Translate this page into:
A case of painful ankle swelling: Cytomorphological clues and pitfalls
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 45-year-old female presented with complaints of painful left ankle swelling for 2½ years following a trivial trauma in the left ankle. There was no fever or chronic cough. There was no discharge or sinus formation. X-ray of the left ankle joint and foot revealed osteoporosis with absorption of the left talus neck. Figures 1a and b show the cytomorphological features of fine-needle aspirate done under ultrasound guidance. Ziehl–Neelsen (ZN) stain for acid-fast bacilli (AFB) and periodic acid–Schiff (PAS) stain for fungi were negative.
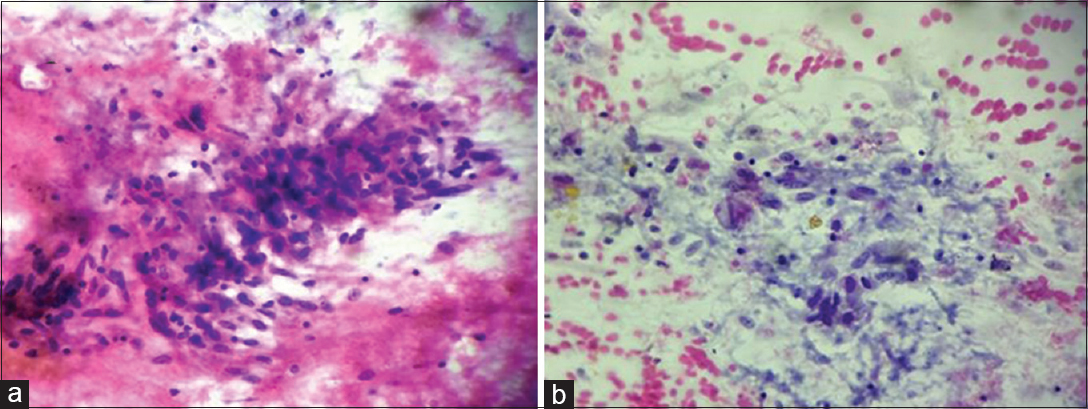
- (a) Smears showed epithelioid cell granuloma in a necrotic background (May-Grünwald-Giemsa, ×400). (b) Smears showed epithelioid cell collection (Papanicolaou, ×400)
QUESTION
Q1: What is your interpretation?
-
Sarcoidosis
-
Tuberculosis
-
Fungal infections
-
Eosinophilic granuloma.
ANSWER
b. Tuberculosis.
Fine-needle aspiration cytology is a simple and safe outdoor procedure for the diagnosis of osteoarticular tuberculosis.[12] The nature of aspirates in osteoarticular tuberculosis is of three types: blood mixed particles, caseous material, and pus.[1] Cytomorphological smears show epithelioid cell granulomas, scattered multinucleated and Langhans’ giant cells in a background of necrosis, and degenerated neutrophils.[1] Osteoarticular tuberculosis is a paucibacillary disease.[34] Hence, it is difficult to demonstrate AFB and culture is rarely positive in these lesions.[34]
Cytomorphologically, the differential diagnosis of osteoarticular granulomatous lesions includes sarcoidosis, eosinophilic granuloma, and fungal infections.[1] Sarcoidosis shows lymphocyte poor naked granulomas in a clean background without any necrosis or other inflammatory cells.[15] Various inclusions may be seen within the giant cells. Eosinophilic granuloma is characterized by Langerhans’ cells having coffee-bean nuclei with nuclear groves, prominence of eosinophils, and absence of necrosis.[16] Identification of a specific fungus is required for diagnosis of fungal infections.[17]
Features favoring osteoarticular tuberculosis over other differential diagnoses are listed as follows:
-
Presence of epithelioid cell granulomas
-
Degenerated inflammatory cells
-
Dead bony fragments
-
Necrotic background.
FURTHER WORK-UP OF THE PRESENT CASE
Erythrocyte sedimentation rate was elevated with 56 mm at the end of the first hour. Her chest X-ray was within normal limits. Computed tomography (CT) scan showed multiple irregular lytic foci involving the talar, navicular, part of calcaneum, and lateral cuneiform with surrounding edema with coke-like sequestrum [Figure 2a]. Trucut biopsy done from the lesion showed necrotic bony tissue, Langhan's type of multinucleated giant cells, and focal areas of caseous necrosis [Figure 2b]. ZN stain for AFB and PAS stain for fungus done on trucut biopsy were negative.
