Translate this page into:
Abstracts for the 59th Annual Scientific Meeting (November 2011) by American Society of Cytopathology (ASC) at Baltimore, MD, USA
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
These are peer-reviewed poster-platform submissions finalized by the Scientific Program Committee. A total of 153 abstracts (14 Platforms [PP1 through PP14] & 139 Posters [1 through 139]) were selected from 161 submissions to be considered for presentation during November 4 – 8, 2011, at the Hilton Baltimore Hotel, to pathologists, cytopathologists, cytotechnologists, residents, fellows, students, and other members of cytopathology-related medical and scientific fields.
Keywords
Abstracts
American society of cytopathology
ASC
cytopathology
cytology
69: Cytology follow-up analysis of the bethesda system — Thyroid diagnostic category follicular lesions of undetermined significance (category III) in African Americans versus non-African Americans
Pamela Archuletta, MD, Raja Gidwani, MD, Opada Alzohaili, MD, Julie Samantray, MD, Jineng Feng, MD, Donping Shi, MD, Lili Geng, MD, Paul Tranchida, MD, Mujtaba Husain, MD, Vinod Shidham, MD, Tamar Giorgadze, MD
Cytopathology, Wayne State University, Detroit, Michigan
Introduction: It has been reported that African Americans (AA) have a higher prevalence of malignancy compared to Non-African Americans (NAA); however, a report by Morris et al. indicates that the rate of thyroid malignancies in AA is half that of NAA. The reports looking at thyroid lesions in AA compared to NAA are few and have conflicting results. Even less is known about the rates of follicular lesions of undetermined significance (FLUS) between these two populations. There are no reports looking at FLUS in this population. The aim of this study is to analyze FLUS in the AA population.
Materials and Methods: We retrospectively reviewed thyroid FNA cytology reports and corresponding surgical pathology reports between January 2005 and January 2011, in cases where the race was known. Two hundred fifty eight patients met our inclusion criteria and were associated with 311 FNA specimens, and 265 surgical pathology specimens. The patients were categorized as AA and NAA. The NAA group included Caucasians (C), Hispanics (H), and Others (O). The rate of FLUS was determined from the total number of thyroid FNAs. Cases predating the latest edition of the bethesda system for reporting thyroid cytology were categorized as FLUS based on microscopic descriptions that paralleled those outlined in the bethesda system for reporting thyroid cytology. All post FLUS diagnostic FNA results were compiled and analyzed. The follow-up surgical pathology diagnosis was used for the final categorization.
Results: Of the 258 patients, 65 were categorized as FLUS and included 36 AA and 27 NAA. The average age for AA was 51 (range 20 – 88) and for NAA was 53 (range 25 – 86) years. The average age of AA diagnosed with FLUS was 48.5 (range 18-80) and NAA was 47.5 (range 24 – 77) years. Similar to the overall population, there were more females than males in both groups. There were more females in the AA versus NAA (85 and 75%, respectively). With respect to the FLUS lesions, there were more females than males (89% for AA and 81% for NAA). The rate of FLUS was similar for AA and NAA (20% and 20.5%, respectively). After a FLUS diagnosis, most patients were followed up with surgical resection as apposed to repeat FNA (91% of AA and 96% of NAA). The time from initial FLUS diagnosis to surgical resection for AA and NAA was six (range 1 – 48.75) months and 2.3 (range 0.25 – 9.57) months, respectively. Three AA (9%) had repeat FNAs averaging 11 (range 1 – 29.75) months after initial FLUS diagnosis, whereas, only one NAA had a repeat FNA 3.75 months after the initial FLUS diagnosis [Table 1]. With respect to the surgical outcomes of FLUS, the rates of malignancy for AA versus NAA were 38% and 56%, respectively. The incidence of papillary thyroid cancer was less in AA versus NAA [Tables 2 and 3].
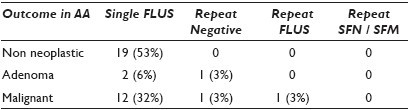
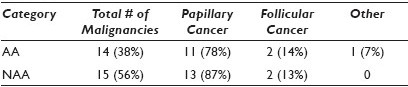

Conclusions: Both groups were more likely to proceed directly to surgical intervention after initial diagnosis of FLUS; however, the time interval between the initial FLUS diagnosis was longer in AA suggesting a delay in surgical intervention compared to NAA. Reasons for this were not elucidated in this study, however, a possible etiology could be a delay in follow-up. Not enough data is present to make any conclusion about the utility of repeat FNA in FLUS lesions in AA versus NAA. AA were less likely to be diagnosed with malignancy than NAA following a FLUS diagnosis. This is an area that warrants further investigation with respect to possible environmental or intrinsic causes.
70: Insights into false-negative fine needle aspiration of the thyroid: A single institution experience
Brent Bedke, MD, Jordan Reynolds, MD, Jesse Voss, CT(ASCP), Ashley Hansen, CT(ASCP), Brittany Rosas, CT(ASCP), Aziza Nassar, MD, Michael Henry, MD
Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, Minnesota
Introduction: Fine needle aspiration (FNA) of the thyroid is an integral step in the evaluation of thyroid nodules. Despite high sensitivity even with ultrasound-guided FNA (US FNA), false negatives (FN) occur leading to delayed treatment. We performed a retrospective review of negative thyroid FNAs from 2001 to 2008, which had a follow-up histological diagnosis of carcinoma. In the present study we compare the cytomorphological characteristics of these FNAs with the histological features of the corresponding thyroid resections.
