 13th most frequent cancer among women in Egypt and the 10th most frequent cancer among women between 15 and 44 years of age.[2] Data from Egyptian studies provide estimates on the prevalence of high-grade preinvasive cervical lesions ranging from 0.3% to 0.5%.[34]
The most important risk factors for cervical cancer are the persistence of an oncogenic human papillomavirus (HPV) infection and a lack of timely screening.[567] One of the most important research priorities involves identifying strategies to increase screening coverage in unscreened or under-screened women, in whom a significant proportion of invasive cervical cancers occur.[8]
The aim of this study was to estimate the rate of cervical intraepithelial lesions in Egyptian women living in Alexandria in an attempt to clarify the need for and the priority of implementing a national organized screening program and a vaccination program in our community.
MATERIALS AND METHODS
The study protocol was approved by the Institutional Review Board of the University of Alexandria. The research team relied on data of a highly utilized tertiary center (the Alexandria Regional Centre for Women's Health and Development [ARC]) and three major obstetrics and gynecology hospitals in Alexandria as well as three screening programs in the remote and less privileged areas to insure the coverage of all socioeconomic levels in order to have a representative sample for women living in Alexandria. All women included in the study were apparently healthy and did not have any cervical disorder-related complaints.
Over a 6 years and 3 months-time period (from September 2007 to December 2013), 6234 cervical Pap smears were examined at the ARC. Of these, 3434 samples were collected from patients attending the ARC gynecology clinics as a part of a general health care screening program that provides Pap tests, mammograms, dual-energy X-ray absorptiometry (DEXA) scans as well as certain laboratory tests. This program was implemented from day 1 in the center as it was one of its main objectives. Invitation of the women to the screening program was done through posters, brochures and lectures in social clubs. Another 1400 samples were collected from women participating in three screening projects (one in 2008, another one in 2010 and a third-one in 2013) involving the far and poor districts of the city of Alexandria, after obtaining their consents. The remaining 1400 samples were collected from the clinics of three major obstetrics and gynecology hospitals in Alexandria, from women with noncervical complaints or seeking contraceptive intrauterine device application. All Pap smears done at the ARC and those of the three screening projects were examined by the first author. The smears done at the clinics of the three obstetrics and gynecology hospitals were examined preliminary by a different pathologist and any suspicious smear was reviewed by the first author.
One of the important prerequisites for inclusion in the present study was the absence of a cervical complaint. Of the 6234 women screened, 34 were excluded from the study because they were non-Egyptians. Another 27 cases were excluded because 24 of them had unsatisfactory smears due to excess polymorphonuclear leucocytes (PMLs) or excess blood and we failed to recall them for repetition of the smears. The remaining 3 cases had a diagnosis of atypical squamous cells of undetermined significance (ASCUS) but did not come back on recall. All other smears that were unsatisfactory at the first evaluation were repeated again after treatment of inflammation or after avoiding the bleeding period of the month and by minimizing traumatization to the cervix during sampling. Postmenopausal women with scanty or inflamed smears that were difficult to interpret were given a course of local estrogen cream for 10 days. Then, the smears were repeated. Patients with abnormal Pap smears were contacted 1-week later and asked to return to the clinic either for a repeat cytology or for colposcopy.
Primary care practitioners and nurses were invited to attend lectures and training courses at the ARC on cervical smear sampling, with a special emphasis on the transformation zone anatomy and on the importance of proper labeling and immediate fixation of the smears.
All screened women were asked to fill in a questionnaire with the help of the attending nurse. The questionnaire included their backgrounds and relative risk factors including socioeconomic characteristics (education, occupation, family income per month), marital status, menstrual, gynecologic and obstetric history as well as the use of contraception. Accordingly women involved in the study were stratified into three socioeconomic strata (SES): Upper, middle and low.
