Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
9: Non-urothelial carcinoma of the urinary bladder — Diagnosis on urine cytology
Manju Aron, MD, Maureen Croyle, CT(ASCP), Donna Hansel, MD, PhD, Christine Booth, MD
Pathology, Cleveland Clinic, Cleveland, Ohio
Introduction: Urothelial carcinoma of the urinary bladder comprises 90% of all bladder carcinomas. Squamous cell carcinomas, adenocarcinomas, and small cell carcinomas of the urinary bladder are rare and account for less than 5, 2, and 0.5% of all bladder carcinomas, respectively. Urine cytology is an efficacious diagnostic tool, with a high specificity and sensitivity in the diagnosis of high-grade urothelial carcinomas. The role of urinary cytology in the preoperative diagnosis of the above-mentioned tumors has rarely been reported. We report our experience on these rare tumors.
Materials and Methods: Between the period of 1983 and 2009, there were a total of 25 cases of small cell carcinoma, 20 of squamous carcinoma, and 10 of adenocarcinoma, wherein prediagnosis urine cytology was available. However, the cytology slides were available for review only from 1997 onwards. Only those cases with available cytology slides were included in the study.
Results: There were eight cases (12 samples) of small cell carcinoma, four cases (6 samples) of squamous cell carcinoma and four cases (5 samples) of adenocarcinoma. The cytological diagnoses of these samples are listed in Table 1. Of the nine samples of small cell carcinoma, categorized as atypical, suspicious for carcinoma, three (33%) were categorized as suspicious for small cell carcinoma, while the others were not further classified, due to limitations of cellular preservation. In the squamous cell carcinoma subgroup, the samples with ‘atypical, suspicious for carcinoma’ diagnoses did not show any keratinization and were interpreted as atypical urothelial cells. All the adenocarcinomas categorized as negative by urine cytology had sparse cellularity and did not reveal any atypical cells on slide review.
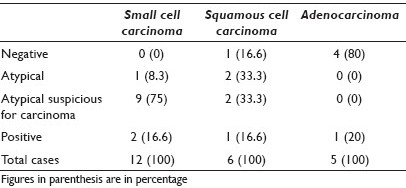
Conclusions: None of the samples of small cell carcinoma had a false negative diagnosis on cytology, while only one case of squamous cell carcinoma was diagnosed as negative. However, only one case of adenocarcinoma was diagnosed preoperatively. Although the sample size is small, this study highlights the relevance of urine cytology in the preoperative diagnosis of these rare non-urothelial tumors of the bladder.
10: Does routine preparation of multiple ThinPrep® and cell block slides improve the detection of malignancy in effusion fluid?
Charles Beavers, MD, Dustin Woods, MD, Sunati Sahoo, MD
Department of Pathology and Laboratory Medicine, University of Louisville Health Sciences Center, Louisville, Kentucky
Introduction: Cytology is the most accurate and cost-effective method of evaluating spontaneous effusions to rule out malignancy. The overall sensitivity of detecting malignant cells in an effusion is 70 to 90%. In effusions multiple factors, including the presence of markedly reactive mesothelial cells or few groups of atypical cells, can pose a dilemma for a definitive diagnosis. At our institution, we recently adopted a policy of preparing a duplicate ThinPrep® slide and slides from cell block for every effusion specimen routinely, with the aim of improving the sensitivity of detecting malignancy and minimizing the rate of ‘suspicious’ and ‘atypical’ interpretations. Prior to the new policy, one ThinPrep® slide was prepared, unless additional ThinPrep® slides and cell block were requested, based on the initial examination.
Materials and Methods: The study population comprised of 50 consecutive cases of effusions after the new policy (groups 1 and 2) and 50 cases before the new policy (group 3) was implemented [Table 1]. All the slides (a total of 150 ThinPrep® slides and 67 cell block slides) were reviewed separately by a cytopathologist, who was blinded to the original method of examination and clinical history. In each ThinPrep® slide an interpretation of ‘positive for malignancy,’ ‘negative for malignancy,’ ‘atypical,’ or ‘suspicious for malignancy’ and ‘scant cellularity’ was rendered.
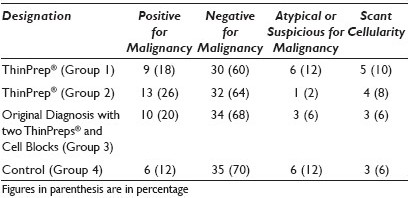
Results: The diagnostic categories from each group of 50 slides are summarized in Table 1. In the vast majority of cases, a definitive diagnosis of ‘positive for malignancy’ (up to 26%) or ‘negative for malignancy’ (up to 70%) was reached, based on the review of one ThinPrep® slide. The rate of ‘atypical’ and ‘suspicious’ interpretation ranged from 2 to 12% (average 7%) when one ThinPrep® slide was reviewed. However, that rate dropped to 6% when two ThinPrep® slides and cell block slides were available for interpretation. The rate of ‘scant cellularity’ did not improve significantly with an additional slide or with the cell block preparation.
Conclusions: Routine preparation of two ThinPreps® and cell blocks on effusion specimens is particularly useful in instances where the initial evaluation reveals atypical or suspicious groups of cells or when the differential diagnosis includes reactive mesothelial cells versus malignancy. Routine performance of multiple ThinPrep® slides or cell block on every effusion specimen is not cost-effective. Additional slides are also of little help in evaluating cases with inadequate fluid volume and scant cellularity.