Materials and Methods: All thyroid FNAs with a negative diagnosis from 2001 to 2008 were identified from the computerized data. Cytologica; specimens signed out as ‘non-diagnostic, too few follicular cells’ were excluded. Available follow-up tissue resection specimens for each case were reviewed to identify FN FNA. Any carcinoma identified in the same thyroid lobe previously aspirated was included. Review of the archived cytology slides was performed by two cytotechnologists, two trainees and one cytopathologist, with a review of histology by the same two trainees and cytopathologist. The FN FNA slides were evaluated for group cellularity, presence of micro / macro follicles, colloid quantity, nuclear hyperchromasia, nuclear groove percentage, intranuclear inclusion quantity, and quantity of lymphocytes. Histology parameters included tumor size, location, and presence of biopsy site change / needle tract within the tumor.
Results: From 2001 to 2008, 11,461 thyroid FNAs were identified, 7225 (63%) were negative of which 37 (0.5%) had histological confirmation of carcinoma. Ten cases could not be retrieved and 27 potential FN cases were obtained, 21 had a histological diagnosis of papillary thyroid carcinoma (PTC), three had a follicular variant of PTC, two had follicular carcinoma, and one had Hurthle cell carcinoma. Median time lapse from FNA to surgical resection was two months (range 0 – 26 months) with median tumor size 0.75 cm (range 0.2 – 9.0 cm). The cytological findings are presented in Table 1.

Conclusions: Overall, the sampling error was attributed to a majority of cases. False negative thyroid FNAs were associated with minimal lymphocytes, low percentage of grooves, and rare nuclear inclusions. Subgroup analysis revealed a larger number of grooves and intranuclear inclusions in cases with biopsy site change, within the tumor. Attention to detail in the cytological evaluation of these features remains crucial to prevent false negative diagnosis.
71: Cytohistological correlation of parotid lesions
Feriyl Bhaijee, MD, Israh Akhtar, MD, Mithra Baliga, MD, Rhyne Flowers, MD, Anwer Siddiqi, MD
Pathology, University of Mississippi Medical Center, Jackson, Mississippi
Introduction: Fine needle aspiration (FNA) is often used as a diagnostic modality in the evaluation of palpable parotid lesions. This study correlates the FNA cytology results with the subsequent histopathological final diagnoses.
Materials and Methods: All parotid FNAs performed at a large academic medical center between 2006 and 2010 were reviewed, and patients that underwent a subsequent surgical resection were identified. We obtained the following data for patients: Age, sex, FNA cytology results, and surgical histopathology results.
Results: Over a four-year period, 74 patients underwent a parotid FNA and subsequent surgical resection. Of these, 34 patients had a pleomorphic adenoma, 94% (32 / 34) of which showed cytohistological correlation; 14 had Warthin's tumor, with 79% (11 / 14) correlation; five had squamous cell carcinoma, with 100% correlation; three had mucoepidermoid carcinoma, with 33% (1 / 3) correlation; two had salivary duct carcinoma, with 50% correlation; one had poorly-differentiated adenocarcinoma, without correlation; and the following diagnoses had 100% cytohistological correlation: One adenoid cystic carcinoma, one epithelial-myoepithelial carcinoma, one oncocytoma, one basal cell adenoma, one papillary adenocarcinoma, one medullary carcinoma, three diffuse large B-cell lymphomas, three melanomas, one branchial cleft cyst, one benign lymphoepithelial cyst, and one salivary duct cyst. Overall, the FNA cytology results and histopathology results correlated in 88% (65 / 74) of the patients. Of the nine cases in which there was disparity between FNA cytology results and subsequent histopathology results: one pleomorphic adenoma was preceded by a non-diagnostic (inadequate) smear; one pleomorphic adenoma was called a duct obstruction / retention cyst on FNA; one Warthin's tumor was suggestive of SCC on FNA, another was ‘suspicious for malignancy,’ and a third was called sialadenitis; one salivary duct carcinoma with squamous differentiation was suggestive of a squamous cell carcinoma on FNA; two mucoepidermoid carcinomas were preceded by benign or non-diagnostic smears; and one poorly-differentiated adenocarcinoma was preceded by a diagnosis of pleomorphic adenoma on FNA.
Conclusions: For parotid lesions, FNA cytology results showed excellent correlation with the subsequent histopathology results. In our setting, a cytological; diagnosis of pleomorphic adenoma, Warthin's tumor, or squamous cell carcinoma was highly predictive of the subsequent histopathological final diagnosis.
72: Combined cytomorphological and immunophenotypic analysis enhances the fine needle aspiration diagnosis of lymphoproliferative disorders involving the thyroid
Gillian Levy, Alexander Finkelstein, Guoping Cai
Pathology, Yale University School of Medicine, New Haven, Connecticut
Introduction: Fine needle aspiration (FNA) is the choice of diagnostic tool for thyroid lesions. Although cytomorphological analysis alone is sufficient for rendering a diagnosis in most circumstances, the addition of ancillary studies may sometimes become necessary. For example, a variety of lymphoproliferative disorders (LPDs) may have overlapping cytomorphological features with that of Hashimoto / lymphocytic thyroiditis, which is quite a common entity in the thyroid. LPDs seen in the thyroid may represent thyroidal involvement of systemic disease and rarely occur as primary neoplasms. Clinicopathological features that prompt further workups include patient's prior history of LPD, presence of monomorphic lymphocytes, or pleomorphic lymphocytes with increased large cell population and frequent mitoses / apoptotic bodies. In this retrospective study, we aimed to review our experience with the FNA diagnosis of LPDs involving the thyroid.
