Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
92: Role of cytology in classifying lung adenocarcinoma and its various subtypes: A five-year retrospective review with emphasis on cytomorphology
Israh Akhtar, MD, Anwer Siddiqi, MD, Rhyne Flowers, MD, Ric Bowlin, SCT, Mithra Baliga, MD
Department of Cytopathology, University of Mississippi Medical Center, Jackson, Mississippi
Introduction: Cytological techniques are of utmost importance in the diagnoses of lung cancer, which is the leading cause of cancer deaths in the United States for both men and women. Adenocarcinoma, arising from the bronchial mucosal glands, is the most frequent non-small cell cancer, representing 35 – 40% of all primary lung cancers. The pulmonologists, radiologists, and internists in conjunction with the cytopathologists are the key players in establishing the diagnoses and subtyping these lesions.
Materials and Methods: A retrospective study was conducted, wherein we reviewed the cytology database for adenocarcinomas of lung for the last five years (September 2005 – August 2010). The specimens included bronchial washes, bronchial brushes, bronchoalveolar lavage, transbronchial fine needle aspiration biopsy (FNAB), endobronchial ultrasound-guided FNAB (EBUS), pleural fluid cytology, image-guided transthoracic FNAB, core biopsy, and core imprints.
Results: A total of 146 cases of adenocarcinomas were diagnosed by various cytological methods. The cases included both primary lung as well as metastatic adenocarcinomas, including 74 male and 72 female patients, with an age range of 32 to 87 years. Lung adenocarcinoma in this study was observed most commonly between the fifth and seventh decades, with an increased incidence in the sixth decade (36.9%). Conventional adenocarcinoma was the most commonly diagnosed subtype (n = 112, i.e., 76.7%). The remaining cases included three bronchoalveolar carcinomas (BAC), mucinous subtype (2.05%), two BAC non-mucinous subtypes (1.3%), three adenocarcinomas with papillary configuration and psammoma bodies (2.05%), one signet ring cell type adenocarcinoma (0.68%), and one mucinous adenocarcinoma (0.68%). Twenty-four cases (16.4%) were metastatic adenocarcinomas from various body sites; colon (n = 10), breast (n = 8), kidney (n = 5), and endometrium (n = 1). The diagnosis of metastatic tumors was confirmed by a clinical workup and immunohistochemistry. On the basis of cytomorphology the conventional subtype, was graded into well, moderate, and poorly differentiated, in most cases.
Conclusions: Primary pulmonary adenocarcinomas may display a wide variety of cytomorphological patterns, which can be difficult to recognize in a limited sample. Familiarity with these unusual patterns, in conjunction with ancillary studies, such as immunohistochemistry, is the frontier for diagnosing and prognosticating subtypes of lung adenocarcinomas. The cytological mode of diagnoses has not only proven to be cost-effective and rapid, but has reduced the morbidity resulting from open biopsies.
93: Variability in the diagnostic yield of endobronchial ultrasound-guided transbronchial fine needle aspiration biopsy
Dustin Woods, MD, Charles Beavers, MD, Sunati Sahoo, MD
Department of Pathology and Laboratory Medicine, University of Louisville Health Sciences Center, Louisville, Kentucky
Introduction: EBUS-FNA is a minimally invasive procedure that has been increasingly used by clinicians for the diagnosis and staging of lung carcinoma. Over the past four years, the frequency of EBUS-FNA has been increasing at our institution. The purpose of this study was to examine the utility and diagnostic yield of this procedure.
Materials and Methods: A computer database search was performed at the University of Louisville Hospital for malignancy on EBUS-FNA cases, between January 2006 and October 2010. A total of 124 cases were retrieved and reviewed for FNA sites and diagnosis.
Results: FNA material from 156 sites was obtained on 124 patients using EBUS-FNA, at the University of Louisville, from 2006 to 2010. The total number of FNA sites were as follows: Lung masses 63, subcarinal nodes 46, paratracheal nodes 27, and peribronchial nodes 20. Of 156 FNAs, 40 were interpreted as non-diagnostic (25.6%). The non-diagnostic rate for lung masses was 17.5% (11 / 63). The non-diagnostic rates for lymph node sites were as follows: Peribronchial 25.0% (5 / 20), subcarinal 32.6% (15 / 46), and paratracheal 33.3% (9 / 27). The number of EBUS-FNAs and the overall non-diagnostic rate from 2006 to 2010 were as follows: 2006, 3 / 10 cases (30%); 2007, 3 / 13 cases (23%); 2008, 13 / 39 cases (33.3%); 2009, 16 / 64 cases (25%); and 2010, 5 / 30 cases (16.7%).
Conclusions: The diagnostic yield of EBUS-FNA was improved significantly as the operator gained more experience. At our institution, the yield of diagnostic material from lung masses was higher than that of lymph nodes.
94: Rapid onsite evaluation of endobronchial ultrasound-guided fine needle aspiration: Correlation between adequacy assessment and final diagnosis in patients with bronchogenic carcinoma
Kathryn Dyhdalo, MD1, Dawn Underwood, MS, CT(ASCP)1, Julie Shorie, CT(ASCP)1, Christine Booth, MD1, Peter Mazzone, MD2, Jennifer Brainard, MD1
1Anatomic Pathology, Cleveland Clinic, Cleveland, Ohio; 2Pulmonary and Critical Care Medicine, Cleveland Clinic, Cleveland, Ohio
Introduction: Endobronchial Ultrasound-Guided Fine Needle Aspiration (EBUS FNA) is a non-invasive method for diagnosis and staging of lung carcinoma, which utilizes real-time optical and ultrasound images to guide the biopsy procedure. Rapid onsite evaluation (ROSE) of FNA samples has been shown to increase the diagnostic yield. There are relatively few reports in the literature that specifically address discordant results between on site adequacy assessments and the final diagnoses. We decided to study our EBUS samples and investigate cases with discrepancies between rapid and final diagnoses in patients with bronchogenic carcinoma.
Materials and Methods: We reviewed all EBUS FNAs over a two-year period (January 2009 to December 2010). In all cases, the slides used for ROSE were stained with diff quik stain (DQ). Pap stained smears, ThinPreps®, and / or cell blocks were reviewed before a final diagnosis was rendered. We compared onsite adequacy assessments with the final diagnoses. If the interpretation at the time of ROSE agreed with the final diagnosis, the aspirate was classified as concordant. If the initial interpretation differed significantly from the final diagnosis, based on a review of all available material, then the case was classified as discordant. All available slides from discordant aspirates were reviewed and re-screened. The reason for the discordant result was categorized as either sampling or an interpretive / screening error at the time of ROSE. In discordant cases due to sampling, the location of the diagnostic material was noted.