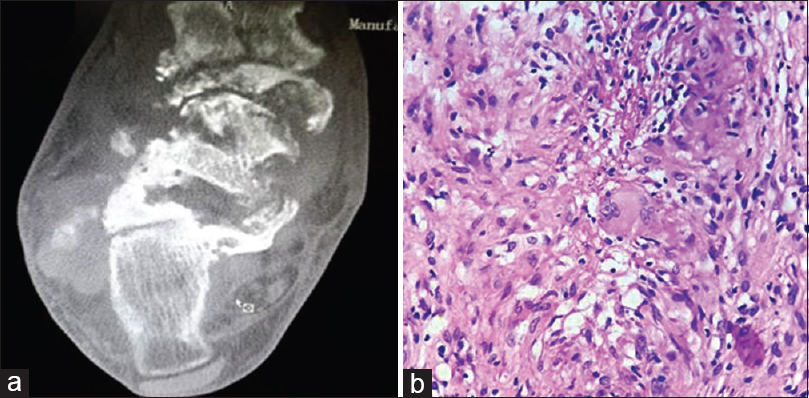
- (a) Computed tomography scan showed multiple irregular lytic foci involving the talar, navicular, part of calcaneum, and lateral cuneiform with surrounding edema with coke-like sequestrum. (b) Trucut biopsy showed epithelioid cell granulomas along with Langhan's giant cells (H and E, ×400)
The patient was advised the World Health Organization directly observed treatment, short-course Category I anti-tubercular therapy (ATT) for a minimum period of 9 months. At 5-month follow-up, she has been doing well and responded to ATT.
ADDITIONAL QUIZ QUESTIONS
Q2: Which of the following tarsal bone is most commonly involved by tuberculosis?
-
Navicular
-
Talus
-
Calcaneum
-
Cuneiforms.
Q3: Which of the radiological type of tuberculosis of foot has the best outcome?
-
Cystic or osteolytic
-
Spina ventosa
-
Rheumatoid
-
Subperiosteal.
ANSWERS TO ADDITIONAL QUESTIONS
Q2 (b); Q3 (a)
Q2 (b): Osteoarticular tuberculosis accounts for 2.2%–4.7% of all cases of tuberculosis in the Western countries and around 10%–15% of extrapulmonary tuberculosis cases.[8] The incidence of extrapulmonary tuberculosis rises to 15%–20% in Asian countries.[8] Tuberculosis of foot and ankle bones accounts for about 10% of osteoarticular tuberculosis.[9] Posttraumatic tuberculosis is even rarer.[10] Any of the bones of the foot can be affected either alone or in combination. Calcaneum is the most common tarsal bone involved by tuberculosis.[8] The other bones of foot and ankle involved are talus, first metatarsal, navicular, and medial and intermediate cuneiforms.[1] Midtarsal joint is the most common affected joint.[9]
Q3 (a): Radiological findings include periarticular osteoporosis, marginal erosion, and joint space narrowing (Phemister triad).[10] Peripheral marginal erosion of joint is the earliest change in plain radiography.[3] Coke-like sequestrum is often noted.[10] Magnetic resonance imaging (MRI) of the foot shows early joint effusions and soft tissue swelling.[10] However, CT is superior to MRI in detecting cortical bone destruction.[10] Radiologically, tuberculosis of foot is of five typical types: cystic, rheumatoid, subperiosteal, kissing, and spina ventosa.[4] Cystic or osteolytic type shows intraosseous radiolucent area with loss of trabeculae.[511] The surrounding soft tissue may or may not be involved and sequestrum may or may not be found.[411] Rheumatoid type shows loss of articular cartilage and osteoporosis of the involved bones, giving the appearance of a coalesced mass of bone, similar to the appearance of the carpus in rheumatoid arthritis (carpal coalition).[4] Subperiosteal type shows subperiosteal scalloping of bones. In kissing type, the infection is localized to one joint with symmetrical scalloping of the adjacent articular surfaces of the involved bones.[4] Spina ventosa refers to the involvement of small bones of the hands and feet characterized by fusiform expansion of the bone, underlying bone destruction, and overlying periosteal new bone formation.[1] Of all these types, cystic type has the better outcome while rheumatoid has the poorest outcome.[4] The present case was radiologically labeled as cystic or osteolytic type. If radiological presentations are atypical, the diagnostic dilemma worsens, especially in a low incidence site like the foot.[4] The radiological features of tuberculosis of ankle and foot may be similar to that of rheumatoid arthritis, sarcoidosis, neuropathic joints, and neoplasms.[3]
BRIEF REVIEW OF THE TOPIC
Clinical findings
Chest radiography shows pulmonary disease in one-third to one-half of cases, but active pulmonary tuberculosis is infrequent.[8] Clinically, these patients have insidious onset and present with pain, swelling, and stiffness.[3] Discharging sinus and nonhealing ulcer with secondary infections are other manifestations.[3] Muscle atrophy due to disuse is characteristically present.[4] Disuse atrophy also leads to periarticular osteoporosis.[4] Clinically, tuberculosis of ankle and foot has varied differential diagnosis such as pyogenic osteomyelitis, inflammatory arthritis, osteochondrosis, and malignancy arising from bone and soft tissue.[3]
Chest radiography shows pulmonary disease in one-third to one-half of cases, but active pulmonary tuberculosis is infrequent.[8] About one-third of patients give a history of trauma.[4] However, the relation between trauma and tuberculosis is still not clear.[4] It has been postulated that trauma produces a locus, which is susceptible to hematogenous infection.[12] Another theory states that traumatic injury activates a preexisting small and symptom-free latent focus, which would not otherwise have developed into a real tuberculous lesion.[12] Pain is the earliest symptom of posttraumatic osteoarticular tuberculosis.[8] Pain usually precedes signs of inflammation for weeks or months.[8] However, the local signs of inflammation are often mild and constitutional symptoms are usually absent.[10] As a result, the duration between trauma and diagnosis of osteoarticular tuberculosis gets prolonged leading to therapeutic delay.[3] In the present case, history of trauma was present followed by pain in the ankle joint.