Materials and Methods: The database of the Department of Pathology was searched for all cases of thyroid FNA with lymphoproliferative disorders in the diagnostic field during the period from January 2008 to March 2011. A total of 16 cases were retrieved, with cytological diagnoses ranging from favor reactive, atypical lymphocytes, suspicious for lymphoma, to malignant lymphoma. Flow cytometric studies were performed in eight cases using the panel of CD20, CD3, CD4, CD8, CD5, CD10, CD23, kappa, and lambda. Follow-ups or prior specimens were available for comparison in eight cases.
Results: The patients included 14 females and two males with ages ranging from 29 to 90 years (mean 53 years). The biopsied lesions involved the right (7 cases), left (4 cases), isthmus (3 cases), and both right and left (2 cases) thyroid. Three patients had a prior history of LPDs including chronic lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and diffuse large B-cell lymphoma (DLBCL). Of the eight cases that had flow cytometry, DLBCL was diagnosed in four cases with another case being MCL. Interestingly, the patient who had a prior history of CLL developed DLBCL in the thyroid. The remaining three cases were considered to be Hashimoto / lymphocytic thyroiditis because of negative flow cytometric results. A reactive process was favored in seven out of eight of the cases without flow cytometry. No follow-up was available for the case that was cytologically suspicious for lymphoma.
Conclusions: Involvement of the thyroid by LPDs is a rare occurrence with DLBCL being the most common type. Patient's prior history and recognition of atypical cytomorphological features must help prompt further workups. Flow cytometry is the choice of ancillary study that helps render a definite diagnosis. In selective cases, addition of fluorescence in-situ hybridization for chromosomal translocations may be helpful in further subtyping LPDs.
73: Reliability of benign non-neoplastic findings on fine needle aspiration of the parotid gland
Richard Cantley, MD1, Leonidas Arvanitis, MD1, Guy Petruzzelli, MD, PhD2, Vijaya Reddy, MD1, Paolo Gattuso, MD1
1Pathology, Rush University Medical Center, Chicago, Illinois; 2Otolaryngology, Rush University Medical Center, Chicago, Illinois
Introduction: There is considerable debate over the role of fine needle aspiration (FNA) in the evaluation of parotid gland lesions. Benign findings on FNA can obviate the need for surgical resection. However, the sensitivity of FNA in diagnosing malignant neoplasms of the parotid gland remains an area of controversy. This study aims to assess the accuracy of a benign, non-neoplastic diagnosis on FNA of the parotid gland.
Materials and Methods: A retrospective search of the cytology archives from our institution for a time period of 19 years (January 1991 to January 2010) revealed that a total of 381 patients underwent parotid FNAs. Of these, 211 had benign and non-neoplastic findings, 90 had benign neoplastic findings, 43 had primary malignant findings, three had secondary malignant findings, and 34 (8.9%) had insufficient material for diagnosis. Among the 211 non-neoplastic cases, 37 (17.5%) underwent surgical resection.
Results: Among the patients with surgical follow-up, there were 13 males and 24 females (M : F 0.54 : 1) ranging in age from 32 to 85 years (mean age 58 years). On surgical resection, 33 (89%) had benign findings. Sixteen (43%) had confirmed non-neoplastic pathology. Seventeen (46%) had benign neoplastic pathology, including twelve Warthin's tumors, three pleomorphic adenomas, one lipoma, and one basal cell adenoma. Four patients (11%) had malignant findings on surgical follow-up. Three had a diagnosis of B cell lymphoma, and one had a diagnosis of squamous cell carcinoma. Among the three lymphoma cases, two had a previous diagnosis of lymphoma. The third patient was being worked up for lymphoma and leukemia, including concurrent bone marrow biopsy, based on a strong clinical and laboratory suspicion. The patient with a diagnosis of squamous cell carcinoma had radiological evidence of bony metastasis to the mandible, prompting surgical follow-up, despite benign FNA findings. In 33 of the 37 cases (89%) with non-neoplastic findings on FNA and subsequent surgical follow-up, resection confirmed the benign FNA findings, although 17 patients (46%) showed benign neoplastic lesions. Warthin's tumor was the most common neoplasm misdiagnosed as non-neoplastic on FNA (12 cases). In the absence of a strong clinical suspicion for malignancy, a finding of non-neoplastic pathology on FNA was a reliable indicator of benignity [Tables 1 and 2].
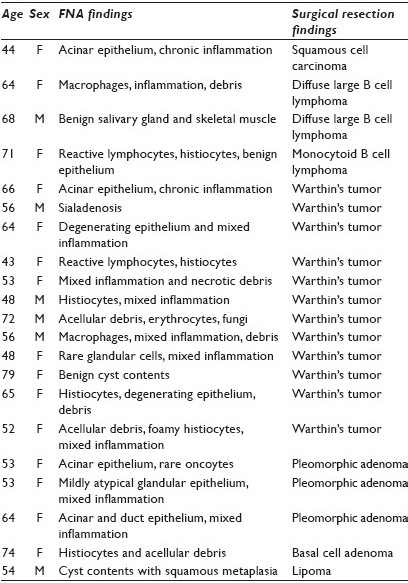
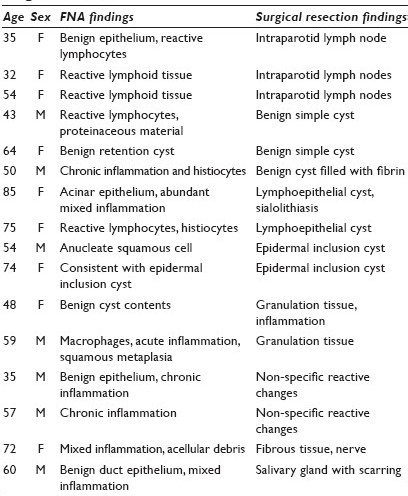
Conclusions: These data suggest that non-neoplastic findings on FNA of the parotid gland could obviate the need for surgical resection when clinical suspicion for malignancy was low, as only four (11%) patients had a diagnosis of malignancy on surgical resection, and all four of these patients had a strong clinical or radiographic evidence of malignancy at the time of FNA.