Results: There were 340 EBUS procedures performed in 335 patients (168 men, 167 women, median age 65 years) with 575 sites sampled during the study period. A diagnostic discrepancy between ROSE and final diagnosis occurred in 138 (24%) total aspirates, including 65 (11%) aspirates from 53 patients with bronchogenic carcinoma. The remaining aspirates were concordant, including all cases called positive for carcinoma at the time of ROSE. The distribution of diagnoses in discrepant cases is summarized in Table 1. Of the 65 discrepant cases, 52 (80%) were positive for carcinoma on final review. All slides were available for re-screening in 60 discordant aspirates, including 47 with a final positive diagnosis. Re-screening of DQ stained slides in cases with a final positive diagnosis showed either no tumor cells or insufficient tumor cells for diagnosis in 28 (60%) cases. The location of the diagnostic cells in these discrepant cases due to sampling is summarized in Table 2. The remaining 19 (40%) cases were classified as interpretive or screening errors at the time of ROSE. The majority of these errors occurred in aspirates called atypical or atypical suspicious, which upon re-screening were considered diagnostic of carcinoma (16 aspirates, 84%).
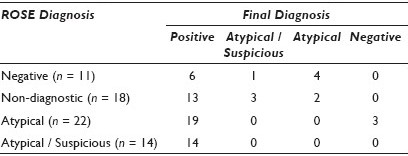
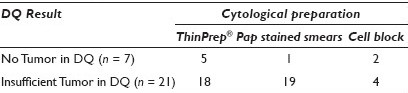
Conclusions: In our study, EBUS adequacy assessments and final diagnoses were concordant in 89% of the aspirates from patients with bronchogenic carcinoma. All aspirates with a positive interpretation at ROSE were concordant. in the discordant cases, all aspirates with ‘atypical cells suspicious for malignancy’ and 86% of aspirates with ‘atypical cells’ on ROSE had a final diagnosis of carcinoma. The majority of discordant cases with a positive final diagnosis were due to sampling (60%). In cases lacking tumor on DQ slides, the tumor was most commonly identified in the ThinPrep®. In cases with insufficient tumor cells for diagnosis on DQ, both the ThinPrep® slide and Pap stained smears were helpful diagnostically.
95: Multinucleated histiocytes in Fine Needle Aspirations of pulmonary hamartomas: A new morphological finding
Cherie Paquette, MD1, Gladwyn Leiman, MD1, Pam Michelow, MD2, Sara Brownschidle, MD1
1Cytopathology, Fletcher Allen Health Care and University of Vermont, Burlington, Vermont; 2Cytopathology, NHLS, University of the Witwatersrand, Johannesburg, South Africa
Introduction: Pulmonary hamartomas (PH) are among the most frequently encountered benign neoplasms of the lung. Commonly presenting as solitary lung nodules, peripheral hamartomas outnumber endobronchial variants by 9 : 1. The radiological diagnosis is specific in most cases; no further diagnostic intervention may occur, the PH being left in-situ under surveillance or resected, as dictated clinically. In cases with inconclusive radiology, fine needle aspiration (FNA) may be undertaken. The cytodiagnostic features of PH are well-described, resting primarily on recognition of the mesenchymal elements (cartilage and fibromyxoid matrix) admixed with benign bronchial cells and pneumocytes. In a recent case with otherwise characteristic features of a PH, numerous giant multinucleated histiocytes (MNHs) were observed. The literature review yielded no mention of this finding. This prompted a retrospective review of cases previously diagnosed as PH, specifically to determine whether the cytological presentation of PH may include MNHs.
Materials and Methods: Archived FNA slides diagnosed as PH by the above-described criteria were retrieved from the files of two institutions and rescreened to confirm the original cytodiagnoses, to ensure that no other pathology (particularly granulomatous) was missed, and they were specifically assessed for MNHs. Inclusion criteria required that MNHs be at least 3× the size of pneumocytes, display 3+ separately identifiable nuclei, and contain no carbon particles. We documented the number of MNHs per slide with the highest count: Findings were grouped as 1 – 4 (rare), 5 – 9 (moderate numbers) or greater than 10 (numerous) MNHs. The MNHs were further subclassified by size: 20 – 60 (regular) or greater than 60 microns (giant). The selected cases were subjected to immunochemical stains to confirm the histiocytic phenotype.
Results: Aspirates of 31 FNA-diagnosed PH from two institutions were retrieved. All cases were confirmed as hamartomas on review; there was no instance in which other pathology, particularly granulomatous, had been overlooked. Of the total of 31 cases, 30 (65%) were found to contain MNHs. MNHs were few in eight cases, moderate in a further eight cases, and numerous in the remaining four cases (quantified as defined earlier); the average number of MNHs per case was eight. The average MNH size was approximately 40 to 50 microns. However, in approximately 25% of the cases with MNHs, giant MNHs (greater than 60 microns) were a prominent and readily identifiable component on the slides reviewed [Figure 1]. Immunochemical stains confirmed that the cells were of the histiocytic type [Figure 2].
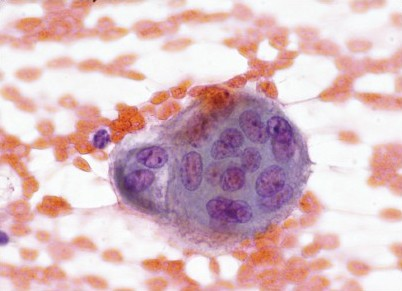
- MNH at 600× (Pap stain)
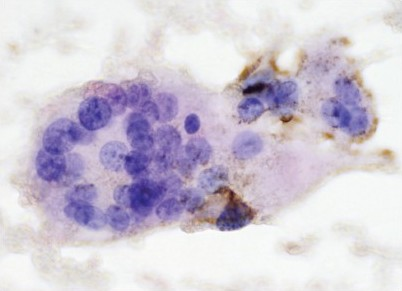
- MNH at 600× (CD68)
Conclusions: Reliable criteria for FNA diagnosis of PH have been well-described. To our knowledge, MNHs have not been mentioned as part of the spectrum of FNA morphology of these lesions. This study indeed shows that in the majority of cases, MNHs are either rare or of regular size, with insufficient prominence to be noted as conspicuous. Nevertheless, when specifically sought, MNHs were found in 65% of the 31 FNAs from PH. In approximately 25% of the positive cases, the MNHs may appear sufficiently large or numerous to impact the diagnosis. In cases with classic stromal representation, the diagnosis of PH would not be in doubt; however, in suboptimally aspirated nodules, the finding of giant MNHs might lead to confusion with granulomatous disease. This study identifies and confirms MNHs as within the range of features seen in FNAs from PH.