Sample collection for pathological study
Conventional Pap smears were obtained by first sampling the ectocervix using an Ayre spatula and spreading the sample on a glass slide with immediate fixation. Then the endocervix was sampled with a cytobrush, smeared on a separate slide and immediately fixed. Fixation was done using 95% ethyl alcohol. The Pap smears were diagnosed using the Bethesda system (2004).[9]
Whenever indicated, persistent abnormal cytological results were referred for colposcopy. All colposcopies were performed by the second author after obtaining the consents of the patients. Biopsies were fixed in 10% buffered formalin for 24 h and then were processed for paraffin embedding and were stained with hematoxylin and Eosin (H and E). Serial sections from each biopsy were classified according to the WHO criteria for cervical neoplasia.[10]
Statistical analysis
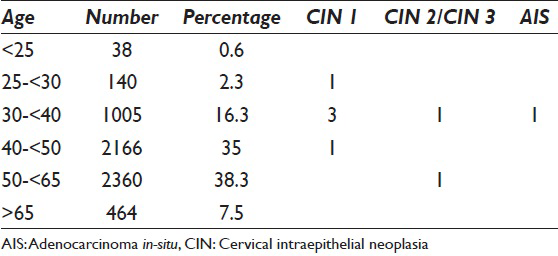
Lesions were grouped according to cytological findings into: Negative for intraepithelial lesion or malignancy (NILM), ASCUS, atypical squamous cells cannot exclude HSIL (ASC-H), low-grade squamous intraepithelial lesion (LSIL), high grade squamous intraepithelial lesion (HSIL), squamous cell carcinoma (SCC) and atypical glandular cells (AGCs). Following biopsy, histological results were grouped into: Reactive changes, cervical intraepithelial neoplasia 1 (CIN 1), CIN 2/CIN 3, adenocarcinoma in-situ (AIS) and invasive SCC. According to the age, patients were classified into six groups (<25, 25–<30, 30–<40, 40–<50, 50–<65 and > 65).
Management of patients with cytological abnormalities
We tried to manage the women with abnormal Pap smears according to the 2006 consensus guidelines[11] as much as possible, within the limits of available and affordable resources.
Women with atypical squamous cells of undetermined significance
We did not have options for choosing between different strategies for triage of women with a diagnosis of ASCUS as HPV testing is not a routine in our center due to financial limitations. We relied on the available tests, which are repeating conventional Pap smear followed by colposcopy and biopsy whenever indicated. Repeat cervical cytologic testing was performed at 6-month intervals until two consecutive “NILM” results were obtained. Colposcopy was performed for women with ASCUS or greater cytologicabnormality on a repeat test.
Women with ASC-H, were referred for colposcopic evaluation.
Women with LSIL, were also referred for colposcopic evaluation.
Women with HSIL, were referred for colposcopy with endocervical assessment and then if necessary loop electrosurgical excision.
In women with atypical glandular cells
Colposcopy with endocervical sampling was done for women with all subcategories of AGC. Endometrial sampling was done in conjunction with colposcopy and endocervical sampling in women 35 years and older with all subcategories of AGCs. Loop electrosurgical excision procedure (LEEP) was done in indicated cases.
RESULTS
The total number of Pap smears included in the study is 6173. Of those 6173 smears 6072 (98.36%) were normal, and only 101 (1.63%) were abnormal.