74: Thyroid fine needle aspiration cytology: Performance data of malignant and neoplastic cases as identified from the ASCP NonGYN assessment program
Stan Eilers, MD, FASCP1, Paula LaPolice, BS, CT(ASCP)2, Perkins Mukunyadzi, MD, FASCP3, Umesh Kapur, MD, FASCP4, Amy Wendel Spiczka, MS, SCT, MB, HTL(ASCP)CM5, Ajay Shah, MD, FASCP6, Husain Saleh, MBA, MD, FASCP7, Adebowale Adeniran, MD, FASCP8, Amberly Nunez, MD9, Indra Balachandran, PhD, SCT(ASCP), CFIAC10, Jennifer Clark, BS, SCT(ASCP)CM11, Larry Lemon, BS, CT(ASCP)11
1Pathology, Mercy Medical Center, Cedar Rapids, Iowa; 2Pathology, Baystate Medical Center, Springfield, Massachusetts; 3Pathology, Arkansas Pathology Associates, Little Rock, Arkansas; 4Pathology, Loyola University Medical Center, Maywood, Illinois; 5Pathology, Mayo Clinic, Scottsdale, Arizona; 6Pathology, FNA Clinic, Toledo, Ohio; 7Pathology, Detroit Medical Center, Detroit, Michigan; 8Pathology, Yale University School of Medicine, New Haven, Connecticut; 9Pathology, University of Alabama at Birmingham Health System, Birmingham, Alabama; 10School of Cytotechnology, Albany College of Pharmacy and Health Sciences, Albany, New York; 11Continuing Professional Development, American Society for Clinical Pathology, Indianapolis, Indiana
Introduction: The ASCP NonGYN Assessment Program is a glass-slide program developed with oversight by the ASCP NonGYN Assessment Committee, and includes Thyroid FNA cases. Participants choose one of the five diagnostic categories. One — Negative / Reactive / Hyperplasia / Developmental; Two — Infectious / Inflammatory Process; Three — Benign Neoplasm; Four — Lesion of Uncertain Biological Potential; and Five — Positive for Malignancy. A secondary specific interpretation is also provided. In thyroid aspirates, the diagnostic category would largely determine the clinical response: Surgical excision, in categories four and five and generally non-surgical follow-up in categories one, two, and three.
Materials and Methods: Data from five cases of thyroid malignancies and neoplasms, with a total of 1558 responses, was reviewed: Papillary carcinoma with 599 responses; Medullary carcinoma with 225 responses; and Anaplastic carcinoma with 163 responses were categorized as positive for malignancy; while follicular neoplasm with 304 responses; and hurthle cell neoplasm with 267 responses were categorized as lesion of uncertain biological potential. responses were placed into groups: Group A represented the correct diagnostic category and correct interpretation (true positives). Group B, which is a summation of the above-mentioned diagnostic categories one, two, and three, represented the incorrect diagnostic category and incorrect interpretation (false negatives). This was the group representing a major error, as it would impact the clinical management of these patients who would generally not undergo treatment by surgical excision. Group C represented the diagnostic category four, lesion of uncertain biological potential, with any incorrect interpretations. Group D represented the diagnostic category five, positive for malignancy, with incorrect interpretations. Group E presented the most common misinterpretation(s) for each case.
Results: Thyroid aspirates that were Positive for Malignancy (Papillary, Medullary, Anaplastic Carcinomas), performed well with false negative (Group B) rates of 5, 7, and 0%, respectively. Group C (Diagnostic category four) and Group D (Diagnostic category five with incorrect interpretation) represented the relatively minor errors that most probably would not significantly alter the eventual treatment and outcome. Thyroid aspirates categorized as lesions of uncertain biological potential and hurthle cell neoplasm, performed in a similar manner to positive for malignancy cases, with a false negative rate of 7% and a correct interpretation rate of 83%. 9.85% of responses of positive for malignancy with incorrect interpretation could lead to a definitive surgical procedure, which may not be indicated. follicular neoplasm, another lesion of uncertain biological potential, showed a false negative rate of 22%, which represented the incorrect diagnostic category and incorrect interpretation (Group B). 17.23% of the responses were in Group D, positive for malignancy with incorrect interpretation, which could lead to a definitive surgical procedure, which may not be indicated [Table 1].
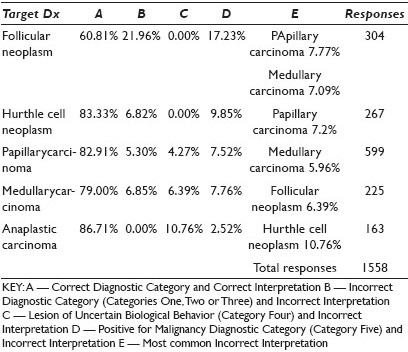
Conclusions: In summary, thyroid aspirates of Papillary carcinoma, Medullary carcinoma, Anaplastic carcinoma, and hurthle cell neoplasm, showed diagnostic sensitivity rates (Group A + Group C) of 92 – 100%, which was similar to the reported rates of around 95%. The follicular neoplasm presented as the most challenging diagnosis, with a 22% false negative rate.