96: The performance of ThinPrep® respiratory cytology in the diagnosis of pulmonary small cell carcinoma
Cheng Wang, MD1, Qiuli Duan, MSc2, Margaret Kelly, MBChB, PhD, FCPath(SA), FRCPC1, Maire Duggan, MSc1
1Pathology and Laboratory Medicine, University of Calgary, Calgary, Alberta, Canada; 2Clinical Trials Unit, Tom Baker Cancer Center, Calgary, Alberta, Canada
Introduction: Calgary Laboratory Services (CLS) is the sole provider of respiratory cytology to nearly 1.3 M residents in the Calgary Health Region (CHR) and the cytology, since 1996, is prepared using the ThinPrep® method. This provided an opportunity to carry out the largest study on the sensitivity, specificity, and the positive (PPV) and negative (NPV) predictive values of ThinPrep® prepared bronchial wash and brush specimens in the diagnosis of pulmonary small cell carcinoma (SCCa).
Materials and Methods: All patients in the CHR with a diagnosis of SCCa between 2000 and 2004 were identified from the provincial cancer registry. The laboratory information system (LIS) was searched for all respiratory cytology performed in that interval. Bronchial wash and brush specimens of SCCa patients and those negative for lung cancer of any other type were identified. Cytology diagnoses of SCCa or suspicious for SCCa were considered test positive and all other cytology results were test negative. Unsatisfactory results were excluded. True positives (TP), true negatives (TN), false positives (FP), and false negatives (FN) were classified using the cancer registration as the gold standard.
Results: Of the 309 patients registered as SCCa, 199 (64.4%) had respiratory cytology. There were 129 brush and 170 wash specimens. There were 1,762 respiratory cytology (409 brush and 1,283 wash) specimens on 1,122 patients who were negative for lung cancer. Nearly 50% of the 538 brush and 1,453 wash specimens were diagnosed by five pathologists who did not have prior experience with ThinPrep® cytology. Among the 527 satisfactory brush (1, 440 wash) specimens, there were 78 (90) TP, two (14) FP, 48 (79) FN, and 399 (1,257) TN results [Table 1]. Differences in sensitivity and specificity between brush and wash specimens were not significant, but differences in PPV and NPV were (P = 0.009 and 0.0006, respectively). When the results were stratified by the year of diagnosis, the bronchial brush sensitivity increased from 51.0% in 2000 – 2001 to 68.8% in 2002 – 2004, and the difference was significant (P = 0.04)
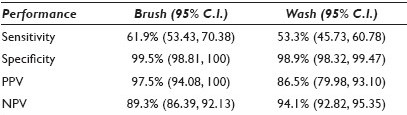
Conclusions: ThinPrep® prepared bronchial wash and brush cytology has moderate sensitivity, excellent specificity, PPV and NPV, in the diagnosis of SCCa. The bronchial brush is more sensitive than the wash, and has the potential to increase further with the pathologists’ experience.
97: Use of mutation-specific antibodies to detect epidermal growth factor receptor status in small biopsy and cytology specimens of lung adenocarcinoma
Adnan Hasanovic, MD, Andre Moreira, MD, PhD
Pathology, Memorial Sloan-Kettering Cancer Center, New York
Introduction: The epidermal growth factor receptor (EGFR) mutation status is the best predictor of response to tyrosine kinase inhibitors in adenocarcinoma of the lung. Approximately 70% of lung cancers are diagnosed in advanced stages, where small biopsies and cytological specimens are the only source of material for both diagnosis and mutation testing. In recent times, antibodies that can detect mutant EGFR protein have been introduced. We have evaluated the detection of the EGFR mutant protein by immunohistochemistry in small biopsy and cytology specimens of lung adenocarcinoma.
Materials and Methods: Forty-six cases of adenocarcinoma were analyzed (28 cytology cell blocks, 10 lung core biopsies, and 8 bone biopsies). Antibodies against the exon 19 deletion (15 bp deletion) and the L858R mutation were used under optimized conditions (Cell Signaling Technology). Stains were scored as negative (weak and focal staining in < 10% of tumor cells), 1+ (faint staining in > 10% of tumor cells), 2+ (moderate staining intensity), and 3+ (strong and diffuse staining). All the cases were analyzed by the standard molecular methods to detect EGFR mutations.
Results: Deletions in exon 19 were detected in 22% (4% cytology specimens, 30% core biopsies, and 67% bone biopsies) and L858R mutation in 11% (11% cytology specimens, 10% core biopsies, and 11% bone biopsies) of the cases. Using a cutoff of 2+ as positive, the positive predictive value (PPV) for exon 19 deletion and L858R mutation was 100%, as no false positive cases were detected. The negative predictive values (NPV) were 83 and 92%, respectively, which reflected the rate of false negative results. When a staining score of 1+ was considered positive, the PPV for exon 19 deletion and for L858R mutation was 76 and 86%, respectively. The drop in PPV was a result of the increased number of false positive cases.
Conclusions: Immunostains for specific mutant EGFR show a good correlation with mutation analysis and can be used as a screening method to identify patients for tyrosine kinase inhibition therapy. Cases with weak positivity (1+) should be considered equivocal due to the risk of false positive results. This methodology is potentially useful in areas where molecular analysis is not available and for use in small biopsies when the material is too scant for molecular analysis or in bone biopsies where the decalcification process interferes with the DNA quality.
