Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
4: Using ASC: SIL ratio, HPV, and interobserver variability to assess and monitor cytopathology fellow training performance
Ivan Chebib, MD, FRCPC1, Rema Rao, MBBS2, David Wilbur, MD3, Rosemary Tambouret, MD3
1Department of Pathology, University of Calgary, Calgary, Alberta, Canada; 2Department of Pathology and Laboratory Medicine, University of California, San Francisco, San Francisco, California; 3Division of Cytopathology, James Homer Wright Pathology Laboratories, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts
Introduction: The goal of the cytopathology fellowship is to advance the resident beyond minimal competency of independent sign-out to a level of expert proficiency. We assessed whether routine cytopathology monitors can be applied to gauge the progress of the cytopathology fellows.
Materials and Methods: The laboratory information system was searched for all cases of cervical cytology interpreted by five cytopathology fellows who trained at MGH between 2007 and 2010. The patient demographics, final pathology result, HPV-test data, and the fellow's original interpretation were recorded. The ASC: SIL ratio was calculated and compared with those of the cytopathologist. Inter-observer variability between the fellow and the pathologist was determined by using the Cohen κ-coefficient.
Results: The five fellows reviewed an average of 490.8 cases per annum. The average κ-value between the Fellow and pathologist interpretation was 0.74 (95% CI 0.69 – 0.79, range 0.67 – 0.80). The percentage of cases of ASC-US with agreement between the pathologist and the fellow ranged between 64.4 and 77.0%. The Fellows had a tendency to interpret ASC-US cases as NILM (range 13.2 – 22.7%) or LSIL (range 2.2 – 13.2%). The average ASC : SIL ratio for the Fellows was 1.15 (95% CI 0.92 – 1.38, range 0.84 – 1.40) with four Fellows having lower ASC : SIL ratios than the cytopathologist, whose average ASC : SIL for the same case cohort was 1.30 (95% CI 1.08 – 1.52, range 0.97 – 1.61). Of cases interpreted as NILM by the Fellow and ASC-US by the pathologist (13.2 – 22.7% of cases), between 25.9 and 44.0% were HPV+, intermediate between that expected for ASC-US (40+%) and for NILM (5 – 10%), possibly because the Fellows were more aggressive in interpreting NILM and / or pathologists were more cautious, rendering an ASC-US interpretation and maximizing the sensitivity. Those cases interpreted as LSIL by the Fellow and ASC-US by the pathologist ranged between 2.2 – 13.2% of the cases, with HPV+ between 61.1 – 100%, indicating that The Fellows could be more aggressive in their interpretations of borderline ASC-US cases as LSIL.
Conclusions: Cytopathology Fellows tend to be more aggressive in interpreting NILM and LSIL, based on subsequent HPV results, than pathologists who render more cautious interpretation of ASC-US, in borderline cases. Using this data, a framework can be applied to measure and improve a Fellow's performance and maturity during their training year by not only assessing the performance on a case-by-case basis, but also measuring ASC : SIL, HPV-status, cyto–histo correlation, κ-value, and review of discrepant cases.
5: iPad and cytopathology: Content creation and delivery
Brian Collins, MD
Department of Pathology and Immunology, Washington University, St. Louis, Missouri
Introduction: The iPad is a tablet-style computer device gaining wider use. It represents a newer style of hardware device with high quality visual capabilities and thin physical design. With abundant memory, storage space, portability and wireless connectivity, it is an excellent platform for storing and easily accessing dynamic medical information. With a high resolution 9.7 inch screen, it is particularly suitable for displaying images. A long battery life of ten hours enhances its portability as a point-of-care information access model. The epub 3.0 standard permits the creation of electronic books (e-books), which can be accessed across a variety of different platforms, including the iPad. Cytopathology-based data in the epub e-book format was developed and designed for utilization on the iPad.
Materials and Methods: The epub standard is designed for the creation of electronic books with text and images that can be accessed across a variety of different hardware platforms. To create this, the Adobe InDesign CS5 software was used, to design and organize the previously created text and image content on a MacBook Pro. The InDesign created a table of contents, organizing the content into chapters, and inserting jpg photomicrographs. Within the text, references were embedded and hyperlinked to online resources. Interactive elements and hyperlinks were designed to interface with the native software and wireless iPad connectivity. InDesign exported the final design in the epub file format as a single, complete file. This file was transferred to the iPad via iTunes software by a simple drag and drop method. The iPad required the iBook app to be installed, in order to access the e-book.