75: Incidence of microcarcinomas diagnosed by ultrasound-guided fine needle aspiration in the Puerto Rican population: A prospective study
M. Garcia, MD, L. Rivera, FCAP, FASCP, W. Virella, FCAP, FASCP, R. Rodriguez, CT(ASCP), G. Villarmarzo, FCAP
Cytology, Hato Rey Pathology Associates, Inc., San Juan, Puerto Rico
Introduction: Thyroid nodules are a very common clinical finding during palpation, with an estimated prevalence that ranges from 3 to 7%. Because of their high prevalence, a cost-effective strategy for diagnosis and management of thyroid nodules becomes vital. Fine Needle Aspiration (FNA) plays an essential role in the diagnosis of thyroid disease. Ultrasound-guided FNA (US-FNA) is recommended for nodules >10 mm and suggested for nodules < 10 mm, if clinical information or US features are suspicious. Several studies demonstrate no significant difference in cancer risk in patients with nodules < 10 mm, which does not justify an arbitrary cut-off value of 10 mm. However, the behavior of microcarcinomas is controversial: Even as some of them remain indolent, a substantial number show a more aggressive course; therefore, early diagnosis and treatment of small tumors is clinically important. In order to better assess smaller incidental nodules, it is important to review pertinent clinical history as well as sonographic findings . Few studies have been conducted to evaluate the use of US-FNA in thyroid nodules < 10 mm.
Materials and Methods: The aim of the study was to perform a one-year prospective study to evaluate the use of FNA in the diagnosis of microcarcinomas and its variants in a Puerto Rican population and to correlate nodule size and sonographic characteristics with the risk of malignancy. The study includes all the patients seen in our clinics during one year, starting on July 2010, with thyroid nodules less than 10 mm in size. Our five clinics accept patients from all over the island. All USG-FNA were performed by experienced pathologists using a 23-gauge needle attached to a 20 ml syringe and pistol . Each image from the procedure date and biopsy site was evaluated by a radiologist who confirmed the nodule's size and sonographic characteristics.
Results: The preliminary results came from the data obtained from July to December 2010. Out of 280 positive cases, a total of 34 (12%) nodules resulted in incidental microcarcinomas, measuring from 1 mm up to 10 mm, with an average measurement of 4 mm. And out of the 34, 11% resulted in medullary carcinoma, and the remaining 89% were papillary microcarcinomas; 56% of the incidental microcarcinoma nodules were hypoechoic solitary nodules, whereas, nine (24%) of these nodules showed associated microscopic calcifications.
Conclusions: These preliminary results demonstrate the importance of Fine Needle Aspiration in the diagnosis of microcarcinomas and point out the fact that this type of tumor may be missed if only lesions greater than 10 mm are biopsied.
76: Thyroid fine needle aspiration reporting rates and outcomes pre- and post-bethesda implementation within a combined academic and community hospital system
Aaron Harvey, MD, Debora Smith, CT(ASCP), Dina Mody, MD, Mojgan Amrikachi, MD
Pathology and Laboratory Medicine, The Methodist Hospital, Houston, Texas
Introduction: The current study compares data from our hospital system before and after the 2008 implementation of the Bethesda System for Reporting Thyroid Cytology, to show the effects it has had on the reporting rates and outcomes for thyroid lesions. Our institution had been previously sub-classifying the ‘Suspicious for Malignancy’ category into the categories recommended by the Bethesda system. However, the ‘Atypia of Undetermined Significance or Follicular Lesion of Undetermined Significance’ (AUS / FLUS) category did not exist in our reporting lexicon prior to the Thyroid Bethesda implementation.
Materials and Methods: A search of the medical record for all thyroid fine needle aspiration biopsies (FNA) was performed for 2002 – 2005 (prior to the Bethesda recommendations) and for 2009 – 2010 (following the Bethesda implementation). The diagnostic outcomes were also reviewed for cases with available follow-up.
Results: From 2002 – 2005, a total of 2958 thyroid FNAs were performed in our hospital system with 67 (2.3%) unsatisfactory, 2514 (85.0%) negative, 261 (8.8%) suspicious for malignancy, and 116 (3.9%) positive for malignancy, upon cytological evaluation. From 2009 – 2010, a total of 2371 thyroid FNAs were performed with 38 (1.6%) unsatisfactory, 2093 (88.3%) negative, 49 (2.1) AUS / FLUS, 107 (4.5%) suspicious for malignancy, and 84 (3.5%) positive for malignancy, upon cytological evaluation [Table 1]. The AUS / FLUS and suspicious thyroid FNAs from 2009 – 2010 with available follow-up showed the following findings [Table 2]. Of the 49 cases of AUS / FLUS on cytological evaluation, 24 (49%) cases had follow-up procedures: Nine had repeat FNAs, 14 had surgical resections, and one had both repeat FNA and surgical resection. Of the nine repeat FNAs, two were AUS / FLUS, one was positive for malignancy, and one was suspicious for follicular neoplasm. Of the 14 surgical resections, three (21.4%) were positive for malignancy (papillary carcinoma) and one was Hurthle cell neoplasm of uncertain malignant potential. The case with both repeat FNA and surgical resection was benign. Of the 64 cases suspicious for follicular neoplasms, 27 had histological material for follow-up and five (18.5%) showed malignancy. Of the 22 cases suspicious for Hurthle cell neoplasm, nine had histological material for follow-up, two (22.2%) showed malignancy, and one was a Hurthle cell neoplasm of uncertain malignant potential. Of the 21 cases suspicious for malignancy, 10 had histological material for follow-up and eight (80%) showed malignancy.