98: Fine needle aspiration as a predictor of squamous cell carcinoma and adenocarcinoma subtypes of non-small cell lung carcinoma
Seema Lale, MD, Nora Morgenstern, MD, Daniel Soto, CT(ASCP), Chiara Sugrue, MS, SCT(ASCP), Patricia Wasserman, MD, FCAP
Pathology, North Shore Long Island Jewish Health System, Lake Success, New York
Introduction: Recent changes in therapeutic modalities, such as, targeted therapy with epidermal growth factor receptor (EGFR) inhibitors, have increased the need for a sub-classification of non-small cell carcinomas on both biopsy and cytology specimens. Recent literature has demonstrated the reliability of cytological diagnosis of lung cancer by fine needle aspiration (FNA). The majority of lung cancers are not resectable at the time of presentation. The diagnosis and treatment decisions are made with increasing use of transbronchial and endobronchial ultrasound-guided needle (EBUS) aspirations. The aim of this study is to measure the accuracy of cytology in distinguishing squamous cell carcinoma (SCC) and adenocarcinoma (ADC) of the lung when compared to tissue diagnosis, and to assess the contribution of immunocytochemistry to this differential.
Materials and Methods: We retrospectively reviewed 613 cases of lung FNA from 2005 to 2010. Of these, 123 patients had FNA diagnosis of ADC, SCC, and Non-small cell lung carcinoma not otherwise specified (NSCLC - NOS), with confirmatory tissue diagnosis. Small cell carcinomas, neuroendocrine tumors, and metastatic carcinomas were excluded from this study. The immunocytochemical stains for TTF-1, p63, and CK5 / 6 were performed on 62 cases. The cytology results were correlated with the histological diagnosis.
Results: Forty-six percent (57 / 123) of the surgical specimens were diagnosed as ADC, 39% (48 / 123) as SCC, and 15% (18 / 123) as NSCLC-NOS. A specific cytological diagnosis was rendered in 81% (100 / 123) of the cases. The cytology cases were accurately classified based only on cytomorphological features in 75% (43 / 57) of ADC, 83% (40 / 48) of SCC, and 100% of (18 / 18) NSCLC-NOS. In 17 cases the initial cytology was NSCLC, but immunocytochemistry permitted sub-classification into adenocarcinoma in (11 / 57) 19% and squamous carcinomas in (6 / 48) 12%. Based on cytomorphology alone, three SCCs by cytology had subsequent tissue diagnosis of ADC, confirmed by immunohistochemistry. Conversely, two ADCs by cytology had subsequent tissue diagnosis of SCC confirmed by immunohistochemistry.
Conclusions: The distinction between adenocarcinoma and squamous carcinoma was accurate based on cytomorphology alone in 75 and 83% of the cases, respectively. Immunocytochemistry was needed in 19 and 12% of the cases. Cytomorphology alone was inaccurate in (3 / 57) 5% of the ADC and in (2 / 48) 4% of the SCC. These findings highlight the importance of immunocytochemical confirmation on both cytology and histology in cases of poorly differentiated ADC and non-keratinizing SCC. This study also supports the cytology-based sub-classification of NSCLC with immunocytochemical aid for diagnosis and treatment decisions.
99: Subclassification of NSCLC / carcinoma on 240 FNA specimens: Can p63 and napsin A be used as a minimal immunohistochemical panel in addition to TTF?
Grzegorz Gurda, MD, PhD1, Lei Zhang, MD2, Syed Ali, MD1, Frederic Askin, MD1, Edward Gabrielson, MD1, Qing Li, MD, PhD1
1Pathology, The Johns Hopkins Medical Institutions, Baltimore, Maryland; 2Pathology, The University of Hawaii, Honolulu, Hawaii
Introduction: Over 60% of non-small cell lung cancer (NSCLC) patients present with a locally advanced or metastatic (stage III or IV) disease at the time of diagnosis. Current treatments for NSCLC have advanced to the point at which further sub-classification of NSCLC into squamous cell carcinoma (SQC) and non-SQC, such as adenocarcinoma (ADC) and others, is necessary. Fine needle aspiration (FNA) cytology plays a critical role in the diagnosis and staging of lung cancer patients; the distinction between SQC and ADC, however, may be difficult on FNA specimens, due to the scant material. Although several studies have investigated the utility of immunohistiochemical (IHC) markers in the sub-classification of NSCLC, most are based on surgical or biopsy material and often with a limited number of cases. The study of using a minimal panel of markers for classification of cytological samples is still suboptimal. Our previous study has shown that Napsin A and TTF form a useful panel for identifying lung ADC. In this study, we have retrospectively assessed the clinical utility of p63 in the sub-classification of NSCLC into SQC and ADC on FNA specimens, in addition to Napsin A and TTF.
Materials and Methods: A computer search of a major teaching hospital identified 240 FNA cytological cases of ‘NSCLC or carcinoma with IHC studies’ over a seven-year period (2004 – March 2011). The cases consisted of lung primaries (n = 74), metastases of a lung primary (n = 61), as well as other malignancies of non-lung primary (n = 105). Among 240 cases, 125 cases (52%) had a surgical follow-up.
Results: The p63 staining of 135 lung cancers is summarized in Table 1. In SQC, p63 was positive in 87% (40 / 46) and negative in 13% (6 / 46) of the cases, while, in non-SQC, p63 was positive in 21% (19 / 89) and negative in 79% (70 / 89) of the cases. Particularly, p63 was positive in 19% (8 / 43) and negative in 81% (35 / 43) of the lung ADC cases. The overall sensitivity and specificity of p63 were 87 and 78%, respectively. The addition of Napsin A in 2008 reduced the unclassified NSCLC from 20% (5 / 25 cases) to 9% (10 / 108 cases), with an increased diagnostic rate of ADC. The combination of p63 and Napsin A showed a better sensitivity and specificity of 94 and 88%, respectively. The staining pattern of p63 in 105 non-lung carcinomas is summarized in Table 2; and it reveals a sensitivity and specificity of 91% and 77%, respectively, for SQC, as urothelial carcinoma was not included. The correlation between the cytological FNA specimen and surgical pathology was 95%.
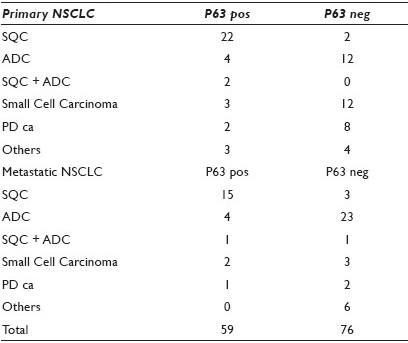
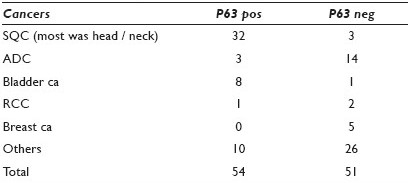
Conclusions: Our data demonstrated that p63 and Napsin A can be efficiently used in the sub-classification of NSCLC in addition to TTF. Both false positive and negative cases were identified in our study. The combination of p63 and Napsin A showed a better sensitivity and specificity than p63 alone. Therefore, from a practical standpoint, p63, Napsin A, and TTF may be used as a minimal panel of IHC markers.