Results: The cytopathology e-book provided searchable, interactive text and references with high resolution cytopathology photomicrographs, which were conveniently stored and accessed on an iPad. Interaction with the content occurred by opening the textbook in the iBook app, and reading and interfacing with the data by touch. A single location or page was bookmarked electronically, which permitted a future reference after exiting. The video was embedded directly. Individual medical references were accessible through embedded hyperlinks, and the iPad seamlessly downloaded them via the wireless connection and built-in web browser for an instant review with a single touch of a finger. Hyperlinked online web resources were available in the iPad through the e-book, including web sites (ASC web site), video (YouTube), and audio. Individual images were viewed with the text and as stand-alone full screen images. The native zoom function of the iPad permitted closer examination of image details. The content could be copied, pasted, printed, and emailed. Video mirroring allowed the iPad to connect to a larger, external HDTV screen for presentation purposes. A single e-book can vary in size from 1MB to 100s MB, and with a capacity up to 64 GB, there was ample storage space.
Conclusions: The iPad is a dynamic, interactive tablet-style computer device with significant potential for improved access and organization of medical information. By using the epub format, a cytopathology based e-book has been created, which has taken advantage of its strengths and capabilities. The iPad, with the epub e-book format, demonstrates its capacity to provide interactive cytopathology content in a portable, easily accessible device.
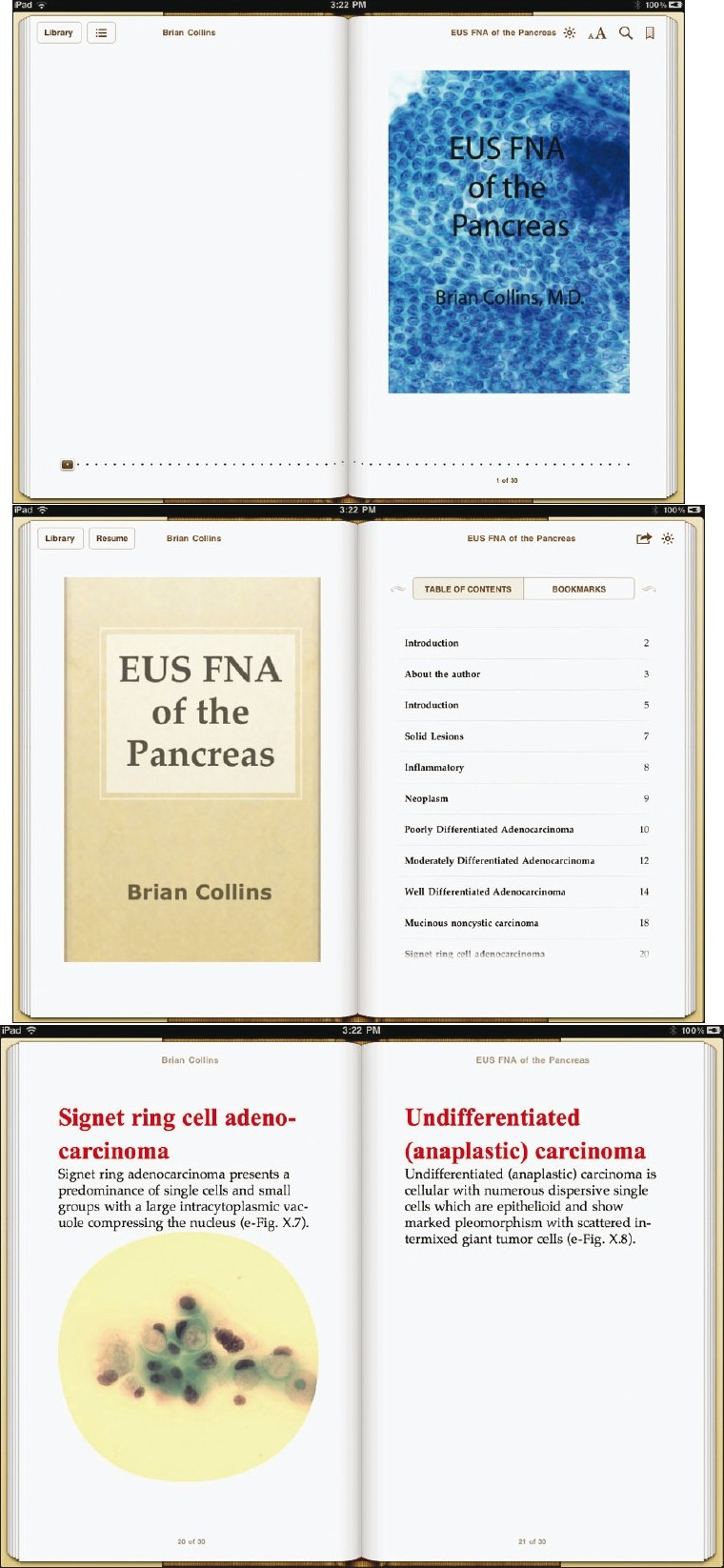
- Front page of the ebook. (iPad iBooks screen capture)
- Table of contents can be viewed and each individual chapter can be accessed directly. (iPad iBooks screen capture)
- Individual chapter headings show a combination of text and images.(iPad iBooks screen capture)
6: The use of journaling in cytotechnology education: Live experience of a cytotechnology educator
Linda Hoechst, MA, SCT(ASCP), CT(IAC)
Clinical Laboratory Science, Cytotechnology Program, Saint Louis University St. Louis, Missouri
Introduction: Adult education tenets hold that learning be more learning-centered than teaching-centered. Toward this goal, this researcher has implemented the use of journaling within a Cytotechnology Education Program. In order to establish rapport and mutual trust between the learner and the instructor various methods may be used to accomplish this goal. Among these is the use of journaling.
Materials and Methods: Journaling as a self-reflective method has been explored in the literature. The purpose of this study is to determine how it performs as a self-evaluative method in Cytotechnology Education.