-
Sixty-one smears were initially categorized as ASC-US. All of them had a repeat smear after 6–7 months. 45 cases were NILM. The remaining 16 cases had persistent ASC-US after another Pap smear at a 6-month interval. These 16 cases underwent colposcopic biopsies. The biopsy showed immature squamous metaplasia and atypia of repair in 15 cases and CIN 1 in 1 case
-
Seven cases were initially categorized as ASC-H [Figure 1a]. All of them underwent colposcopic biopsies. The biopsy revealed immature squamous metaplasia and atypia of repair in 6 cases and CIN 2/CIN 3 in 1 case [Figure 1b]. LEEP was done for this latter case and no invasion was detected
-
Six cases were initially categorized as LSIL. All of them underwent colposcopic biopsies. The biopsy revealed atypia of repair in 2 cases and CIN 1 in 4 cases
-
One case was categorized as HSIL [Figure 2a]. She underwent colposcopic biopsy. The biopsy showed CIN 2/CIN 3 [Figure 2b]. LEEP was done for her and no invasion was detected
-
Twenty-six cases were initially categorized as AGC (including atypical endocervical cells, atypical endometrial cells and AGC not otherwise specified). All of them underwent colposcopy with endocervical sampling and 22 had additional endometrial evaluation after D and C (20 patients above 35 years and 2 patients below 35 years but with intermenstrual bleeding). Histopathological examination revealed endocervical polyps and atypia of inflammation and repair in 22 cases, endometrial hyperplasia in 3 cases (one of them with atypia) and cervical AIS in 1 case [Figure 3a and b]. This latter case was managed by cold knife cone excision and no invasion was detected
-
Nine women of ≥40 years had endometrial cells in their Pap smears. 6 of them were complaining of intermenstrual or postmenopausal bleeding. All of them underwent D and C. Histopathology revealed endometrial hyperplasia in 6 of them and disordered proliferative endometrium in three of them.

- (a) A smear categorized as atypical squamous cells cannot exclude high grade squamous intraepithelial lesion (ASC-H). In this field a cell is identified with raised nucleocytoplasmic ratio and coarse chromatin. Few similar cells were scattered in other areas of the smear (Pap stain, ×400). (b) Histologic section of the case seen in Figure 1a showing a highgrade squamous intraepithelial lesion. Nuclei throughout the lower 2/3 of the epithelium show a coarse chromatin pattern and numerous abnormal mitotic figures. (H and E, ×400)
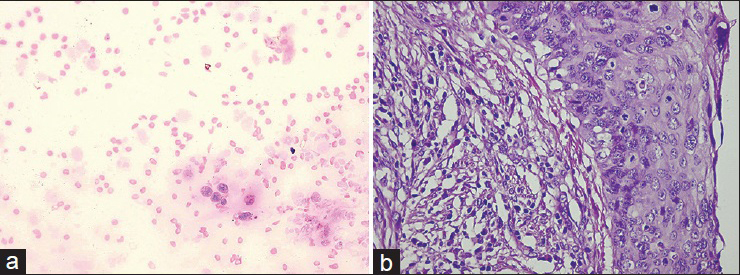
- (a) A smear categorized as high grade squamous intraepithelial lesion. Isolated dysplastic cells with a high nuclear to cytoplasmic ratio. Nuclei are greatly enlarged, vary in size and shape, and contain hyperchromatic, coarsely granular clumped chromatin (Pap stain, ×400). (b) Histologic section of the case seen in Figure 2a showing a high-grade squamous intraepithelial lesion. There is lack of surface maturation. Nuclei throughout most of the thickness of the epithelium show pleomorphism, membrane irregularities and coarse chromatin pattern together with numerous mitotic figures, of which many are abnormal. (H and E, ×400)

- (a) A smear categorized as atypical endocervical cells. A cluster of endocervical cells with enlarged nuclei, nuclear hyperchromasia and coarse chromatin (Pap stain, ×400). (b) Histologic section of the case seen in Figure 3a showing an endocervical adenocarcinoma in-situ. Intact endocervical gland lined by pseudostratified glandular cells with enlarged, elongated, hyperchromatic nuclei. A gland-in-gland arrangement is noted. Numerous mitotic figures and apoptotic bodies are seen. (H and E, ×400)
The age of the screened women and the associated lesions are shown in Table 1.
Distribution of cytological and histological epithelial abnormalities according to socioeconomic strata
Out of the 6173 women included in the study, 3309 were classified as high and middle socioeconomic classes, and 2864 were classified as a low socioeconomic class. Characteristically women of low SES showed a high rate of unsatisfactory smears (560 smears, 19.5%) due to excess inflammatory exudate and PMLs as compared to 123 smears (3.7%) from women of high and middle SES. All unsatisfactory smears of women included in the study were repeated after treatment of cervicitis.