100: Retrospective review of bronchial brushing specimens from peripheral lung nodules utilizing morphology and fluorescence in-situ hybridization characteristics
Trynda Oberg, MS, CT(ASCP), Jesse Voss, CT(ASCP), Justin Cassett, Mark Vande Haar, Jordan Reynolds, MD, Kevin Halling, MD, PhD, Amy Clayton, MD, Michael Henry, MD
Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota
Introduction: The sensitivity of routine cytology is suboptimal due to sampling difficulties of peripheral lung nodules, and fluorescence in-situ hybridization (FISH) assays have been shown to increase the detection of these lesions. Since 2006, our laboratory has offered a FISH reflex assay for the detection of lung cancer using residual bronchial brushing (BB) cytology specimens. The goal of this study is to determine the value of FISH for detecting peripheral lung neoplasms with equivocal BB cases and to evaluate the potential cytological criteria indicative of carcinoma in these specimens.
Materials and Methods: The medical records were searched for equivocal (atypical or suspicious) BB specimens from peripheral lung nodules that had reflex FISH testing and clinical follow-up information. FISH was called positive when ≥ 5 hypertetrasomy (polysomy) cells (≥ 3 signals for ≥ 2 probes, with at least one of the probes showing five signals) were present. The gold-standard was determined by using the pathological and / or radiological evidence of a lung neoplasm. The BB slides were re-screened by the cytotechology students and a cytopathology Fellow without knowledge of the clinical outcome, and each case was evaluated for numerous cytological criteria in the most abnormal appearing cells on the slides. Positive (n = 5) and negative (n = 5) control cases were reviewed, but not included for data analysis.
Results: From June 2006 through January 2011, 37 BB samples from 36 patients met the study criteria for inclusion. Patient demographics included 17 females and 19 males with a mean age of 71.6 years (range 49 – 87 years). Lung malignancy was found in 10 of 21 (48%) atypical cytology specimens and 14 of 16 (88%) suspicious cytology specimens. Cancer subtypes included: Adenocarcinoma (n = 8), typical carcinoid (n = 1), non-small cell carcinoma (n = 3), squamous cell carcinoma (SCC) (n = 8), and small cell carcinoma (SCLC) (n = 4). Polysomy FISH results were present in 13 specimens (n = 7 atypical, n = 6 suspicious) and all were found to have cancer on follow-up. Conversely, 46% (11 / 24) of the specimens diagnosed as negative by FISH were found to have lung cancer. Hyperchromasia in the majority of abnormal cells was identified in significantly more patients with cancer (63 vs. 15%; p = 0.006). Absent nucleoli were found significantly more often in patients with cancer (25 vs. 0%; p = 0.049) and we observed that these six cases were SCC (n = 5) and SCLC (n = 1). Hypochromasia was identified in the majority of abnormal cells in patients without cancer (77 vs. 33%; p = 0.011). Notably, all five cases (100%) with gland-like architecture and 11 / 14 (79%) with architecture of single abnormal cells, had cancer. Interestingly, 12 / 18 cases (67%) with abnormal single cells containing cilia / terminal bars present were found to have cancer on follow-up. All four cases (100%) with cells present, with nuclei four to five times the normal size, had cancer.
Conclusions: In our small pilot study, in the BB specimens diagnosed as equivocal, we did not find clear-cut cytological criteria indicative of cancer; however several appeared to be helpful. The numerous types of cancers might partially explain why the distinct cytological features were lacking. All patients with a polysomy FISH result had a lung neoplasm; FISH might be a useful tool in determining which patients with a peripheral lung nodule and an equivocal cytology result were most likely to have cancer on follow-up.
101: Utility of cell block preparations in endobronchial ultrasound-guided transbronchial-needle aspirates
Arbaz Samad, MD1, Charanjeet Singh, MD1, David Tasso, MD1, Tetyana Mettler, MD1, Rafael Andrade, MD2, Stefan Pambuccian, MD1
1Laboratory Medicine and Pathology, University of Minnesota, Minneapolis, Minnesota; 2Surgery, University of Minnesota, Minneapolis, Minnesota
Introduction: Endobronchial ultrasound-guided transbronchial-needle aspirates (EBUS-TBNA) is a novel, minimally invasive technique used for staging of patients with lung cancer and the diagnosis of accessible mediastinal lymphadenopathies or masses. The aim of this study was to determine the diagnostic utility of Cell block preparations (CBP) in addition to smears in the EBUS-TBNA samples.
Materials and Methods: We recorded specimen adequacy, cytological diagnoses, adequacy of CBP, and the use of immunoperoxidase stains (IPS) and special stains (SS), FISH, and molecular studies on CBP, in the EBUS-TBNA performed between January, 2008 and April, 2011. EBUS-TBNA specimens were procured by thoracic surgeons in the operating room. Preparation of slides, triage of the specimens, and rapid onsite evaluation (ROSE) was performed by a cytopathologist. After air-dried and alcohol-fixed smears were made, the residual specimen was placed in 10% buffered formalin for CBP. When ROSE was suspicious for lymphoma or infection, part of the residual material was submitted for flow cytometry or culture. IPS or SS were ordered immediately based on the ROSE impression; additional stains were ordered as needed. Cell blocks were prepared by the HistoGel method and sections were stained with H and E.