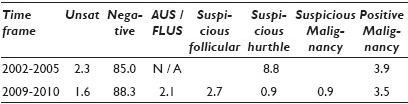
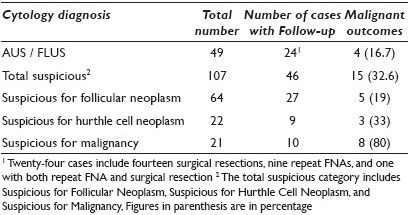
Conclusions: In conclusion, our AUS / FLUS rate of 2.1% is at the lower range of the ‘up to 7%’ recommendation of the Bethesda guidelines and our 16.7% rate of malignancy of AUS / FLUS with available follow-up is slightly above the 5 – 15% recommendation of the Bethesda guidelines. As the percentage of cases classified as suspicious (follicular neoplasm, Hurthle cell neoplasm, and malignancy) dropped from 8.8% in 2002 – 2005 to 4.5% in 2009 – 2010, we believe the 2.1% of AUS / FLUS cases in 2009 – 2010 would have probably been included within the suspicious category prior to the 2008 Bethesda implementation.
77: Review of the National cancer institute / Bethesda terminology system for thyroid cytology specimens: The New York university experience, with special focus on the indeterminate category follicular lesion of undetermined significance
Rachel Hudacko, MD1, Keith Heller, MD2, Kepal Patel, MD2, Jennifer Ogilvie, MD2, Joan Cangiarella, MD1, Aylin Simsir, MD1
1Pathology, New York University Medical Center, New York City, New York; 2Surgery, New York University Medical Center, New York City, New York
Introduction: In 2007, a National Cancer Institute (NCI)-sponsored consensus conference developed a unified ‘Bethesda Terminology System (BTS)’ for reporting thyroid fine needle aspiration (FNA) specimens. A national source of dilemma has been with the diagnosis, reporting, and treatment of the indeterminate category called ‘follicular lesion of undetermined significance (FLUS)’. Current recommendations are that the FLUS diagnostic rate should not be higher than 7%, and that FLUS should be followed up with a repeat FNA in three to six months due to the low incidence of malignancy (5 – 10%). However, follow-up (F / U) studies published since 2007, have reported malignancy rates of up to 48%. We have been using FLUS before the BTS with a special comment favoring the hyperplastic nodule (HN), follicular neoplasm (FN), or the follicular variant of papillary carcinoma (FVPC), when possible, to offer further input for clinical management. In December 2009, we officially reviewed our diagnostic criteria / terminology and adopted the BTS in 2010, as a department in its entirety, with an intention of eliminating further comments for the FLUS category. The purpose of this study is to compare our FLUS diagnostic and malignancy rates with the published data before and after 2010.
Materials and Methods: This study was confined to FLUS cases with surgical F / U divided into the pre-Bethesda (2006 – 2009) and post-Bethesda (2010) periods. The FLUS cases were further categorized into five subtypes as indicated in the original reports: FLUS not otherwise specified (NOS), FLUS favor HN, FLUS favor FN, FLUS favor FVPC, and atypia of undetermined significance (AUS). The surgical F / U diagnoses were recorded. The FLUS diagnostic and malignancy rates were calculated.
Results: In the pre-Bethesda and post-Bethesda periods, there was a total of 6053 and 2261 thyroid FNAs, respectively, both with the same FLUS diagnostic rate of 6.5%. Overall, 223 FLUS cases (41%) were surgically resected. The malignancy rates for each of the FLUS subtypes are shown in Table 1. The overall malignancy rate for the FLUS category was 48%. Of the malignant cases, 44% were FVPC, 40% were classic PC, 14% were follicular carcinoma, and 2% were medullary / other carcinoma. After exclusion of the subtypes FLUS favor FN and FLUS favor FVPC, the overall malignancy rate decreased by 8% [Table 2]. The malignancy rates were similar for cases diagnosed in both the pre- and post-Bethesda periods.

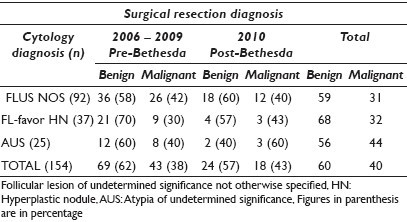
Conclusions: Our overall diagnostic rate for FLUS is similar to the published data. Our malignancy rate for FLUS is significantly higher than what is reported by the BTS, but similar to that reported by some institutions. This may partly be due to the inclusion of cases deemed worrisome for FN and FVPC in the FLUS category. Reclassification of some FLUS cases (i.e., favor FN or FVPC) into more appropriate categories as recommended by the BTS (i.e., neoplasm or suspicious for malignancy) helped to decrease the malignancy rate. Therefore, each institution must evaluate their own practice, to determine how their diagnostic criteria / categories compare to the BTS. This is essential for recommending appropriate F / U for FLUS cases. Based on the wide variation of reported FLUS diagnostic and malignancy rates, revision of the FLUS category at a future national consensus conference is warranted.