Table 2 summarizes the epithelial abnormalities detected according to the socioeconomic status of the women studied.

DISCUSSION
This study was aimed at clarifying whether organized cervical cancer screening and vaccination programs are a priority in our community or not, through the estimation of the frequency of preneoplastic lesions in women from Alexandria. Similar studies were previously done in the governorates of Cairo[3] and Ismailia[4] but this is the first one in the city of Alexandria.
Our study included 6173 women of different ages and of varying social and educational standards. Abnormal smears were found in 101 (1.63%) of them. On colposcopic biopsies, CIN 1 was found in 5 cases (0.08%), CIN 2, 3 in 2 cases (0.03%) and AIS in 1 case (0.01%).
Women initially diagnosed with ASCUS in this series were 0.98% of the total screened women. Out of the 16 biopsied women with ASCUS, one showed a low-grade intraepithelial lesion while the rest showed immature squamous metaplasia and atypia of repair. It was previously reported that a cytological result of ASC is the least reproducible of all cytologic categories.[123] The prevalence of invasive cancer is reported to be 0.1–0.2% in women with ASCUS.[14] In our series, none of the ASCUS cases showed an invasive carcinoma. The prevalence of CIN 2, 3 is reported by the American Society for Colposcopy and Cervical Pathology, to be higher among women with ASC-H than women with ASCUS.[11] This was also true in our series where 14.2% of women with ASC-H had a high-grade lesion on colposcopic biopsy, whereas none of those with ASCUS had a high-grade lesion on biopsy.
In the present study, LSIL constituted 0.09% of screened women. In the US, in 2003, the mean LSIL reporting rate was 2.9% for liquid-based specimens.[15] The prevalence of CIN 2 or greater identified at initial colposcopy among women with LSIL is reported to vary from 12 to 16%.[167] In our study, however, none of those initially diagnosed with LSIL showed a high-grade lesion on colposcopic biopsy. This discrepancy may be attributed to the small number (6 cases) of women with LSIL in the present study.
The frequency of HSIL in the screened women in our series was 0.016%, which is a much lower rate than the one reported in the US laboratories (0.7%).[16] AGC, in the present study, constituted 0.4% of all screened women, which is concordant with the mean reporting rate in the United States in 2003.[16] Out of the 26 cases of AGC that were biopsied, only 1 case showed cervical AIS. Recent series have reported 9–38% of women with AGC have significant neoplasia.[181920]
Overall, 0.08% of the screened women in our study were found to have CIN 1, 0.03% were found to have CIN 2, 3 and 0.01% were found to have AIS. This is a lower incidence than that reported in the US population where an observational cohort study was conducted in 2004 and the annual incidence of CIN across all female enrollees was 0.27%.[21] Similarly in a more recent study among the US population, an annual incidence of 0.16% for CIN 1 and of 0.12% for CIN 2, 3 was reported.[22] Although data from previous studies on Egyptian females provide higher estimates on the prevalence of high-grade preinvasive cervical lesions ranging from 0.3%[3] to 0.5%,[4] still these prevalence rates are considered low for a population that was not previously screened. The higher estimates in these two Egyptian studies as compared to ours may be attributed to the fact they included all the females recruited regardless they had cervical complaints or not. Some of them even had gross abnormalities like warts and polyps. In our study, however, all women presenting with a cervical disorder were excluded from the study.