11: Utility of special stains for opportunistic infections in bronchioalveolar lavage fluid
Ramneesh Bhatnagar, MD, Paul Staats, MD
Department of Pathology, University of Maryland Medical Center, Baltimore, Maryland
Introduction: Bronchioalveolar lavage (BAL) fluid can be analyzed for opportunistic infections by bronchial and sputum cultures, as well as molecular studies and serology. Along with microbiology, special and immunohistochemical stains for cytology are often performed. However, it remains uncertain whether special stains for organisms on cytology preparations provide substantial additional diagnostic sensitivity compared to microbiological tests and routine cytological preparations.
Materials and Methods: We retrospectively reviewed the cytology reports of all BAL specimens over a period of one year (2010). The results of routine stains (Diff Quick and Papanicolaou) as well as stains for microorganisms, Gomori methenamine silver stain (GMS), Acid Fast Bacilli (AFB), and immunoperoxidase stains for Cytomegalovirus (CMV) and Toxoplasma were recorded. All cases reported as positive for organisms were reviewed for confirmation by two pathologists, and the presence of organisms on routine stains, special stains, or both was noted. Such cases were also correlated with the microbiology results.
Results: A total of 476 cases were reviewed, of which 235 (49%) had special staining for GMS, 222 (47%) for CMV, 189 (40%) for Toxomplasma, and 111 (23%) for AFB. Of the 235 GMS-stained specimens, 19 (8%) were positive for Pneumocystis carinii (PCP). Evidence of PCP infection was visible on routine stains in all but one case (18 / 19), and it was more prominent with Papanicolaou staining. Candida was seen in 10 out of the 235 GMS stains (4.2%), and five out of the 10 cases had microorganisms readily identifiable on routine stains. There was one specimen (< 1%) positive for Aspergillus, and one other (< 1%) positive for Cryptococcus neoformans. Both of these cases required GMS staining, as the microorganisms were not visible on routine stains. All cases with positive cytology were also identified by microbiological methods (positive cultures or antigen detection). None of the specimens were positive for CMV, Mycobacteria, or Toxoplasma on cytology.
Conclusions: Special and immunohistochemical stains for microorganisms can be helpful in identifying specific pulmonary infections, particularly GMS staining for fungal organisms, compared to routine stains; however, microorganisms, when present, are usually visible on routine stains, and in this study have always been identified on microbiological studies of the BAL specimen, so the special stains have provided no improvement in the overall sensitivity for the detection of organisms. CMV, mycobacteria, and toxoplasma are relatively uncommon pulmonary infections, as supported by the lack of any positive immunostains in our study, so the utility of routine staining for CMV, mycobacteria, or Toxoplasma is limited, although cost-benefit analysis of routinely performing these tests is beyond the scope of this study.
12: Atypia in pleural effusions after lung transplantation
Maureen Croyle, CT(ASCP), Ghada Aramouni, CT(ASCP), Beverly Cash, CT(ASCP), Deborah Chute, MD
Department of Anatomic Pathology, Cleveland Clinic, Cleveland, Ohio
Introduction: Pleural effusions are frequent non-gynecological specimens. Many benign processes can cause significant reactive atypia in mesothelial cells, including infectious and inflammatory disorders. Pulmonary transplant patients are immunosuppressed, and therefore, at a higher risk for development of both malignant and infectious conditions. This study evaluates the clinical and pathological features of pleural effusions in patients, after lung transplantation.
Materials and Methods: All patients who underwent lung transplant and had post-transplant pleural fluid within the last five years were included. The initial cytological interpretation was recorded, and the slides were reviewed for cellularity, presence of inflammation, mesothelial cell features, and the presence of cell clusters. Follow-up clinical and pathological information was recorded from the time of effusion to the most recent transbronchial biopsy.
Results: Thirty-six (15%) patients with a total of 63 pleural effusions were included. The average time from lung transplant to pleural effusion was 10.7 months. Twenty-seven patients had bilateral lung transplants, and nine had a unilateral lung transplant. In nearly all patients (97%), the pleural effusion was ipsilateral to the transplanted lung. The original cytological diagnosis was negative in 59 (94%) effusions. Four effusions were suspicious for neoplasia. Mesothelial cellularity was low in almost all cases (94%). Inflammation was a frequent finding, chronic in 46 cases (73%) and acute in 12 cases (19%). Mesothelial cells often had prominent nucleoli (38%) and were vacuolated (35%). Mesothelial cell clusters were uncommon (25%), and clusters with community borders was only seen in one case. On follow-up, one effusion suspicious for malignancy was diagnosed with adenocarcinoma on pleural biopsy. In this case, there was high cellularity, the cell clusters had community borders, and the effusion occurred contralateral to the transplanted lung. The other three atypical effusions were from one patient, concerning a lymphoproliferative disorder, but follow-up was negative. Two patients with negative fluids were diagnosed with post-transplant lymphoproliferative disorder within one year of the pleural effusion. All other patients were negative for malignancy on all subsequent biopsies.