78: Fine needle aspiration of thyroid nodules in the pediatric population: A twelve-year cyto-histological correlation experience at long island Jewish medical center
Seema Lale, MD, Nora Morgenstern, MD, Lori Anderson, DO, Chiara Sugrue, MS, SCT(ASCP), Patricia Wasserman, MD, FCAP
Pathology, North Shore Long Island Jewish Health System, Lake Success, New York
Introduction: Diagnostic evaluation of thyroid nodules by fine needle aspiration (FNA) is an acceptable and cost-effective screening test to triage patients for clinical management, based on the rate of malignancy of each diagnostic category. The bethesda system for reporting thyroid cytopathology was published in 2007, by the National Cancer Institute (NCI). Using this classification, we studied our institution's experience in the pediatric population calculating the rate of malignancy for each diagnostic category, and comparing our findings to the overall patient population and that of the literature.
Materials and Methods: There were 13,312 thyroid FNAs performed at our institution between 1998 and 2010. Of these 282 cases were from patients under 19 years of age. We reviewed and reclassified these cases using the new NCI categories, and pursued a cytology-surgical follow-up.
Results: Of the 282 FNA cases, 20.92% (59) were classified as unsatisfactory (U), 48.22% (136) as benign (B), 2.12% (6) as Atypia of undetermined significance (AUS), 14.18% (40) as suspicious for follicular neoplasm (FN), 2.12% (6) suspicious for malignancy (SM), and 12.41% (35) as positive for malignancy (P). The U-category was further subclassified as the non-diagnostic (ND) 12.41% (35) and the cyst (C) 8.51% (24) category. Seventy-four children had a surgical follow-up. The rates of histologically confirmed malignancy were 10% in U (1 / 10), 0% in B (0 / 17), 50% in AUS (2 / 4), 39% in FN (7 / 18), 100% in SM (4 / 4), and 100% in the P (24 / 24) categories, respectively. Among the U category, the malignancy rate was 0% for the ND category and 25% for the C category.
Conclusions: To our knowledge, this is the first study to apply NCI categories to the pediatric population and compare the risk of malignancy in each category in the pediatric population to that of the overall population, as reported in the literature. The rate of malignancy in the U category was only seen in the specimens with cystic-component (25% malignancy rate in cysts compared to 0% in the non-diagnostic category), although only two patients had surgery in this category. The AUS and FN categories had a higher malignancy rate in our pediatric population (50 and 39%, respectively) as compared to that of the overall population reported in the literature (15 and 30%, respectively). Given that the rates of malignancy are higher for cysts and AUS in the pediatric population, the literature recommendation to ‘follow-up and repeat’ may not apply well to children, where surgery may be warranted instead. As the rate of malignancy is slightly higher for FN, the literature recommendation of diagnostic lobectomy remains sound, unless malignancy can be proven by slide re-review or frozen section, before the lobectomy is final.
79: Hashimoto thyroiditis: The great obscurer or a mere diagnostic obstacle
Alexander Finkelstein, DO, MD, Gillian Levy, MD, Constantine Theoharis, MD
Pathology, Yale University School of Medicine, New Haven, Connecticut
Introduction: Fine needle aspiration (FNA) is the modality of choice in the diagnostic workup of thyroid nodules. The inflammatory condition hashimoto thyroiditis (HT) is often encountered, and while, in and of itself, HT does not usually present a diagnostic challenge, it is associated with both epithelial and lymphocytic cytological changes that lie within the spectrum of thyroid neoplasms. Furthermore, HT is classically associated with an increased risk of certain thyroid malignancies including papillary thyroid carcinoma (PTC) and non-hodgkin lymphoma (NHL). In light of the wide spectrum of changes and the increased risk of malignancy, HT may be associated with a concurrent neoplastic process that goes unnoticed. We sought to investigate the risk of HT disguising a neoplastic process in a tertiary endocrine referral center, that is , whether the presence of HT on thyroid FNA obscures another pathological condition in the thyroid for which surgical intervention would be warranted.
Materials and Methods: Three hundred and forty-nine cases were retrieved from the Department of Pathology archive representing all cases of thyroid FNA with HT during the five-year period of January 2002 to December 2007. Cytological diagnoses ranging from HT alone, HT with follicular neoplasm (FN), to HT with PTC were represented. Surgical follow-up was available in 39 cases (11%). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated in relation to the histopathological diagnoses.
Results: Twenty-seven (69%) of the 39 operated cases or 8% out of the total 349 HT patients had a cytological diagnosis of either FN or PTC in addition to HT. In the remaining 12 cases (31%), operations were performed for cosmetic reasons. Cases where both cytological and histopathological evaluation exhibited HT with a concurrent neoplastic lesion were designated as true positives (21 cases). Cases where cytological evaluation showed HT and follow-up confirmed HT alone were designated as true negatives (7 cases). Cases diagnosed cytologically as HT with a concurrent neoplasm, but upon resection exhibited HT alone were designated as false positives (6 cases). Finally, cases where cytological evaluation displayed HT only, but where histopathology displayed as both HT and a concurrent neoplasm not detected preoperatively were designated as false negatives (5 cases). These five false negative cases included: Three PTCs, two Follicular Adenomas, and one NHL. Sensitivity in the detection of a neoplasm concurrent with HT was 81% and specificity was 54%. PPV and NPV in our patients were 78 and 58%, respectively.
Conclusions: Neoplasms concurrent with HT, while not exceedingly common, can present a diagnostic challenge. FNA has a relatively high sensitivity and PPV in the detection of these neoplasms (81 and 78%, respectively). However, as shown by the rate of false negatives in this study, the epithelial and lymphocytic cytological changes in HT may obscure the significant concurrent pathology. Therefore, the FNA diagnosis of HT demands some degree of heightened vigilance for the presence of concurrent neoplasms.