Diagnostic role of fine-needle aspiration biopsy
-
Fine-needle aspiration biopsy (FNAB) is a simple and safe outdoor procedure for the diagnosis of osteoarticular tuberculosis[12]
-
FNAB can easily be done in pathologically altered bone and useful diagnostic material can be obtained for cytomorphological examination[1]
-
Considering the fact that tuberculosis of ankle and foot has varied differential diagnosis clinically and radiologically and difficult to demonstrate or culture acid-fast mycobacteria, FNAB becomes important in such a setting for a definitive diagnosis.[12]
Potential pitfalls in cytological diagnosis of osteoarticular tuberculosis
-
Presence of granulomas without necrosis
-
Presence of only necrosis
-
Difficult to demonstrate AFB in ZN stain due to paucity of AFB
-
Cytomorphological mimickers of the lesions.
Handa et al. noted epithelioid cell granulomas with or without necrosis in 85.2% of cases.[1] Masood noted granulomas with or without necrosis in 73% of cases.[2] Scattered multinucleated and Langhans’ giant cells were present in 55.6% of cases.[1] Background usually had inflammatory cells, osteoblasts, and proliferating fibroblasts.[1] Osteoarticular tuberculosis is a paucibacillary disease.[34] Hence, it is difficult to demonstrate AFB and culture is rarely positive in these lesions.[34] Handa et al. observed 22.2% positivity for AFB in cytology smears.[1]
Focused differential diagnosis of osteoarticular tuberculosis:
Sarcoidosis
Eosinophilic granuloma
Fungal infections
Role of real-time polymerase chain reaction in osteoarticular tuberculosis
Advanced molecular methods such as real-time polymerase chain reaction (RT-PCR) have shown very promising results for the early and rapid diagnosis of tuberculosis, due to its detection capability in various clinical samples with bacilli load as less as 1–10 bacilli.[13] It has increased the diagnostic predictability in osteoarticular tuberculosis with paucibacillary samples. The specificity of PCR is as high as 93.75% and the sensitivity ranges from 61% to 83% in various studies.[13] However, if RT-PCR is negative, further decisions would be based on the histopathological findings. Irrespective of RT-PCR status, a positive biopsy warrants antitubercular treatment.[13]
SUMMARY
Tuberculosis of talar bones is an uncommon form of osteoarticular tuberculosis. Diagnostic and therapeutic delay may occur due to uncommon site, lack of awareness, and ability to mimic other diseases clinically and radiologically. Thus, a prompt diagnosis and management is necessary to reduce any functional morbidity. The role of FNAB thus becomes important in such a setting for an early definitive diagnosis.
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The author(s) declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author.
Each author has participated sufficiently in the work and take public responsibility for appropriate portions of the content of this article.
BD carried out the procedure, interpreted the results, and drafted the manuscript.
AHD interpreted the results and helped draft the manuscript.
P helped to carry out the procedure, collected the details of the case, and helped draft the manuscript.
CBG participated in the interpretation of the results and participated in its design and coordination.
JSN participated in its design and coordination.
AR involved with the management and helped draft the manuscript.
All authors read and approved the final manuscript.
Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from the Institutional Review Board (or its equivalent).
LIST OF ABBREVIATIONS (In alphabetic order)
AFB- Acid fast bacilli
ATT - Anti-tubercular therapy
CT - Computed tomography
FNAB - Fine-needle aspiration biopsy
MRI - Magnetic resonance imaging
PAS - Periodic-acid Schiff
RT-PCR - Real-time-polymerase chain reaction
ZN - Ziehl-Neelson.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model. (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Role of fine-needle aspiration cytology in tuberculosis of bone. Diagn Cytopathol. 2010;38:1-4.
- [Google Scholar]
- Diagnosis of tuberculosis of bone and soft tissue by fine-needle aspiration biopsy. Diagn Cytopathol. 1992;8:451-5.
- [Google Scholar]
- Ankle and foot tuberculosis: A diagnostic dilemma. J Family Med Prim Care. 2014;3:129-31.
- [Google Scholar]
- Cytological diagnosis of sarcoidosis revisited: A state of the art review. Diagn Cytopathol. 2011;39:541-8.
- [Google Scholar]
- Cytopathologic diagnosis of an eosinophilic granuloma of bone by needle aspiration biopsy. Acta Cytol. 1989;33:683-5.
- [Google Scholar]
- Fine-needle aspiration biopsy in fungal infections. Diagn Cytopathol. 1997;16:31-4.
- [Google Scholar]
- Posttraumatic tuberculous osteomyelitis of the foot – A rare case report. Chin J Traumatol. 2015;18:184-6.
- [Google Scholar]
- The role of polymerase chain reaction in the management of osteoarticular tuberculosis. Int Orthop. 2009;33:801-5.
- [Google Scholar]