The Middle East Cancer Consortium (MECC) reported a 0.027% prevalence rate for cervical cancer in Egyptian women.[23] Among the MECC countries, the highest age-standardized rate of cervical cancer was observed in Israeli Jews (5.3), followed by Cypriots (3.7), Egyptians (2.7), Jordanians (2.6), and Israeli Arabs (2.5). The US surveillance, epidemiology and end results (SEER) rate (7.0) was higher than for any MECC registry. This could be attributed mainly to differences in sexual activity. According to the Gharbiah population-based cancer registry (as part of MECC), an important observation is the very low frequency of cancer of the cervix uteri (not shown in the chart of the more frequent types of cancer). It was only shown on the charts of the females aged 60+, thus constituting 6% of the diagnosed cancers of females in this age group.[24]
This low incidence of cervical intraepithelial lesions and cervical cancer in Egypt could be attributed to many factors, such as sexual behavior, male circumcision, and religious culture. The sexual behavior is a potent modifier of the cervical cancer risk in different countries. Women in our country tend to remain monogamous unless they are remarried due to divorce or death of the husband. Extramarital relationships are rare in most social standards due to strong religious beliefs. Epidemiological studies investigating risk factors for HPV infection have clearly and consistently shown that the key determinants of infection in women are: The number of sexual partners, the age at which sexual intercourse was initiated, and the likelihood that at least 1 sexual partner was an HPV carrier as estimated by his sexual behavior patterns.[2526] These aforementioned studies have established that the risk of cervical cancer for a given woman is predictable from the sexual behavior of her husband or sexual partner as much as from her own sexual behavior. In populations where female monogamy is predominant, female sex workers play an important role in the maintenance and transmission of HPV infections. The lifetime number of sexual partners of men, along with having prostitutes as sexual partners, are key determinants of cervical cancer risk for their wives.[27] Fortunately in our country, although prostitution exists, it is done on a very limited scale as it is an illegal service that is, prohibited by law. Accused people can be sentenced to many years in prison.
The significance of male circumcision in lowering the incidence of cervical cancer was emphasized in several studies; In a study of 5000 cervical cancer cases in Madras between 1982 and 1990, the incidence of cervical cancer was low among Muslim women compared to Hindu and Christian women,[28] and several other studies in India came out with the same conclusion.[2930] Drain et al. evaluated the relationships between male circumcision prevalence and seven infectious diseases using country-specific data among 118 developing countries. They used multivariate linear regression and found that male circumcision was significantly associated with lower cervical cancer incidence.[31] A meta-analysis by Bosch et al.,[32] published in 2009 of 14 studies found that after adjustment for age at first intercourse, lifetime number of sexual partners, and other potential confounders, circumcised men were about 3 times less likely to harbor HPV in their penis than did uncircumcised men (odds ratio 0.37, 95% confidence interval 0.16–0.85). Within the same study data, they found strong associations in the three key steps occurring from male circumcision to cervical cancer development: Male circumcision reducing the risk of penile HPV, penile HPV increasing the risk of cervical HPV and cervical HPV increasing the risk of cervical cancer. Thus, male circumcision in our country can be considered an important factor that influences the risk of HPV acquisition and transmission as well as of cervical cancer development.
The target population should be defined in terms of age. In our study, none of the screened females below the age of 25 years had an epithelial abnormality. Therefore screening before this age may not be cost-effective in our community. According to the American Society for Colposcopy and Cervical Pathology cervical cancer screening should begin at age 21 years.[8] Women under the age of 21 should not be screened regardless of the age of sexual initiation or other risk factors.[33] This is because cervical cancer is rare in adolescents and young women[34] and may not be prevented by cytology screening.[35]
Most women with cervical cancer are diagnosed before the age of 50; according to SEER stat fact sheets, from 2006 to 2010, the median age of women diagnosed with cervical cancer was 49 years.[36] However, older women remain at risk. More than 20% of new cases are diagnosed in women over 65.[37] In all MECC countries and US SEER, the proportion of cervical cancer diagnosed under the age of 30 years was low. However, the proportion in the MECC registries (about 2%) did appear to be lower than in US SEER (6.4%). Furthermore in the MECC countries the highest percentages of cases were in the age group 30–49 years, except in Egypt, where over half the cases were in females aged 50–69 years, compared with 36.5% of those aged 30–49 years.[23] In the study by Hammad et al., the mean age for CIN was 44.23 years while that for cervical cancer was 54.32.[3]
Previous studies[38394041] have shown that in industrialized and developing countries an inverse correlation exists between socioeconomic status and the incidence of cervical cancer. In this study, although a slightly increased incidence of cervical epithelial abnormalities was noted in women from low SES, this difference was not statistically significant. This could be due to the relatively small number of overall epithelial abnormalities detected in the study. This slightly increased risk of cervical epithelial abnormalities in women from low SES in our population may be attributed partly to the significantly higher parity among noneducated women. Another factor that might have an impact is that 22.4% of husbands of women of low SES in the present study have more than one wife as compared to 2.1% only of husbands in the high and middle SES.
