Translate this page into:
A rare case of malignant metastatic tumor diagnosed on fine-needle aspiration of cervical lymph node
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
A 57-year-old female came to ear, nose, throat outpatient department with painless right-side cervical swelling for 1½ years. On examination, she had an enlarged right cervical lymph node in the middle part of the neck, measuring approximately 3 cm in diameter. It was firm, mobile, and nontender. Fine-needle aspiration cytology (FNAC) was performed from the cervical lymph node to establish the diagnosis [Figure 1].
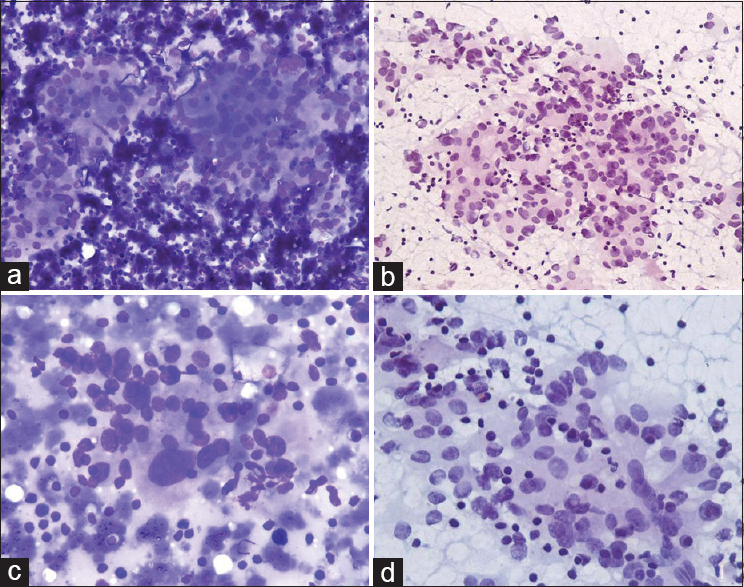
- Fine-needle aspiration cytology. (a and b) Cellular smears showing loose cohesive clusters of tumor cells with acinar follicular pattern in a background of reactive lymphoid cells (a: MGG, ×100; b: PAP, ×100). (c) High power showing round-to-oval nucleus with moderate anisonucleosis and bizarre cell (MGG, ×400). (d) Tumor cell showing fine nuclear chromatin and moderate-to-abundant fragile cytoplasm and lymphocyte sprinkling (PAP, ×400)
QUESTION
What is your Interpretation?
-
Reactive lymphoid proliferation
-
Non-caseating granuloma
-
Metastatic paraganglioma
-
Metastatic follicular carcinoma.
ANSWER
The correct cytopathology interpretation is: C. Metastatic paraganglioma
On microscopic examination, the smears were cellular and showed many loose cohesive clusters and dispersed tumor cells in a background of abundant reactive lymphoid cells and hemorrhage [Figure 1a and b]. The tumor cells were arranged in focal acinar or follicular pattern with a round-to-oval nucleus, moderate anisonucleosis, fine nuclear chromatin, and moderate-to-abundant fragile cytoplasm with the focal presence of fine granules. Few bizarre and binucleated tumor cells were also noted [Figure 1c and d]. On the basis of characteristic cytological features, a diagnosis of metastatic neuroendocrine tumor/paraganglioma was suggested.
In view of the cytological diagnosis, the patient was further evaluated by ultrasonography and contrast-enhanced computerized tomography (CECT) of the neck. CECT revealed, in addition, a lobulated, ill-marginated enhancing space-occupying mass in the right carotid bifurcation. It was in close proximity to right common carotid artery beginning at the level of carotid bifurcation. It measured approximately 3.4 cm × 3.2 cm × 3.2 cm [Figure 2]. On color Doppler evaluation, the lesion was observed to lie between the internal and external carotid arteries. She underwent surgery, and resection of the tumor with neck dissection was performed, which was reported as malignant carotid body paraganglioma on histopathology.