Conclusions: Reactive atypia and chronic inflammation are frequent findings in pleural effusions of lung transplant patients. However, cell clusters with a community border, as well as effusions involving the contralateral lung, should raise concern for a diagnosis of malignancy.
13: Cytomorphology of atypical teratoid / rhabdoid tumor in cerebrospinal fluid
Eric Huang, MD, PhD1, Miguel Guzman, MD2, Edmund Cibas, MD1
1Department of Pathology, Brigham and Women's Hospital, Harvard Medical School, Boston, Massachusetts; 2Department of Pathology, Children's Hospital Boston, Harvard Medical School, Boston, Massachusetts
Introduction: Atypical teratoid / rhabdoid tumor (AT / RT) is an extremely rare and highly aggressive intracranial neoplasm with a predilection to spread along the cerebrospinal fluid (CSF) pathways. The cytopathological characteristics of this tumor in the CSF specimens, however, have not been extensively studied. Here we report the pattern of CSF cytomorphology from a series of patients with histologically documented AT / RT.
Materials and Methods: We conducted a retrospective review of 36 malignant CSF specimens from eight patients with histologically confirmed AT / RT (all females; age range 0.8 to 9.6 years at initial diagnosis; mean age = 2.4 years) from 2001 to 2009. Cytospin preparations were made in all cases. In most cases, at least two slides were prepared with the Papanicolaou and / or Wright Giemsa stains.
Results: The CSF samples were predominantly sparsely cellular (67%; 24 / 36 cases) and the malignant cells were accompanied by lymphocytes and monocytes (69%; 25 / 36 cases). Two principal malignant cell types were seen: The most striking and recognizable form was a large, usually rhabdoid cell with an eccentrically placed nucleus, prominent nucleolus, and abundant cytoplasm, seen in 72% (26 / 36) of the cases. Some, but not all of these large cells contained the dense condensation of cytoplasm, characteristic of rhabdoid morphology. The second type of neoplastic cell had a ‘small cell’ appearance and was seen in isolation in 28% (10 / 36) of the cases. Both large and small malignant cells were seen in 31% (11 / 36) of the cases.
Conclusions: A significant proportion (28%) of AT / RT cases metastatic to CSF consisted of only the small cell component, without the large rhabdoid cells that were characteristic of this neoplasm. Familiarity with this pattern of spread was important in the differential diagnosis, with other small cell malignancies like medulloblastoma, which have a high propensity for spreading along the CSF pathways.
14: Immunoreactivity of the IMP3 antibody in malignant epithelial tumors and reactive mesothelial cells in serous effusions
Semra Karaburun, MD, Saverio Ligato, MD
Pathology, Hartford Hospital, Hartford, Connecticut
Introduction: The distinction between benign and malignant effusions can be a major diagnostic challenge in cytology. Several immunohistochemical / cytochemical antibodies have been studied as ancillary tools in the differentiation between benign / reactive and malignant effusions. The insulin-like growth factor II messenger RNA binding protein-3 (IMP3, also known as L523S) is an oncofetal RNA-binding protein, expressed during embryogenesis and in various malignancies. In this study, we investigate the use of IMP3 to help in the differentiation between benign and malignant cells in effusion cytology specimens.
Materials and Methods: A total of 33 (17 pleural, 15 peritoneal, and 1 pericardial) effusions, including 15 negative, 15 positive, and three atypical, but not diagnostic, effusion specimens were selected and stained with antibody to IMP-3 (clone 69.1; Dako, Carpinteria, California, USA). The intensity (scale 0-3+) and percentage of cells staining were evaluated, and a diffuse (>75%) staining with 2 – 3 positive intensity was considered positive.
Results: The immunohistochemical stain for IMP-3 / L523S showed positive staining in 11 (73%) of 15 malignant, two (66%) of three atypical, and one (7%) of 15 reactive effusions. The overall specificity for the diagnosis of malignancy with IMP-3 was 93%, whereas, the sensitivity was 73%. Positive and negative predictive values were 92 and 78%, respectively.
Conclusions: IMP3 / L523S antibody is a useful marker for the detection of malignant cells in serous effusions and it can be helpful in distinguishing neoplastic cells from reactive mesothelial cells in serous effusions. Our results are similar to the study previously performed by Ikeda Katusuhide in Japan.
15: The cytological appearance of a mixed malignant mesodermal tumor in pelvic washings: Correlation with histological findings
Ann Leathersich, MD, Kay Kasal, CT(ASCP), DengFeng Cao, MD, PhD, Hannah Krigman, MD
Pathology and Immunology, Washington University, St. Louis, Missouri
Introduction: A mixed malignant mesodermal tumor (MMMT) is an aggressive uterine tumor that typically occurs in women between the age of 50 and 80. MMMT accounts for approximately 2% of the endometrial primary tumors. As this tumor is rare, the findings on pelvic washing cytology are not well described. For this reason, we performed a study of pelvic washings obtained at the time of definitive resection for an MMMT. The goal was to identify the features specific to MMMT and to examine the spectrum of findings in this histologically diverse tumor population.
Materials and Methods: The pathology database was searched for all patients with a diagnosis of MMMT from 1995 to 2010. All cases with pelvic washing cytologies obtained at the time of definitive resection were selected for review. Pap stained, monolayer preparations from washings were reviewed and evaluated for the glandular component, stromal elements, and inflammation. The histological subtype of the MMMT, on definitive surgical resection, was also reviewed and compared with the elements shed into the pelvic fluid.