Students are required to submit journal entries weekly during the Program. Information requested in these entries include: The material they understand; the material that is challenging to them; the material they find difficult; how they would like the material to be presented; what works and does not work for them; any personal issues that may be influencing their ability to grasp the content; and any other comments that may provide information to determine an action plan toward their academic success. Every one of these items need not be included in every journal entry. Over the span of thirteen years, this researcher has used journaling as a means of assessing student educational needs, challenges, and impediments. Through an evaluation of the information provided by the students and their feedback about this method, data have been generated identifying the benefits of its use in Cytotechnology education.
Results: The data support the use of this method in Cytotechnology education. It has been an important generator of trust and rapport among students and the instructor. It has identified the best teaching methods and strategies for each individual student. It has provided an explanation of outside influences that impact learning. It has identified issues before they become problems. It has indicated student dissatisfaction in a timely matter, to be dealt with before course evaluations are written at the end of the course.
Conclusions: Journaling in Cytotechnology Education is an important and useful tool in the academic success of Cytotechnolgy students. It is a cost-effective method to assess Cytotechnology Education as a dynamic process and enables timely response to issues that arise in the teaching and learning process.
7: The cytotechnologists and their role in tissue analysis at the mayo clinic
Lindsey Kane, SCT(ASCP)1, Kandelaria Rumilla, MD2, Angela Sorenson, MA, SCT(ASCP)1
1Cytopathology, Department of Laboratory Medicine, Mayo Clinic, Rochester, Minnesota; 2Molecular Genetics, Department of Laboratory Medicine, Mayo Clinic, Rochester, Minnesota
Introduction: Over time, the Cytotechnologists’ (CT) workload has decreased, with a significant change in the cervical Pap volumes, while the pathologists’ workload has seen a significant increase, specially in the area of molecular genetic testing. Our laboratory wanted to find a way to utilize the CTs’ morphological skills to fill the void left by the decline of Pap volumes and a way to reduce the pathologists’ workload. It was determined that the CTs’ cytology skills could convert to the review of the histological sections of a tissue. This would allow a group of CTs’ to collaborate with the molecular genetics laboratory, by being a part of the pre-analytic process of molecular tumor testing and documentation.
Materials and Methods: Meetings began with two consultants from the molecular genetics laboratory, to determine the responsibilities of the CTs. Documentation processes were modified to incorporate CTs into the tissue review process. CT responsibilities would include documentation for materials received, tumor–type and source, appropriateness of the material for the test ordered, including the presence / absence of the normal estimating percent of tumor nuclei in the tissue sample, and immunohistochemical stain interpretation, all of which would then be subject to review by the pathologist. To train for this new workflow there were group scope sessions and individual sign-out sessions with pathologists. Collaborating with the pathologists one-on-one allowed the CTs to quickly gain an understanding of the testing, tissue review, to estimate the percent of the tumor nuclei.