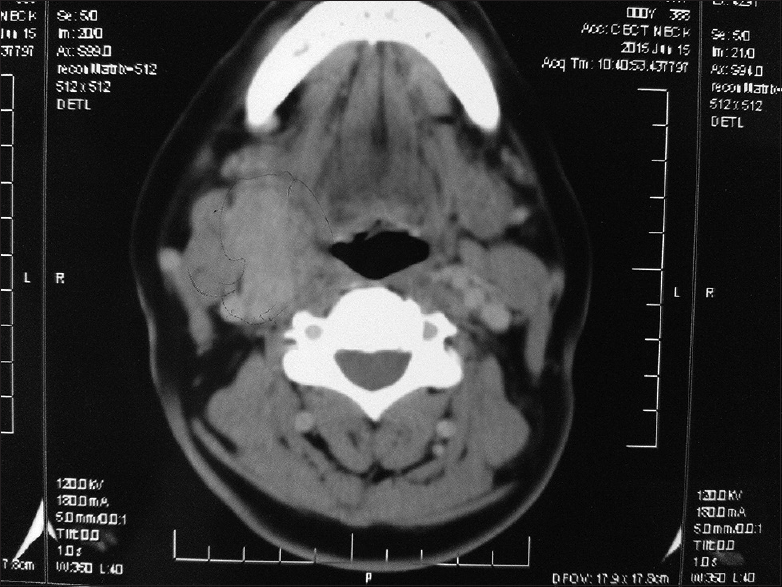
- Contrast-enhanced computerized tomography showing a lobulated, ill-marginated enhancing space occupying lesion in the right carotid bifurcation
ADDITIONAL QUIZ QUESTIONS
Q1: Which is the most common site of paraganglioma?
-
Carotid body
-
Adrenal gland
-
Mediastinum
-
Organ of Zuckerkandl.
Q2: Following immunohistochemistry (IHC), which IHC marker is not expressed in paraganglioma?
-
S-100
-
Pan-cytokeratin
-
Synaptophysin
-
Neuron-specific enolase.
Q3: Which of the following is the diagnostic feature of malignant paraganglioma?
-
Pleomorphism
-
Mitosis
-
Metastases
-
All the above.
ANSWERS TO THE ADDITIONAL QUESTIONS
Q1: b; Q2: b; and Q3: c
Q1: (b) Adrenal gland accounts for 90% of paraganglioma, which is also known as pheochromocytoma at this site. Extraadrenal paraganglioma accounts for the rest 10%–15% cases. The most common extraadrenal site is the carotid body and the organ of Zuckerkandl[1]
Q2: (b) The chief cells of paraganglioma show positive immunostaining with chromogranin, synaptophysin, and neuron-specific enolase, whereas S-100 and glial fibrillary acidic proteins are positive in stellate or dendritic sustentacular cells.[1] Pan-cytokeratin is negative in both the cells
Q3: (c) Malignant paraganglioma is diagnosed only when it metastasizes to the regional lymph node or distant organs such as the liver, bone, or lungs.[1] There are no accepted cytological or histopathological criteria for the diagnosis of malignancy in paraganglioma. Multicentric paraganglioma must be distinguished from the true metastases.
BRIEF REVIEW OF THE TOPIC
Paraganglia are collections of specialized neural crest cells arising in association with the autonomic ganglia. Tumors arising from these cells are called paragangliomas, and their names depend on their site.[23] Carotid body paraganglioma is the most common extraadrenal paraganglioma in the head-and-neck region.[23] It is situated in the adventitia of the posteromedial aspect of the common carotid artery bifurcation. The usual clinical presentation is that of a painless, slowly enlarging cervical mass, and the median age of presentation is 45–54 years, with female predominance 2:1.[456]
The incidence of malignant form is 6% to 24% of nonadrenal paraganglia.[7] The risk of malignancy is more in young patients with heritable tumors. The distinction between benign and malignant form cannot be made on cytomorphology or histopathology. Malignant carotid body paraganglioma usually metastasizes to the regional lymph nodes, liver, bone, or lungs.[7] Our case presented with painless, progressive cervical lymphadenopathy, which on FNAC turned out to be an unsuspected case of malignant carotid body paraganglioma contrary to usual presentation of tumor itself presenting as a cervical mass.