Results: Twenty-six positive pelvic washings were identified. Eight cases had a predominantly endometrial adenocarcinoma pattern. Three cases had a mixture of serous and endometrioid adenocarcinoma patterns. Two washings had a mixture of endometrioid and undifferentiated malignant cells. Five cases had predominantly small, undifferentiated malignant cells. In no cases, were definitive malignant stromal elements identified. The type of epithelium did not correlate completely with the reported histological subytpes. Five MMMTs with serous epithelium, on hysterectomy, had groups more reminiscent of adenocarcinoma, on the washings. Three patients with endometrial type adenocarcinoma on hysterectomy had serous appearing groups on washing, including one with psammomatous calcification.
Conclusions: A predominant histological pattern in uterine resections is not necessarily predictive of the pattern of malignant elements in pelvic washing cytology, for MMMT. This shift in pattern reflects the pluripotent nature of this neoplasm. A mixture of malignant epithelial types suggests an MMMT and warrants additional sampling, to demonstrate the presence of this particular subtype of malignancy.
16: Pericardial fluid cytology: Etiology and diagnostic accuracy. An analysis of 128 specimens from 113 consecutive patients over a six-year period
Lina Liu, MD, Ema Dragoescu, MD
Pathology, Virginia Commonwealth University Health System, Richmond, Virginia
Introduction: Pericardial effusion is a common finding in clinical practice with causes including: Infections, malignancy, connective tissue diseases, injury (post-trauma, postmyocardial infarction), metabolic causes (hypothyroidism, uremia), heart diseases (pericarditis, myocarditis, heart failure) or idiopathic causes. Pericardiocentesis (PC) is performed based on the clinical scenario, effusion size, and hemodynamic instability. This procedure is concurrently diagnostic and therapeutic. Although systematic evaluation of pleural and peritoneal fluid cytology is abundant in the literature, large series focusing on pericardial fluid (PF) cytology are sparse. This study aims to analyze a large cohort of PF specimens from a single institution, to determine the etiology of PF, the diagnostic utility of cytology, and correlation with the histological and microbiology results.
Materials and Methods: The PF specimens collected between January 2005 and December 2010 were retrieved. Clinical history, laboratory and radiological results, cytological and all pertinent histological diagnoses were recorded. The PF was collected through ultrasound or fluoroscopic-guided PC or via the pericardial window. The PF was sent for chemistry, microbiological, and cytological evaluation. The specimens were received fresh from Cytology. For each specimen one Diff-Quik® and three Papanicolaou stained cytospin slides were prepared and if more than 10 ml of PF was received a cell block was performed.
Results: One hundred twenty-eight PF specimens were obtained from 56 males and 57 females with age ranging from 6 to 85 years (mean 52.5 years). During the study period 1292 pleural and 1396 peritoneal fluid specimens were processed (4.54% incidence of PF specimens). The amount of fluid received ranged from 1 to 1,150 ml (mean 60.5 ml). Table 1 summarizes the cytological diagnoses of all PF cases. Thirty-one cases (24.22%) were malignant. With regard to males, the most common malignancy was lung carcinoma (75%) followed by digestive system carcinomas (25%), while for females the most common malignancy was lung carcinoma (52.17%) followed by breast carcinoma (39.13%), [Table 2]. The underlying etiology of negative PF specimens was broad [Table 3]. The two cases diagnosed as suspicious for malignancy had few atypical cells present in the PF and no ancillary studies were performed. Pericardial biopsy was performed in 32 cases. In 25 (78.1%) the cytological diagnosis correlated with the histological one. Cytology failed to diagnose lymphoma (two cases) and metastatic sarcoma (one case) (9.4% false negative rate), whereas, biopsy failed to sample four carcinomas (12.5%), diagnosed by cytology and confirmed by clinicoradiological findings. Ten PFs were culture-positive for bacteria; one case lacked marked acute inflammation on cytology (confirmed on biopsy), and the culture-positive result was interpreted as contamination (clinical impression favored minoxidil-associated pericardial effusion).
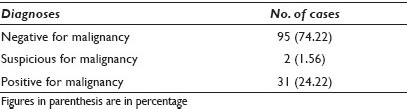
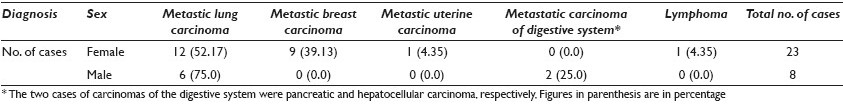
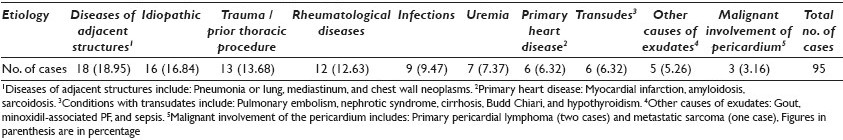
Conclusions: PF specimens are uncommon and the vast majority of them are the result of a benign process (74.22%). The most common metastatic malignancy is lung carcinoma in both males (75.0%) and females (52.17%), followed by digestive system carcinomas in males (25.0%) and breast carcinoma in females (39.13%). The cytological / histological correlation is excellent (78.1%) and the cytological evaluation is superior to biopsy in identifying carcinomas, as biopsy carries a sampling error. The cytological diagnosis correlates 100% with the microbiology cultures in infectious cases.
