Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
1: Cytological assessment of estrogen receptor, progesterone receptor, and HER2 status on distant metastases of breast carcinoma
Ryan Des Jean, MD, Marcia Edelweiss, MD, MaryAnn Friedlander, MPA, CT(ASCP), Silvia Babore, CT(ASCP), Muzaffar Akram, HT, Melissa Murray, DO, Edi Brogi, MD, PhD
Pathology, Memorial Sloan-Kettering Cancer Center, New York, New York
Introduction: The assessment of the estrogen receptor (ER), progesterone receptor (PR), and HER2 status of metastatic breast carcinoma (MBC), using a cytology material, is relatively uncommon. Furthermore, some reports indicate that ER, PR, and HER2 status of breast carcinoma (BC), as determined by immunohistochemistry (IHC), can change in metastatic lesions compared to the primary tumor (PBC), with discordance in up to 30 – 40% of the cases. To address these issues, we compared the results of ER, PR, and HER2 stains (IHC) on paired surgical samples of PBC and cytology material (CYT) from metastatic breast cancer (MBC).
Materials and Methods: We searched our files for patients (pts) with CYT of MBC with IHC results, between 2007 and 2009. CYT IHC was compared to PBC IHC. Any discrepant IHC result was retested on the CYT of the MBC, if available. Patient demographics, and HER2 FISH status of the PBC and / or MBC, if available, were also recorded. HER2 scoring followed the ASCO / CAP guidelines [Table 1].
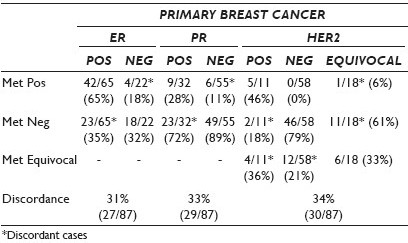
Results: Eighty-seven patients with median age of 55 years (range 28 - 80) fulfilled the study criteria. The PBC was invasive ductal (72 / 87; 83%), invasive lobular (6 / 87; 6%), and mammary (9 / 87; 10%). Nineteen MBCs involved the liver, 19, the lymph nodes (only two axillary), 16, the bone, 14, the lung, nine, the soft tissue, two, the adrenal, two, the mediastinum, two, the pleura, and four, the body fluids (two pleural, one CSF, one ascite). IHC was performed on ThinPrep® (20 / 87; 23%) and cell block (CB) (67 / 87; 77%). Table 1 summarizes the IHC results on MBC and PBC. There were 27 ER discrepant cases, of which four were positive on CYT, and 29 PR discrepant cases, with six positive in CYT. HER2 FISH on CYT, performed in 21 cases, allowed to definitively classify 13 MBCs, of which 12 were equivocal and one was negative on IHC, and five with HER2 gene amplification and eight without. Three patients had CYT and core biopsy from the same MBC; IHC on the core biopsy yielded the same results as CYT.
Conclusions: IHC performed on the cytology material of distant metastases of breast carcinoma has good concordance with IHC of the primary tumor. The biological significance of the discordant IHC profiles remains unclear and must be explored clinically. Our results also demonstrate that cytology material is suitable for HER2 FISH evaluation and its use can provide the relevant information for patient treatment.
2: Sclerosing adenosis of the breast: A restrospective review of fine needle aspiration features and correlation with the corresponding core-needle biopsy features
Uma Kundu, MD, Yun Gong, MD
Department of Pathology, Section of Cytopathology, MD Anderson Cancer Center, Houston, Texas
Introduction: Although the histological diagnosis of sclerosing adenosis (SA) of the breast is usually straightforward, the cytological diagnosis may be difficult due to the lack of well-defined features in the current literature. Published cytological studies on SA are sparse and are almost always represented by small cohorts or case reports. To improve on the diagnostic accuracy of SA on fine needle aspiration (FNA), we reviewed the cytological features of SA on FNA samples in conjunction with the histological findings on the corresponding core-needle biopsy (CNB) samples.
Materials and Methods: We searched our pathology database for breast lesions with a diagnosis of SA on CNB between January 2003 and February 2010. We subsequently searched for the corresponding FNA cases that were previously or concurrently sampled from the same lesions. We identified a total of 27 SAs that were sampled both by FNA and a concurrent / subsequent CNB of the same lesion. Clinical and radiographic data for each case was also obtained.