The cytomorphological features are well established,[389] with smears showing cells arranged in loose cohesive clusters and singly with acinar/follicles/rosette formations. Tumor cells are round-to-oval, plasmacytoid, or spindle-shaped cells with moderate anisonucleosis. Fine and dusty chromatin with salt and pepper pattern is characteristic. Cells have abundant cytoplasm and indistinct cytoplasmic borders and may show red granules or vacuolization.
In the neck region, carotid body paraganglioma can be difficult to differentiate from thyroid neoplasms, neurogenic tumors, and metastatic carcinoma.[10] Acinar structures in paraganglioma can be mistaken for the follicles seen in follicular neoplasm of the thyroid. However, the identification of colloid is useful in such a setting. A misdiagnosis of the neurogenic tumor can occur if there is a predominance of ovoid- or spindle-shaped nuclei in a paraganglioma. The uniform and fine chromatin pattern of the nucleus in paraganglioma helps in distinguishing it from metastatic carcinoma.
Ancillary techniques are helpful for the confirmation of carotid body paraganglioma. It shows immunoreactivity for chromogranin, synaptophysin, neuron-specific enolase, and S-100.[11] Radioimaging studies, such as CECT and magnetic resonance angiography, and vascular imaging studies, such as Doppler ultrasound and selective digital subtraction angiography, are useful adjuncts to cytomorphology. These studies help in the exact localization of carotid body paraganglioma and also define their relation with major blood vessels.[1213] The diagnosis of malignant carotid body paraganglioma on FNAC of lymph node has been rarely reported. This case broadens the differential diagnosis of cervical lymphadenopathy. Authors also want to emphasize that aspiration cytology can be cost-effective and valuable tool to diagnose this rare tumor in unsuspected cases, which can be confirmed by radiological studies. It, thereby, helps the surgeon with the definite preoperative diagnosis so that the appropriate management can be planned for the patients with minimum complications.
COMPETING INTERESTS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
Each author has participated sufficiently in the work and takes public responsibility for the appropriate portions of the content of this article. SK carried out substantial contributions to conception and design, acquisition of data, and drafting the article. AA carried out substantial contributions to conception and design, acquisition of data, drafting the article, and revising it critically for important intellectual content.
ETHICS STATEMENT BY ALL AUTHORS
As this is case report without identifiers, our institution does not require approval from the Institutional Review Board (or its equivalent).
LIST OF ABBREVIATIONS (In alphabetic order)
CECT - Contrast-enhanced computerized tomography
FNA - Fine-needle aspiration
MGG - May–Grunwald–Giemsa
MRA - Magnetic resonance angiography
PAP - Papanicolaou
USG - Ultrasonography.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- World Health Organization Classification of Tumors. In: Barnes L, Eveson JW, Reichart P, Sidransky D, eds. Pathology and Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005. p. :362-3.
- [Google Scholar]
- Paragangliomas of the head and neck region: A clinical study of 69 patients. Cancer. 1977;39:397-409.
- [Google Scholar]
- Imaging and management of head and neck paragangliomas. Eur Radiol. 2005;15:1310-8.
- [Google Scholar]
- Fine needle aspiration biopsy cytology of paragangliomas. Cytologic, light microscopic and ultrastructural studies of three cases. Acta Cytol. 1983;27:651-7.
- [Google Scholar]
- National cancer data base report on malignant paragangliomas of the head and neck. Cancer. 2002;94:730-7.
- [Google Scholar]
- Fine-needle aspiration of six carotid body paragangliomas. Diagn Cytopathol. 1993;9:510-5.
- [Google Scholar]
- Parapharyngeal paraganglioma: Diagnosis on fine-needle aspiration. Am J Otolaryngol. 2005;26:360-1.
- [Google Scholar]
- Fine-needle aspiration diagnosis of carotid body tumor: Report of a case and review of experience with cytologic features in four cases. Diagn Cytopathol. 1997;17:143-7.
- [Google Scholar]
- Pitfalls in fine needle aspiration cytology of extraadrenal paraganglioma. A report of 2 cases. Acta Cytol. 2003;47:1082-6.
- [Google Scholar]