17: Pediatric effusion cytology: Ten-year retrospective analysis at a children's hospital
Minoti Magotra, MBBS, MS, Nariman Gobara, MBChB, MS, Morris Edelman, MD, Nora Morgenstern, MD
Department of Pathology and Laboratory Medicine, North Shore Long Island Jewish Health System, New York, New York
Introduction: Background: Information on pediatric effusion cytology is limited. Some studies have shown that the pleura are the most common site of pediatric serosal effusions, primarily due to infectious etiologies. However, these studies have not focused on the cytopathology.
Materials and Methods: We report data of pediatric serosal effusions submitted for cytology from 2000 to 2010. One hundred and ten serosal effusions were categorized based on anatomical location, cytology, and age group (A: 0 to < 1 year, B: 1 to < 5 years, C: 5 to < 12 years, and D: 12 to < 20 years).
Results: Pleural effusions constituted 49% of the cases, ascites 33%, and pericardial effusions 18%. A majority of the effusions belonged to group D (48% pleura, 61% ascites, and 60% pericardial) followed by group C. Males had 55% pleural effusions and 21% were malignant. Pleural malignancies included neuroblastoma in groups A and C, Wilms’ tumor in group B, lymphoproliferative disorders in groups C and D, and rhabdomyosarcoma in group D. For ascites, 72% were female, 8% were malignant (ALL, dysgerminoma, and Ewing's sarcoma), 39% had an associated malignant condition (one neuroblastoma, five lymphoproliferative, two CNS tumors, six ovarian, and one pancreatic cancer), and 14% had benign ovarian tumor. Sixty percent of the pericardial effusions occurred in males, 10% were malignant (all lymphoproliferative) and 10% were benign.
Conclusions: Among pediatric serosal effusions, pleural effusion was the most common and the most likely to be malignant. Teenagers had the highest prevalence of all effusions (54%). However, children in groups C and D had the highest prevalence of malignant effusions (27%), mostly lymphoproliferative disorders. The majority of malignant effusions in groups A and B were pleural, associated with neuroblastoma and Wilms’ tumor. Ascites occurred mostly in females, typically due to ovarian tumors.
18: Cytomorphological and immunohistochemical assessment of metastatic breast carcinoma with apocrine features in fluid cytology
Sara Monaco, MD, Walid Khalbuss, MD, PhD, Payam Arya, MD, Liron Pantanowitz, MD
Pathology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Introduction: Breast carcinoma is one of the most common metastases identified in fluid cytology. Immunocytochemical evaluation in these cases is often necessary and involves a panel of immunostains for mesothelial cells and adenocarcinoma. However, interpretation of immunostain results can sometimes be very difficult, particularly with apocrine breast carcinomas, where calretinin expression has been described in about 25% of these cases. The aim of this study is to report our experience with metastatic breast carcinomas showing apocrine features in fluid cytology specimens.
Materials and Methods: A retrospective search was conducted for surgical biopsies and excisions of primary breast carcinomas with apocrine features in our computer database. We then reviewed these cases to find any corresponding fluid cytology specimens. The fluid cytology cases were then evaluated for patient demographics and clinical features, cytomorphology, and available immunostain results. The cytospins, ThinPrep® slides, and cell block sections with immunostains were then reviewed in each case.
Results: A total of 20 fluid cytology cases were identified in 10 patients (mean age, 64.6 years; age range, 50 – 86 years) with a history of a primary breast carcinoma with apocrine features. Of these 20 cases, five were positive, two suspicious, four atypical, and nine negative for malignant cells. On retrospective slide review, 12 cases (60%) were positive for metastatic adenocarcinoma (six peritoneal fluids, six pleural fluids), including the five cases initially called positive, two called suspicious, three of the atypical cases, and two cases previously diagnosed as negative. The primary breast carcinomas in these cases included six cases of classical lobular carcinoma, four cases of ductal carcinoma with apocrine features, and two cases of pleomorphic lobular carcinoma. Cytomorphology revealed a predominance of single cells in a mesothelial-like pattern in eight cases (67%), and small clusters in four cases (33%). The tumor cells had moderate-to-abundant homogeneous cytoplasm and prominent nucleoli in all cases. The immunostain results were available in eight cases (78%). ER and mammaglobin immunoreactivity confirmed the presence of metastatic adenocarcinoma of breast origin in six out of eight cases (75%). Five cases (63%) showed positivity for calretinin in the tumor cells, but WT-1 was negative in the tumor cells. Four cases were negative for BerEP4 (50%).
Conclusions: Our results demonstrate that the cytomorphological and immunohistochemical evaluation of metastatic breast carcinomas with apocrine features can be challenging. These tumor cells often mimic benign or reactive mesothelial cells in fluid cytology, leading to non-definitive (atypical or suspicious) or negative diagnoses in some cases, and repeat sampling. In addition, these carcinomas may show unusual positivity for calretinin, and negativity for BerEP4, which can make their assessment even more difficult. Nonspecific cytoplasmic staining with calretinin may be due to the apocrine granules present in these tumor cells. Thus, nuclear stains like WT-1 (for mesothelial cells) and ER (for breast carcinoma) are more likely to be helpful in these difficult cases.