Results: To determine if the CTs were providing significant time saving for the pathologists, the times were recorded along with documenting any changes made to the case. The changes were classified as major (could impact test performance or result), moderate, minor (not likely to impact test), and judgment calls. When time recordings were reviewed it was found that the average pathologist's full-time equivalent (FTE) used per case was 0.000355 prior to the CT review and after the CTs were introduced to the process the average FTE used per case was 0.00038. When the overall average time per case for each pathologist was reviewed it was found that two pathologists saw substantial time improvements, by greater than 50%, while two saw only minor improvements. When the changes were charted out the two pathologists with substantial time saving had significantly fewer minor changes made to the cases. It also showed that those showing little time improvement had considerably more minor changes made on each case. Quarterly a set of de-identified cases circulate internally to the whole group and the results are compared, particularly percent tumor nuclei. A majority of the minor changes fall within our gold standard for QA case review. With this in mind the group went to minimizing those changes that would not impact the test results, in the hope of seeing a more significant time saving. When the time saving was recorded again a year later and compared to the time taken prior to the CT's reviewing the cases, it was seen that the average time saving was 35%.
Conclusions: We found the updated time saving to be valuable and helpful for the pathologists. One reason we may not be maximizing efficiency is the turnover of the Fellows rotating through the area. Our average pathologist FTE per case will continue to be monitored over time and the QA cases will also continue to be used, to hone both the pathologist and CT review skills.
8: Telecytology for immediate assessment of endoscopic ultrasound-guided fine needle aspiration: Improved pathologist efficiency, and a valuable educational tool
Jonathan Marotti, MD, Vickie Johncox, CT(ASCP), David Ng, MD, Vijayalakshmi Padmanabhan, MBBS, MD
Department of Pathology, Dartmouth Hitchcock Medical Center, Lebanon, New Hampshire
Introduction: In a tertiary academic medical center, onsite evaluation of fine needle aspiration (FNA) procedures can take anywhere from 30 minutes to two hours of the cytopathologist's time, given the distance from the Department, and the training and the experience of the performer. Telecytology is being increasingly used as an alternative for onsite cytopathologist evaluation. One of our department's quality incentives for 2010, was the reduction of cytopathologist procedure time by 50%, improving the efficiency. The aim of this study was to evaluate the role of telecytology for immediate assessment of endoscopic ultrasound (EUS)-FNA procedures, to improve the efficiency.
Materials and Methods: Following an adaptation period of one week, which included performing onsite evaluation in tandem with the transmitted image review, telecytology was incorporated and evaluated over a 10-month period. Using an Olympus BX41 microscope and Olympus DP72 camera with Olympus CellSens software, dynamic images of the air-dried Diff-Quik® stained smears were transmitted by the cytopathology Fellow or the cytotechnologist, using a secure internet connection. The cytopathologist remotely accessed the real-time images on a computer and rendered immediate assessments, while communicating over the telephone with the cytopathology Fellow, who would communicate with the clinicians. Cytopathology Fellow / cytotechnologist procedure time and cytopathologist procedure time for each EUS-FNA was recorded.
Results: Two hundred and forty-nine EUS-FNA procedures were performed during the 10-month period. Overall, 164 (66%) procedures utilized telecytology. By the end of the 10-month period, the utilization rate was greater than 95%. The average cytology fellow / cytotechnologist procedure time, with and without telecytology was 1.1 hours. The average cytopathologist procedure time without telecytology was 0.74 hours; the average procedure time with telecytology was 0.2 hours. A total of 88.56 cytopathologist hours was saved. The Fellows greatly appreciated the autonomy and the ability to communicate with the clinical staff. The immediate assessment diagnosis matched the final diagnosis in all but one case, where the final diagnosis was suspicious and the immediate assessment positive for malignancy.
Conclusions: Incorporation of telecytology for immediate assessment of EUS-FNA successfully increased cytopathologist efficiency. The department's incentive goal was met and surpassed. It allowed the cytopathology Fellow to interact with the clinical staff as a junior consultant. Telecytology is now routinely incorporated in greater than 95% of all EUS-FNA procedures in our hospital, reducing cytopathologist time by at least 70%. The projected 2011 cytopathologist time saving is 174.96 hours. Furthermore, telecytology augmented the cytology fellowship training program.