Implementing screening programs in Egypt could be difficult because at present only few centers have the complete health services needed for these programs. In each of the 27 governorates at least three such centers are required. In our center we do cytology, colposcopy, histopathology as well as cryosurgery and LEEP, so the woman with a cytological abnormality is followed up, undergoes colposcopy and biopsy if recommended, and if the abnormality is confirmed, she receives the relevant treatment. If the patient needs a major surgery, she is referred to a hospital.
In the Netherlands, the HPV vaccine was found to be not cost-effective even under favorable assumptions.[42] Therefore, in our country it should not have a priority among more endemic diseases and the diseases with higher incidence and mortality.
The abnormal cervical cytological prevalence rate in our study is lower than rates from many other areas of the world. Therefore, although organized screening programs would be an attractive opportunity for Egyptian women because they could be life saving for many of them, the results of this study should be presented to the policy makers to make up their priorities. Nevertheless, we should aim at training all primary health care physicians on proper cervical inspection, on the necessity of sampling any abnormalities as well as the proper way to take a cervical smear with immediate fixation.
Similarly, HPV vaccination should not be one of the priorities in our country. Benefits should be weighed against costs. A large budget is urgently needed for screening and managing other major health problems in the country as chronic HCV and hepatocellular carcinoma as well as breast cancer.
CONCLUSION
Cervical cancer screening programs are not a sufficiently high priority in our community. Money for national health screening programs should preferably be directed more toward recruiting women for breast cancer screening rather that for cervical cancer screening, since breast cancer accounts for about 33% of all female cancers in Egypt ranking number one,[43] while cervical cancer ranks number 13.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors have participated sufficiently in the conception and design of this work or the analysis and interpretation of the data, as well as the writing of the manuscript, to take public responsibility for it.
-
Mona Abdel Hadi examined the pap smears and biopsies, reviewed the literature and wrote the manuscript
-
Adel Khalaf performed the pap smears, the colposcopic biopsies and the minor surgical procedures
-
Hanaa Aboulkassem examined the patients and performed the pap smears
-
Noha Naeem examined the patients and performed the pap smears
-
Mohamed Abdelbaqy designed the study, collected and analysed the data
-
Hassan Sallam organized the study, supervised the gynecological procedures and critically revised the manuscript.
ETHICS STATEMENT BY ALL AUTHORS
The study protocol was approved by the Institutional Review Board of the University of Alexandria.
LIST OF ABBREVIATIONS
CIN = Cervical Intraepithelial Neoplasia
AIS = Adenocarcinoma in-situ
WHO = World Health Organization
HPV = Human Papillomavirus
DEXA = Dual-Energy X-ray Absorptiometry
PMLs = Polymorphonuclear Leucocytes
ASCUS = Atypical Squamous Cells of Undetermined Significance
SES = Socioeconomic Strata
NILM = Negative for Intraepithelial Lesion or Malignancy
LSIL = Low-grade Squamous Intraepithelial lesion
HSIL = High Grade Squamous Intraepithelial Lesion
SCC = Squamous Cell Carcinoma
AGC = Atypical Glandular Cell
LEEP = Loop Electrosurgical Excision Procedure
MECC = Middle East Cancer Consortium
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://www.globocan.iarc.fr
- [Google Scholar]
- Human Papillomavirus and Related Cancers, Fact Sheet. ICO HPV Information Centre Institut Català d’Oncologia. 2013. Available from: htpp://www.hpvcentre.net/statistics/reports/EGY
- [Google Scholar]
- Low prevalence of cervical intraepithelial neoplasia among Egyptian females. Gynecol Oncol. 1987;28:300-4.