19: Pleural effusion in women with a known adenocarcinoma: The role of immunostains in uncovering another hidden primary
Haitham Nasser, MD, Tomi Kuntzman, DO
Cytology, William Beaumont Hospital, Royal Oak, Michigan
Introduction: Pleural fluid metastasis is often secondary to a known primary. We aim to identify the percentage of adenocarcinomas metastatic to pleural fluid and the frequency of a second primary being the origin of the effusion in women; and also assess the role of immunostains in uncovering the second primary.
Materials and Methods: We reviewed 131 cases of metastatic adenocarcinoma to pleural fluid from the archives of William Beaumont Hospital between June 2007 and November 2010.
Results: A total of 123 cases (94%) had a well-documented primary. In this group, the breast was the most common primary site (34%). Less common were lung (30%) and ovary (20%). Ten cases (7.9%) had two primaries. Seven cases, detected with the aid of immunostains at the time of effusion, proved to be secondary to an adenocarcinoma other than the one identified in the patients’ records. Lung would have been the most commonly overlooked tumor (5 / 7 cases). Eight cases (6%) remained of inconclusive origin due to an occult primary, lack of cells on cell blocks, discordance with radiology or cytology of a known primary. Morphology, in association with a small panel of immunostains, including TTF1, Estrogen Receptor, Mammaglobin, WT1, CA125, and CDX2, proved helpful in identifying the primary origin in 94% of the cases.
Conclusions: Due to the major implications of the therapeutic strategy, even in the presence of a known primary, a small panel of immunostains is recommended on the available cell block material, to verify the origin of the effusion. Otherwise, a comparison with the previous available material is highly recommended to avoid overlooking another primary.
20: Cytomorphological features of metastatic sarcomas in effusions
Julieanna Constantine, BSc, Walid Khalbuss, MD, PhD, Sara Monaco, MD, Liron Pantanowitz, MD
Pathology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Introduction: Metastatic sarcomas are an infrequent finding in the practice of effusion cytology. Making a diagnosis of sarcoma in fluid cytology can be challenging and often requires knowledge of a known primary tumor and / or use of ancillary studies. Moreover, a variety of different sarcomas can manifest with a malignant effusion. The morphology of sarcomas in effusion preparations may differ from those of the original sarcoma and may also mimic other poorly differentiated neoplasms. The aim of this study was to evaluate the cytomorphology of sarcomas in effusions and to determine the useful characteristic features for their recognition.
Materials and Methods: A nine-year retrospective review of cytology cases was performed, which included effusions with a final cytological diagnosis of metastatic sarcoma. Data regarding patient information (age, gender), effusions (body cavity involved), and sarcoma findings (primary site, presentation in months to effusion, and ancillary studies such as immunocytochemistry and FISH) were recorded. The cytology samples included direct smears, cytospins, ThinPrep® slides, and cell blocks. The following cytomorphological features were evaluated: Cellularity, cell arrangement, cell size and shape, cytoplasm quality and quantity, nuclear detail (nuclear: cytoplasmic ratio, chromatin, nucleoli), and background.
Results: A total of 27 malignant effusions (15 pleural, 56%; 12 peritoneal, 44%) due to metastatic sarcoma were identified. In three cases (11%), effusion was the initial presentation, and in 24 (89%), sarcomas were diagnosed, on an average, 11 months (range, 1 – 48) prior to obtaining the fluid specimen. A wide variety of sarcomas were diagnosed including Ewing sarcoma (four), MMMT (four), epithelioid sarcoma (four), osteosarcoma (three), clear cell sarcoma (three), leiomyosarcoma (three), rhabdomyosarcoma (two), pleomorphic sarcoma / MFH (one), chondrosarcoma (one), liposarcoma (one), and high-grade sarcoma NOS (one). The specimens were of variable cellularity. The cytological features shared by these sarcomas in effusions included single cell arrangement (93%), multinucleation (52%), nuclear pleomorphism (37%), indistinct cell borders (225), and a bloody proteinaceous background (63%). Loose clusters were infrequent (26%), including one Ewing sarcoma with rosettes. In almost all cases, the tumor cells were round, and rarely spindle-shaped (one osteosarcoma, one MFH) or bizarre (one rhabdomyosarcoma, one high-grade sarcoma NOS) in appearance. The matrix material was identified in the chondrosarcoma case, with a tigroid background in the case of metastatic clear cell sarcoma.
Conclusions: This series indicates that a wide variety of sarcomas may be diagnosed in effusion specimens. Although their cytomorphological findings are diagnostic of malignancy, very few specific characteristics appear to be unique to these metastatic sarcomas in effusions. Further sub-classification of these malignant effusions relies largely on a comparison of metastatic tumor cells with the primary sarcoma and / or ancillary testing.
21: Peritoneal washing cytology in patients with ovarian serous tumors of low malignant potential
John Thomison, III, MD, Anais Malpica, MD, Nour Sneige, MD
1Division of Pathology and Laboratory Medicine, The University of Texas MD Anderson Cancer Center, Houston, Texas
Introduction: At presentation, up to 30% of patients with ovarian serous tumors of low malignant potential (OvSeLMP) demonstrate extra-ovarian disease, further categorized as non-invasive or invasive implants. Patients with implants are at a higher risk of developing recurrences than patients with OvSeLMPs only. Although peritoneal washing cytology (PW) is generally recommended as part of the staging workup of OvSeLMP, to date, no study has evaluated the role of PWs in predicting the presence of peritoneal implants and their correlation with invasive versus non-invasive status.