Results: During the study period, 244 patients (M = 131 / F = 113) aged 15 to 89 (mean 61) years, underwent EBUS-TBNA. One to five (mean 2) nodal and / or pulmonary sites were sampled for a total of 480 individual specimens. In 88 specimens (18.3%) the EBUS-TBNA result was ‘inadequate’ based on the lack of sufficient lymphoid cells in the absence of granulomas or neoplastic cells. Of the remaining 392 specimens that were considered to be diagnostic, 40 (10.2%) had inadequate CBP cellularity. In these cases, the diagnosis was based on smears alone, and it was ‘malignant’ in 17 cases and ‘negative for malignancy’ in 23 (granulomas, n = 14 and reactive lymph node, n = 9). The remaining 352 specimens had adequate CBP. Table 1 shows the differences in diagnosis between the two groups in the ‘non-negative’ cases. Of the 73 cases of nonsmall-cell lung carcinomas (NSCLC) (adenocarcinomas (ADCA), n = 44, squamous cell carcinoma (SqCC), n = 25, and NSCLC, NOS, n = 4), 48 (66%) were diagnosed based on their characteristic morphology on smears and CBP and comparison with the previous histology (when available), while in the remaining 25 cases (34%), a panel of IPS (CK5 / 6, CK7, TTF1, and p63) was used, resulting in a diagnosis of ADCA in 19 and SqCC in two. Four cases could not be classified as ADCA or SqCC and were diagnosed as NSCLC, NOS. Of the cases with adequate CBP, 30 patients had granulomas: AFB / GMS stains were successfully performed in all cases and were negative in all but three cases, which showed fungal organisms consistent with Histoplasma. Molecular studies for EGFR, and in some cases also for KRAS and EML4-ALK were performed in 22 adenocarcinomas; 20 were successful and showed EGFR mutations in two. In one case of metastatic Ewing sarcoma, FISH was positive for the EWSR1 translocation.
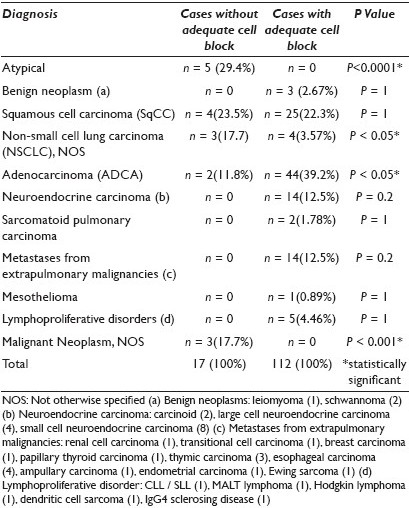
Conclusions: Whenever possible, CBP should be made from EBUS-TBNA material to perform IPS, SS, and molecular studies because they allow:
-
More frequent, specific, and definitive diagnoses (no ‘atypical’ diagnoses)
-
Subtyping of NSCLC and their nodal metastases to allow accurate therapeutic decisions
-
Exclusion of infectious agents in the majority of cases with granulomas
-
Performance of molecular studies for EGFR, KRAS, and EML4-ALK in cases of adenocarcinoma, allowing personalized treatment options
102: Evaluation of the effectiveness of CT-FNA cytology in stage I lung cancer
Melissa Paoni, CT(ASCP)1, Mary-Beth Beasley, MD1, David Burstein, MD1, Matthew Cham, MD2, David Yankelevitz, MD2, Maoxin Wu, MD, PhD1
1Anatomic Pathology, The Mount Sinai School of Medicine, New York, New York; 2Radiology Associates, The Mount Sinai School of Medicine, New York, New York
Introduction: Lung carcinoma accounts for the most cancer-caused deaths in both men and women. CT-guided fine needle aspiration (CT-FNA) biopsy cytology of small lung lesions has become crucial in the early diagnosis and management of lung carcinomas. The objective of this study is to evaluate the effectiveness of CT-FNA cytology in diagnosing stage I lung cancer (< 3 cm).
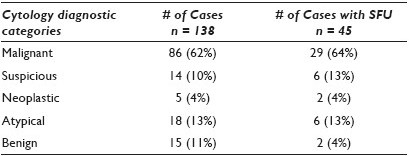
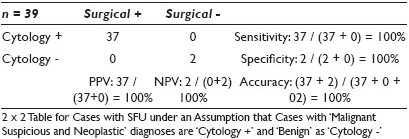
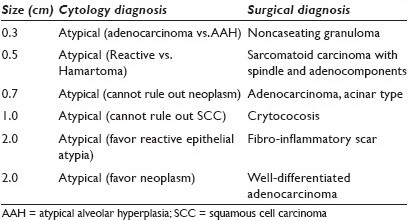
Materials and Methods: In the period from 16 February 2010 to 29 March, 2011, 312 CT-FNA lung biopsies were performed at the Mount Sinai School of Medicine. There was 138 cases with recorded tumor sizes of 3.0 cm or less, based on CT. These cases were cytologically classified as ‘Malignant, Suspicious for Malignancy, Neoplastic, Atypical, and Benign.’ Statistical analysis was performed for the cases with surgical follow-up (SFU) using surgical diagnosis as the gold standard.
Results: Among the 138 cases [Table 1], there were 86 (62%) malignant, 14 (10%) suspicious, 5 (4%) neoplastic, 18 (13%) atypical, and 15 (11%) benign. There were 45 cases that had surgical correlations including 29 (64%) malignant, six (13%) suspicious, two (4%) neoplastic, six (13%) atypical, and two (4%) benign cases. As shown in Table 2, all 39 cases within malignant, suspicious, neoplastic, and benign groups show virtual agreement with the surgical diagnoses and thus achieve 100% sensitivity, 100% specificity, 100% positive predictive value (PPV), 100% negative predictive value (NPV), and 100% accuracy. The rest of the six atypical cases [Table 3] showed three (50%) carcinomas and three (50%) non-neoplastic lesions.
Conclusions: The results suggest that CT-FNA cytology is a sensitive and specific diagnostic modality for stage I lung cancer with great positive and negative predictive values and great accuracy in the majority of cases except a small percentage of atypical cases.
103: The accurate subtyping of lung carcinoma on cytology specimens: A cytomorphological and immunohistochemical comparison
Scott Lauer, MD, Momin Siddiqui, MD, Cynthia Cohen, MD, Michelle Reid, MBBS
Pathology, Emory University School of Medicine, Atlanta, Georgia
Introduction: Accurate subtyping of non-small cell lung carcinoma into adenocarcinoma (AD) and squamous cell carcinoma (SQC) has become critical because of the emerging histology-specific therapies. However, while drugs such as Bevacizumab (Avastin) are effective in the treatment of lung AD, the same drug may cause life-threatening pulmonary hemorrhage in patients with SQC of the lung. Therefore, accurate cytological distinction between SQC and AD is paramount. However, it can be especially difficult for cytopathologists to make this distinction in limited cytology specimens, particularly when the tumors are poorly differentiated. Several immunohistochemical (IHC) stains aid in the distinction of these two subtypes, but with variable results. We compared the accuracy of cytomorphological and IHC diagnosis of lung AD and SQC on fine needle aspiration (FNA) to the gold standard histological (biopsy or resection) specimen.