- [Google Scholar]
- Prevalence of cervical neoplastic lesions and Human Papilloma Virus infection in Egypt: National Cervical Cancer Screening Project. Infect Agent Cancer. 2007;2:12.
- [Google Scholar]
- Human papilloma virus and cervical screening. Curr Opin Obstet Gynecol. 2003;15:473-7.
- [Google Scholar]
- Women's knowledge of Pap smears, risk factors for cervical cancer, and cervical cancer. J Obstet Gynecol Neonatal Nurs. 2001;30:299-305.
- [Google Scholar]
- Sexual behavior, human papillomavirus type 16 (HPV 16) infection, and HPV 16 seropositivity. Sex Transm Dis. 2002;29:182-7.
- [Google Scholar]
- American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis. 2012;16:175-204.
- [Google Scholar]
- The Bethesda System for Reporting Cervical Cytology. (2nd ed). New York: Springer-Verlag; 2004.
- [Google Scholar]
- Tumours of the uterine cervix. In: World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Breast and Female Genital Organs. Lyon: IARC Press; 2003. p. :259-89.
- [Google Scholar]
- American Society for Colposcopy and Cervical Pathology--sponsored Consensus Conference. 2006 consensus guidelines for the management of women with abnormal cervical cancer screening tests. Am J Obstet Gynecol. 2007;197:346-55.
- [Google Scholar]
- Interlaboratory reproducibility of atypical squamous cells of undetermined significance report: A national survey. Cytopathology. 2003;14:263-8.
- [Google Scholar]
- Smears diagnosed as ASCUS: Interobserver variation and follow-up. Diagn Cytopathol. 2001;25:138-40.
- [Google Scholar]
- Follow-up of abnormal gynecologic cytology: A college of American pathologists Q-probes study of 16132 cases from 306 laboratories. Arch Pathol Lab Med. 2000;124:665-71.
- [Google Scholar]
- Bethesda 2001 implementation and reporting rates: 2003 practices of participants in the College of American Pathologists Interlaboratory Comparison Program in Cervicovaginal Cytology. Arch Pathol Lab Med. 2004;128:1224-9.
- [Google Scholar]
- A randomized trial on the management of low-grade squamous intraepithelial lesion cytology interpretations. Am J Obstet Gynecol. 2003;188:1393-400.
- [Google Scholar]
- Cytologic-histologic correlation of screening and diagnostic Papanicolaou tests. Diagn Cytopathol. 2006;34:503-6.
- [Google Scholar]
- Dysplasia associated with atypical glandular cells on cervical cytology. Obstet Gynecol. 2005;105:494-500.
- [Google Scholar]
- Rate of pathology from atypical glandular cell Pap tests classified by the Bethesda 2001 nomenclature. Obstet Gynecol. 2006;107:1285-91.
- [Google Scholar]
- Human papillomavirus DNA detection and histological findings in women referred for atypical glandular cells or adenocarcinoma in situ in their Pap smears. Gynecol Oncol. 2004;95:618-23.
- [Google Scholar]
- Diagnoses and outcomes in cervical cancer screening: A population-based study. Am J Obstet Gynecol. 2004;191:105-13.
- [Google Scholar]
- Incidence and costs of cervical intraepithelial neoplasia in a US commercially insured population. J Low Genit Tract Dis. 2010;14:29-36.