Materials and Methods: A total of 110 patients diagnosed with OvSeLMP, ages 21 to 89 years, with 155 corresponding PWs, met the inclusion criteria, based on the medical record review. Surgical diagnoses were divided into four categories: OvSeLMP (72 patients), OvSeLMP with microinvasion or micropapillary features (30 patients), and focal low-grade serous carcinoma arising from OvSeLMP (LGSC / LMP) (eight patients). Staging biopsies were diagnosed as negative, endosalpingiosis, non-invasive implant, invasive implant, or low-grade serous carcinoma (LGSC). The corresponding PWs were reviewed and categorized as negative, endosalpingiosis or serous neoplasm, using the previously published criteria. These results were correlated with the histological diagnosis and statistical analysis was done using the Fischer's exact test.
Results: Staging biopsies showed peritoneal disease in 35 patients (32%) (18 non-invasive implants, 12 invasive, and five LGSC) and endosalpingiosis in 22 patients (20%). Sixty-nine percent of the patients with peritoneal disease demonstrated PWs with serous neoplasm (P < 0.0001). However, there were no definitive cytological features separating invasive or LGSC from non-invasive implants. PWs were positive for serous neoplasm in 11 of the 75 patients (15%), without the corresponding histological tumor implants (results summarized in Table 1. Of these, two patients had recurrent disease within one year (one with OvSeLMP and one with LGSC / LMP). A total of 11 patients had recurrent disease, with 10 having either microinvasion or LGSC / LMP in the primary tumor, or invasion or LGSC in the peritoneal implants, and eight were with PWs showing serous neoplasm (median time to recurrence, three years). Of the 110 patients, 93 were alive at the time of data collection, with nine lost to follow-up, five deceased from other causes, and only three dead from their disease, each with LGSC / LMP (median follow-up, four years; mean, 4.9 years).
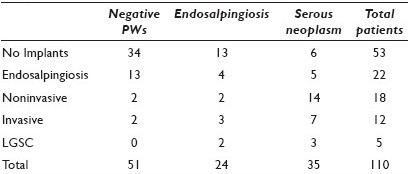
Conclusions: PW is a sensitive indicator for the presence of peritoneal implants and may detect a subset of patients with subclinical peritoneal involvement in the staging of OvSeLMP. The distinction between invasive and non-invasive implants requires tissue sections, and the role of PW is limited in this distinction. However, in a small percentage of patients without histological implants, a positive PW may be useful in predicting disease recurrence.
22: Rapid evaluation of Diff-Quik® stained corneal scrapings for acanthamoeba cysts
Cora Uram-Tuculescu, MD1, Charlie Thompson, MD2, Joseph Iuorno, MD2, Ema Dragoescu, MD1
1Pathology, Virginia Commonwealth University Health System, Richmond, Virginia; 2Opthalmology, Virginia Commonwealth University Health System, Richmond, Virginia
Introduction: Acanthamoeba is a ubiquitous protozoan found in soil and freshwater. Acanthamoeba keratitis (AK) is an intractable, sight-threatening infection of the cornea. In the United States (US), 85% of the AK cases occur in contact lens wearers, usually as a result of exposure to contaminated water. In the US, the incidence of AK is estimated to be one-to-two cases / million contact lens users. Currently, there is no approved drug for the treatment of AK in the US. An early diagnosis and appropriate management of AK are critical for ensuring the best visual outcome. Clinically, AK should be suspected in all cases of corneal trauma complicated by exposure to soil or contaminated water and in all contact lens wearers. Tests used to confirm the diagnosis are corneal biopsy and culture (which require at least few days of processing until the final result is reported) or in vivo tandem scanning confocal microscopy (which is an expensive technology, available only in select centers). The aim of this study is to report our experience with rapid evaluation of Diff-Quik® stained corneal scrapings in suspected AK cases. Diff-Quik® stain, a modified Wright Giemsa stain, has the advantage of reducing the staining time to 15 seconds and offers better visualization of cytoplasmic details and extracellular materials, including microorganisms.
Materials and Methods: Corneal scrapings collected between January 2005 and April 2011 were retrieved. Demographic data, results of corneal biopsy and culture and calcofluor white stain, if available, were recorded. The cornea was gently scraped with the blunt side of a scalpel blade and the material was smeared on a glass slide, air dried, Diff-Quik® stained, and rapidly evaluated. If enough material was obtained, a second slide was stained for calcofluor white (a fluorochrome stain used to detect fungi and parasites in microbiology).