Materials and Methods: A total of 43 resected or biopsied lung AD (24), SQC (13), sarcomatoid (SAR) (1) and poorly differentiated carcinomas (PDC) (5), all with previous FNA material, were identified. These 43 FNA specimens were submitted for IHC staining with two AD markers (TTF1 and MOC31) and two SQC markers (p63 and cytokeratin 5 [CK5]). IHC staining was considered positive for SQC if both SQC markers were positive. IHC staining was considered positive for AD if at least TTF1 (a lung AD marker) was positive. In addition, the specific cytomorphological features of AD (gland formation, cytoplasmic mucin, and SQC keratin, intercellular bridges) were sought in the cytology material. Based on the cytomorphology and IHC analysis a cytological diagnosis of AD or SQC was rendered and compared to the gold standard histological diagnosis.
Results: The results of the cytomorphological and IHC analysis of 42 of the 43 cytology cases (excluding the single SAR case) are summarized in Table 1. The histologically diagnosed SAR carcinoma was also called SAR carcinoma on cytology and was negative for all four IHC stains. After completing the cytomorphological and IHC analysis of all 43 cytology specimens, 14 cases were still unclassifiable as AD or SQC, either by cytomorphology or by IHC analysis. The final resolution of these 14 cases is shown in Table 2.
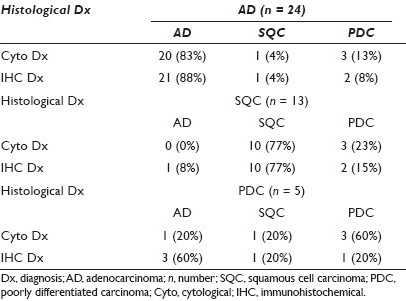
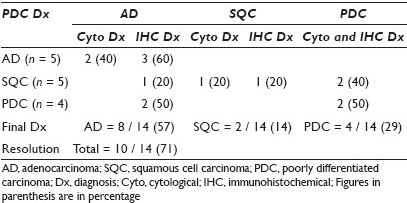
Conclusions: When compared to histology, accurate cytologic subtyping of lung carcinomas can be accomplished on FNA material using both cytomorphological and immunohistochemical methods. Immunohistochemistry was surprisingly only slightly superior to cytomorphology in the subtyping of lung AD and SQC. In cases where one method was unable to classify the tumor the other method played a complementary role and resolved the diagnosis in 71% of the cases. Of the five cases that were diagnosed histologically as poorly differentiated carcinoma, cytomorphology or immunohistochemical staining of the cytology material was able to definitely classify four of these as AD or SQC. The combination of cytomorphological and immunohistochemical analysis helped to accurately subtype the majority of lung carcinomas on cytology specimens, including tumors being classified as poorly differentiated carcinoma on histology. In some cases the cytomorphological and immunohistochemical analysis of the cytological material may be superior to histology. Despite the advent of the recent immunohistochemical stains, a prudent cytological practice should combine cytomorphological and immunohistochemical analysis for the accurate classification of these tumors.
104: Diagnostic accuracy of routine Cytology, cell block preparation and fluorescence in-situ hybridization for the detection of neuroendocrine tumors in bronchial brush specimens
Jordan Reynolds, MD, Jesse Voss, CT(ASCP), Shannon Brankley, CT(ASCP), Jill Caudill, SCT(ASCP), Michael Henry, MD, Amy Clayton, MD, Kevin Halling, MD, Aziza Nassar, MD
Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota
Introduction: Bronchial brush (BB) cytology carries a low sensitivity for detecting neuroendocrine carcinoma (NEC) and typical carcinoid (TC) tumors of the lung. The aim of this study is to investigate the detection of TCs by routine cytology on BB, as well as ancillary testing, including cell block (CB) preparation and fluorescence in-situ hybridization (FISH), using the LaVysion™ probe set.
Materials and Methods: Lung biopsy or resection specimens containing the term ‘neuroendocrine’ or ‘carcinoid’ in the diagnosis were searched, from 2008 to 2011. Residual BB specimens retained in the (PreservCyt Hologic, Inc. Bedford, MA) media were retrieved and a ThinPrep® slide (Hologic) was prepared for FISH analysis utilizing probes to pericentromeric regions of 6p11 and the locus-specific regions of 7p12 (EGFR), 8q24 (MYC) (Abbott Molecular Inc., Des Plaines, IL), and 5p15. Slides were screened for chromosomal gains or losses by a technologist. A CB with H and E and IHC for chromogranin and synaptophysin were prepared from the remaining BB specimen. A cytopathologist and a fellow screened the BB slides for tumor cells and atypical features. Patient demographic and clinical follow-up information was collected from the medical records.
Results: From 2008 to 2011, 187 cases (mean age 75) had the diagnosis of NEC or TC. Sixteen had residual BB cytological material within one year of the diagnosis and were used to make 16 FISH and 15 cell blocks for additional analyses [Table 1]. Nine tumors had a central location and seven were peripheral. Most TCs were < 2 cm in size (< 1 cm, n = 6; 1 – 2 cm, n = 6; > 4 cm, n = 4). Three of three primary NEC (1SCLC, 2TC) that were positive by FISH were centrally located with sizes of 3 cm, 1.8 cm, and 2 cm. The SCLC showed polysomy (86% abnormal cells), while the two TCs showed a gain of 7p12 (15% abnormal cells) and a gain of 5q15 (72% abnormal cells). Two of three TC cases positive by FISH (1 SCLC and 1 TC) also had CBs positive for chromogranin and synaptophysin. Cytology diagnosed one case as positive for malignancy (SCLC), one as suspicious for adenocarcinoma, and 14 as negative for malignancy. After a retrospective rescreening of all cases, only one additional TC was diagnosed on BB and it demonstrated medium-sized, bland nuclei, vague rosetting, and evenly distributed chromatin with small nucleoli. This case was positive by FISH and CB. Thirteen of fifteen CBs were negative, showing macrophages and bronchial cells, indicating lack of tumor sampling. For the detection of all NECs by BB sampling, the sensitivities were 6.25% for cytology, 12.5% for CB, and 31.3% for FISH.