- [Google Scholar]
- Cervical and corpus uterine cancer. In: Freedman LS, Edwards BK, Ries LA, Young JL, eds. Cancer Incidence in Four Member Countries (Cyprus, Egypt, Israel, and Jordan) of the Middle East Cancer Consortium (MECC) Compared with US SEER. Bethesda, MD: National Cancer Institute, NIH Pub. No. 06.5873; 2005. p. :83-90.
- [Google Scholar]
- Cancer in Egypt, Gharbiah. In: Triennial Report of 2000-2002. Egypt: Gharbiah Population-Based Cancer Registry; 2007.
- [Google Scholar]
- High-risk human papillomavirus is sexually transmitted: Evidence from a follow-up study of virgins starting sexual activity (intercourse) Cancer Epidemiol Biomarkers Prev. 2001;10:101-6.
- [Google Scholar]
- Prevalence of penile human papillomavirus DNA in husbands of women with and without cervical neoplasia: A study in Spain and Colombia. J Infect Dis. 1997;176:353-61.
- [Google Scholar]
- The epidemiology of human papillomavirus infection and its association with cervical cancer. Int J Gynecol Obstet. 2006;94 Suppl 1:S8-21.
- [Google Scholar]
- Association between cervical and penile cancers in Madras, India. Acta Oncol. 1993;32:617-20.
- [Google Scholar]
- Role of male behavior in cervical carcinogenesis among women with one lifetime sexual partner. Cancer. 1993;72:1666-9.
- [Google Scholar]
- Epidemiological trend in the distribution of cancer in Kashmir Valley. J Epidemiol Community Health. 1993;47:290-2.
- [Google Scholar]
- Male circumcision, religion, and infectious diseases: An ecologic analysis of 118 developing countries. BMC Infect Dis. 2006;6:172.
- [Google Scholar]
- Male circumcision, human papillomavirus and cervical cancer: From evidence to intervention. J Fam Plann Reprod Health Care. 2009;35:5-7.
- [Google Scholar]
- Practice improvement in cervical screening and management (PICSM): Symposium on management of cervical abnormalities in adolescents and young women. J Low Genit Tract Dis. 2010;14:73-80.
- [Google Scholar]
- Practice improvement in cervical screening and management: Symposium on management of cervical abnormalities in adolescents and young women. J Low Genit Tract Dis. 2010;14:238-340.
- [Google Scholar]
- Effectiveness of cervical screening with age: Population based case-control study of prospectively recorded data. BMJ. 2009;339:b2968.
- [Google Scholar]
- Surveillance Epidemiological and End Results (SEER). SEER Stat Fact Sheets: Cervix Uteri. Bethesda, MD: National Cancer Institute; 2013. Available from: http://www.seer.cancer.gov/statfacts/html/cervix.html
- [Google Scholar]
- American Cancer Society (ACS). What are the key statistics about cervical cancer? Atlanta: American Cancer Society; 2013. Available from: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-key-statistics
- [Google Scholar]
- Socioeconomic differences in cervical cancer: Two case-control studies in Colombia and Spain. Am J Public Health. 1996;86:1532-8.
- [Google Scholar]
- Socioeconomic differences in cancer incidence and mortality. IARC Sci Publ. 1997;138:65-176.
- [Google Scholar]
- Social differences in sexual behaviour and cervical cancer. IARC Sci Publ. 1997;138:309-17.
- [Google Scholar]
- Associations between community income and cancer incidence in Canada and the United States. Cancer. 2000;89:901-12.
- [Google Scholar]
- Cost-effectiveness analysis of human papillomavirus vaccination in the Netherlands. J Natl Cancer Inst. 2009;101:1083-92.
- [Google Scholar]
- ECR Today 2012. Daily News from Europe's Leading Imaging Congress; Sunday 04 March 2012. Available from: http://www.myesr.org/html/img/pool/ECR_Today_2012_Sunday.pdf
- [Google Scholar]