Results: Fourteen corneal scrapings from 12 females (85.71%) and two males (14.29%) with age ranging from 18 to 78 years (mean 39) were retrieved. Seven cases (50%) had a concomitant calcofluor white stained slide. In 11 cases (78.57%), the material was sent for microbiology culture and in three cases (21.42%), corneal biopsy was performed. One corneal scraping was positive for Acanthamoeba cysts on Diff-Quik®, with the result subsequently confirmed with a positive calcofluor white stain and corneal biopsy. The cysts were extracellular, large-sized and double-walled [Figure 1]. The background showed reactive corneal epithelial cells and acute inflammation. Another case was negative on corneal scraping and culture, however, the clinical suspicion for AK persisted and the confocal microscopy confirmed the diagnosis, followed by positive corneal biopsy one month later. The corneal scraping slide was re-reviewed and no cysts were seen. Their absence was attributed to the deep penetration of corneal stroma by the cysts and the superficial nature of the scraping. The other 12 cases were negative on Diff-Quik®, confirmed by their clinical evolution. Fungal hyphae were identified in one case, and in six cases, various bacterial organisms were identified on cultures.
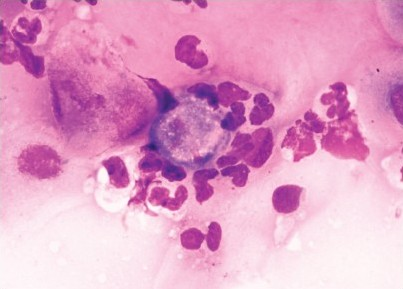
- High-magnification of extracellular Acanthamoeba cyst identified in corneal scraping. Note the large size of the cyst with a double wall and a somewhat polygonal shape (Diff-Quik® stain)
Conclusions: Acanthamoeba cysts can be identified in Diff-Quik® stained corneal scrapings. This has not previously been reported in literature. The cysts are extracellular, large, and double-walled. A rapid positive result of AK helps in immediate treatment and a better visual outcome. In the case of a negative result, if clinical suspicion for AK persists, further tests are needed.
23: PAX2 and PAX8: Efficacious markers for evaluating effusions from metastatic tumors
Lindsay Waters, MD, Donna Coffey, MD, Luan Truong, MD, Dina Mody, MD
Pathology, The Methodist Hospital, Houston, Texas
Introduction: PAX2 and PAX8 are transcription factors of the paired box gene (PAX) family that serve as important developmental regulators. Prior studies of surgical specimens demonstrate that PAX2 plays an important role in renal and female genital tract maturation; similarly, PAX8 is understood to influence thyroid, renal, and female genital tract development. Knowledge of PAX2 and PAX8 immunohistochemical staining can be applied to reach diagnoses in challenging metastatic malignant effusions. Distinguishing Mullerian and non-Mullerian carcinoma may be difficult; therefore, these adjunct diagnostic markers for tumors of Mullerian origin are valuable. Additionally, identifying renal cell carcinoma (RCC) in effusion cytology, albeit uncommon, is essential. PAX2 and PAX8 immunohistochemical staining has not been extensively studied in cytology specimens, specifically pleural and peritoneal effusions from both renal cell and Mullerian carcinomas.
Materials and Methods: We evaluated PAX2 and PAX8 expression in gynecological carcinoma, non-gynecological carcinoma, and renal cell carcinoma effusion specimens. These specimens had prior panels of immunohistochemical staining, that is, CA-125, WT1, CK7, CK20, ER, PR, TTF-1, and CDX2, performed to correctly identify the primary tumor. Sections from cell blocks of 89 pleural and peritoneal effusions were selected from 2003 to 2011 at The Methodist Hospital (18 controls, 10 renal cell carcinomas, 21 Mullerian carcinomas, and 40 non-Mullerian carcinomas). PAX2 and PAX8 immunohistochemical staining was performed. The stained slides were blindly reviewed, and immunohistochemical positivity was defined as at least 25% strong nuclear staining of tumor cells.
Results: PAX2 stained 0 / 18 (0%) control cases, 9 / 9 (100%) RCC cases, 7 / 20 (35%) Mullerian carcinoma cases, and 1 / 40 non-Mullerian carcinoma cases (2%). PAX8 stained 1 / 18 (5%) control cases, 10 / 10 (100%) RCC cases, 20 / 20 (100%) Mullerian carcinoma cases, and 1 / 40 non-Mullerian carcinomas (2%). PAX2 is 35% sensitive to Mullerian carcinomas and 100% sensitive to renal cell carcinomas. PAX2 is 98% specific to Mullerian carcinomas and renal cell carcinomas. PAX8 is 100% sensitive to Mullerian and renal cell carcinomas. PAX8 is 98% specific to Mullerian and renal cell carcinomas. One pleural effusion from a metastatic breast carcinoma showed weak PAX2 staining, and a second pleural effusion from a metastatic breast carcinoma showed PAX8 staining.
Conclusions: Cell blocks from metastatic malignant effusions are often limited due to low tumor cellularity. Therefore, arriving at an accurate diagnosis and identification of the primary tumor requires a small panel of highly sensitive and highly specific immunohistochemical stains. In pleural and peritoneal effusions from metastatic Mullerian and renal cell carcinomas, PAX2 and PAX8 are expressed. We observed that PAX8 stains more tumor cells with high nuclear intensity. PAX2 stains tumor cells less strongly, thus it is often challenging to interpret. PAX8 is more sensitive to metastatic effusions from Mullerian carcinomas, and it appears superior to PAX2 for this purpose. We recommend adding Pax8 in a panel of immunohistochemical stains when the differential diagnosis includes tumors of Mullerian origin.