Results: The patients’ ages ranged from 40 to 68 years (average, 51.2 years). Radiographically, the target lesions ranged in size from 0.4 to 4.2 cm (average, 1.16 cm). The lesions were described as ill-defined hypoechoic in 12 cases, hypervascular in one case, a well-circumscribed mass in four cases, an ill-defined mass in five cases, mass / NOS in four cases, and suspicious for carcinoma in one case. A CNB slide review identified SA in 10 (37%) cases, SA with radial scar / complex sclerosing lesion or other benign lesions in 11 (41%) cases, and SA with atypia in six (22%). FNA diagnoses were as follows: Benign lesion (mostly fibrocystic changes or fibroepithelial lesions) in 21 (78%) cases and atypical / suspicious in six (22%) cases. Of the 22 FNA cases available for slide review, low cellularity was found in 13 (59%), fibrotic stromal fragments in 20 (91%), and dyscohesive / isolated epithelial cells in five (23%). Small tubules (some with angulated configuration and open-ended lumens) and solid nests / cords of epithelial cells were seen in all (100%) cases and myoepithelial cells within these cell groups were often diminished or lacking (n = 19, 86%), raising a concern of low-grade ductal / tubular carcinoma or lobular neoplasm. However, these cell groups / tubules were seen focally in most cases along with overtly benign cells. The epithelial cells were uniform and bland in 20 (91%) cases.
Conclusions: Sclerosing adenosis can pose diagnostic dilemmas in cytological and radiological interpretations. Although the configuration and architecture of some cell groups may resemble that of low-grade carcinoma, the focality and paucity of these groups along with minimal to no nuclear atypia are suggestive of SA. Familiarity with the cytological features of SA can minimize false-positive interpretations on FNA and tissue confirmation is recommended for the challenging cases.
3: Atypical epithelial cells in fine needle aspiration biopsy of breast lesions: Histological follow-up and sources of equivocal cytological diagnosis
Gene Landon, MD, Qiusheng Si, MD, Ming Guo, MD, Nour Sneige, MD, Yun Gong, MD
Pathology, MD Anderson Cancer Center, Houston, Texas
Introduction: An indeterminate diagnosis made on fine needle aspiration (FNA) samples of breast lesions can cause dilemmas in the clinical management. Identifying the histological follow-up and potential sources of indeterminate diagnoses will improve diagnostic certainty.
Materials and Methods: In this retrospective study, we identified 143 FNA cases that had originally been diagnosed as ‘atypical’ or ‘suspicious for carcinoma’ between July 2002 and June 2010, and for which concurrent or subsequent core needle biopsy (CNB) samples of the same lesions were available. The histological follow-up information was recorded, and the cytological slides reviewed (available in 131 cases).
Results: The patients’ mean age was 52 years (range, 19 – 85 years). The CNB diagnoses included carcinoma in 66 cases (46.1%), benign in 75 (52.5%), and indeterminate in two (1.4%); subsequent excision was performed in 57, 13, and two lesions of each category, respectively. Of the 66 carcinomas, 39 (59.1%) were diagnosed as invasive ductal carcinoma (IDC), 11 (16.7%) as invasive lobular carcinoma (ILC), five (7.6%) as mixed IDC and ILC, one (1.5%) as metaplastic carcinoma, eight (12.1%) as ductal carcinoma in-situ (DCIS), and two (3.0%) as lobular carcinoma in-situ. Nuclear grade 1 was found in 29 (44.0%) tumors, grade 2 in 33 (50.0%), and grade 3 in three (4.6%). Of the 75 benign lesions, 13 had been excised; one was diagnosed as atypical ductal hyperplasia (ADH) on CNB, and turned out to be grade 1 IDC on excision. Of the remaining 74 lesions, 15 (20.3%) were fibroadenoma, 13 (17.6%) benign epithelium (with or without stromal fibrosis), 10 (13.5%) ADH, nine (12.2%) adenosis (including two sclerosing adenosis and one atypical microglandular adenosis), 10 (13.5%) fibrocystic change or ductal hyperplasia, five (6.7%) papilloma, two (2.7%) pseudoangiomatous hyperplasia, and 10 (13.5%) others. Two CNB indeterminate lesions were found to be low-grade DCIS on excision. Cytologically, scant cellularity, loss of cohesion, morphological distortion due to fibrosis, small tubular architecture, diminished myoepithelial cells, nuclear crowding or enlargement, and prominent nucleoli were the common contributory features.
Conclusions: Approximately half of the cytologically indeterminate lesions are malignant, indicating a necessity for further histological confirmation. Low-intermediate-grade carcinoma, fibroadenoma, ADH, adenosis, and stromal fibrosis constitute most of such cases. Familiarity with the cytological features of these lesions will improve diagnostic certainty.