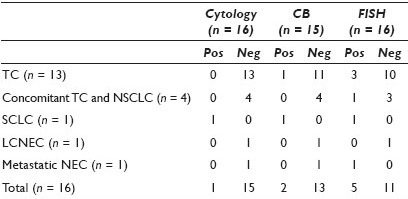
Conclusions: TCs are difficult to detect by BB cytology, This is most probably due to lack of tumor cells present in the specimen. Performing CB on all cases detected only one additional TC, while FISH detected three additional cases. Further studies are needed to explore the role of FISH and cytology for the detection of clinically apparent NEC centrally located tumors using bronchial brush specimens.
105: Clinical characteristic of pediatric population undergoing bronchoalveolar lavage for lipid laden macrophage index
Alice Coogan, MD, Joyce Johnson, MD, Catherine Smith, MD
Pathology, Vanderbilt University Medical Center, Nashville, Tennessee
Introduction: Chronic respiratory symptoms lead to consideration of aspiration in pediatric patients. The lipid-laden macrophage index (LLMI) semi-quantitatively evaluates alveolar macrophage lipid content in bronchoalveolar lavage (BAL) specimens and is used for evaluating chronic aspiration. The majority of LLMI studies are negative. The clinical setting(s) in which this test is most useful has not been established.
Materials and Methods: One hundred sequential pediatric (< 18 years) BAL specimens, from September 2008 to October 2009, were reviewed. Charts were reviewed for age, presenting symptom(s), and underlying disease(s). The Ding modification of the Colombo scale was applied, with a score of 5 considered positive. Patients were categorized into nine clinical groups: Cystic fibrosis (CF), transplant (including solid organ and bone marrow), recurrent pneumonia, airway obstruction, cardiac abnormalities, congenital pulmonary abnormalities, prematurity / failure to thrive (FTT), chronic cough otherwise healthy, and reactive airway disease (RAD) / asthma.
Results: Twenty-three of the 100 studies were positive. The average age of the positive group was 4.3 years; the average of the negative group was 5.8 years [Table 1].
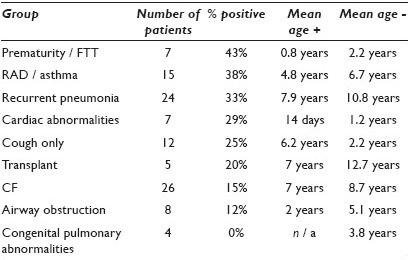
Conclusions: Most BAL samples were from patients with CF or recurrent pneumonias. The average age of positive patients was younger than that of the negative ones. This held true for eight of the nine clinical groups, the exception being chronic cough only. The highest percent of positive studies was in the prematurity / FTT group, followed by RAD / asthma, and recurrent pneumonias. None of the children with congenital pulmonary abnormalities had a positive study. CF patients were unlikely to have a positive test. LLMI may be best suited for identifying increased pulmonary lipid in younger children and those with prematurity / FTT, RAD / asthma, and recurrent pneumonias, and in older, otherwise healthy children with chronic cough.
106: Cell block examination is critical for sarcoidosis diagnosis by transbronchial ultrasound-guided mediastinal lymph node fine needle aspiration
He Wang, MD, PhD1, Akshatha Rao, BS2, Anthony Lafranco, MD2, Anil Vachani, MD2, Andrew Haas, MD, PhD2, Prabodh Gupta, MD1
1Pathology, Hospital of University of Pennsylvania, Philadelphia, Pennsylvania; 2Pulmonary Medicine, Hospital of University of Pennsylvania, Philadelphia, Pennsylvania
Introduction: Sarcoidosis, a multiorgan disease, presents with intrathoracic lymphadenopathy in more than 85% of the patients. Transbronchial lung biopsy (TBBx) has been the standard approach for the diagnosis of pulmonary sarcoidosis; however, recent studies suggest that endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is safer, with a superior diagnostic yield. Our center is one of the first to adopt EBUS-TBNA in sarcoidosis diagnosis in North America, with onsite Diff-Quick smear interpretation by cytopathologists, with variable degrees of training and experience, as well as cell block preparation, for all cases.
Materials and Methods: In this study, we report our experience with EBUS-TBNA in a total of 61 consecutive patients (female: 33, 54.1%) from 2008 to 2010, with clinical suspicion of sarcoidosis. They all underwent EBUS-TBNA using an Olympus EBUS-TBNA endoscope. One to three mediastinal lymph nodes (LN) were sampled (max. 5 passes / site) using a 21- or 22-gauge needle. The last one to two FNA specimens / site were collected in Normosol for additional studies including cell block preparations, they were not examined on site.
Results: A definitive diagnosis of sarcoidosis, based on the presence of non-necrotizing granulomas identified by either EBUS-TBNA or TBBx examination, as well as clinical indication, was made in 46 patients (73.7%, 45 patients by aspiration or biopsy, 1 patient by other clinical information); an alternative diagnosis (pneumonia, carcinoma, and lymphoma) was established in 11 patients (18%); the last four patients remained clinically suspicious for sarcoidosis after our diagnostic procedures. Of the 46 sarcoidosis patients, 37 patients were diagnosed with EBUS-FNA (80.4%), 10 out of the 37 patients (27.0%) were diagnosed (7 patients) or suspected (3 patients) onsite. Of the 37 patients diagnosed by EBUS-TBNA, LN sampling was done in one (17 patients, 17 LNs), two (14 patients, 28 LNs) or three (6 patients, 18 LNs) locations. Granulomas were observed in 17 / 17 LNs, 20 / 28 LNs, and 13 / 18 LNs, respectively. In the 46 sarcoidosis patients, the diagnostic yield of LNs at different locations varied dramatically: 50% in R4, 67.9% in the subcarinal, 80% in R11, and 100% in the R12 sites. A total of 34 patients underwent both EBUS-FNA and TBBx, the diagnoses from the two approaches were identical in 22 patients (64.7%); TBBx independently identified sarcoidosis in eight patients, whereas, EBUS-TBNA independently identified sarcoidosis in four patients.
Conclusions: Our study indicates that cell block preparation is valuable for EBUS-FNA diagnosis of sarcoidosis. On site interpretation appears to be experience- and preparation-dependent. EBUS-TBNA and TBBx are effective and complimentary tools for mediastinal LN biopsy. In this study, concomitant bronchoalveloar lavage or bronchial washing were not useful in establishing the finial diagnosis. Laterality (right side), size of the lymphadenopathy, and cost effectiveness of EBUS-TBNA are areas of interest for further studies.