80: Interinstitutional second opinion in thyroid cytology: Should second opinion be mandated prior to definitive surgery if Fine Needle Aspiration was performed elsewhere?
Xiaosong Li, MD1, Keithe Heller, MD2, Joan Cangiarella, MD1, Aylin Simsir, MD1
1Pathology, NYU Medical Center, New York, New York; 2Endocrine Surgery, NYU Medical Center, New York, New York
Introduction: Interinstitutional consultation / second opinion (IC) for review of surgical biopsy slides, prior to definitive surgery, is a routine practice in many institutions, if the original biopsy leading to the definitive surgery has been performed elsewhere. Data on the effect of IC for cytology specimens prior to definitive surgery is somewhat sparse. Studies show major discrepancy rates varying from 7.4 to 9.3% in a variety of gynecological and non-gynecological cytology specimens. Thyroid fine needle aspiration (FNA) is one of the major specimen types leading to a change in diagnosis and patient management upon IC. The Interinstitutional diagnostic concordance rate varies from 40 to 82%. We reviewed our experience with the IC of thyroid FNAs for patients who had the FNA procedure done elsewhere and were referred to NYU for further management.
Materials and Methods: The pathology reports from all IC thyroid FNAs in 2009 and 2010 were retrieved; the original and IC diagnoses were recorded and compared. For the purpose of this study the diagnostic categories were grouped as follows, based on effect on clinical management: (1) Nondiagnostic, (2) benign, (3) atypia of undetermined significance / follicular lesion of undetermined significance (AUS / FLUS), (4) suspicious for follicular neoplasm / follicular neoplasm (susp FN / FN), (5) suspicious / positive for malignancy including papillary carcinoma and other carcinomas. The diagnostic concordance rates were calculated. Surgical follow-up was obtained when possible.
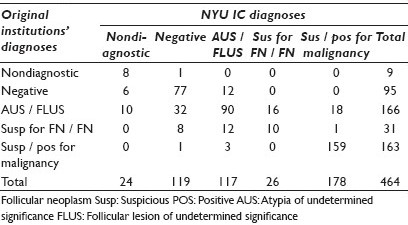
Results: Table 1 summarizes the original referral and NYU IC FNA diagnoses. The overall diagnostic concordance rate with referral institutions was 74% [Table 2]. The lowest concordance rate was within the AUS / FLUS and susp FN / FN categories. Of the AUS / FLUS cases, 19% were downgraded to benign, 6% were downgraded to unsatisfactory, and 20% were upgraded to susp FN / FN or malignant categories; therefore, within this group, patient management would potentially be altered in 46% of the cases based on the IC review. Of those who underwent surgery, 86% of the AUS / FLUS cases that were downgraded to benign were confirmed to be benign nodules on excision; one of the seven cases was papillary carcinoma. On excision, 86% of the AUS / FLUS cases upgraded to susp for FN / FN or malignant categories were confirmed to be malignant. For the susp FN / FN category, 26% were downgraded to benign, 39% were downgraded to AUS / FLUS, and 3% upgraded to malignant, potentially altering patient management in 68% of the cases. None of the cases downgraded to benign had a surgical follow-up; 67% of the cases downgraded to AUS / FLUS were papillary carcinoma on excision, whereas, 33% were confirmed to be benign. The single case upgraded to malignancy in this group was papillary carcinoma on excision. Malignancy rates on surgical excision are summarized in Table 3.
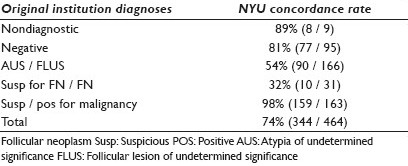
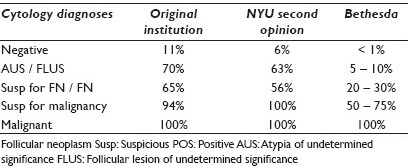
Conclusions: (1) The greatest diagnostic concordance with referring institutions is with the unsatisfactory, benign, and susp / positive for malignancy categories. The least diagnostic concordance is with the AUS / FLUS and susp for FN / FN diagnostic categories. (2) The IC review in AUS / FLUS and susp for FN / FN cases can lead to significant changes in management; therefore, IC should be undertaken whenever possible. Based on the surgical outcome results and cytological diagnostic discordance, these lesions continue to pose significant diagnostic and management challenges. (3) The malignancy rates in most diagnostic categories are higher in this study compared to the published Bethesda data. This may be, in part, due to the selection bias, as cases sent for second opinion / surgery may reflect those patients with higher risk of malignancy based on clinical / radiologic findings.
81: Application of the Hybrid Capture-2 assay to squamous cell carcinomas of the head and neck: A convenient liquid-based approach for the reliable determination of HPV status
Zahra Maleki, MD1, Justin Bishop, MD1, Alexander Valsamakis, MD, PhD1, Xiaofei Chang, MD2, Sara Pai, MD2, William Westra, MD1
1Pathology, The Johns Hopkins Hospital, Baltimore, Maryland; 2Otolaryngology, The Johns Hopkins Hospital, Baltimore, Maryland
Introduction: A growing proportion of head and neck squamous cell carcinomas (HNSCCs) are caused by the human papillomavirus (HPV). In light of the unique natural history and prognosis of these HPV-related HNSCCs, routine HPV testing is being incorporated into the diagnostic protocols. Accordingly, there is an escalating demand for an optimal detection strategy that is sensitive and specific, transferrable to the diagnostic laboratory, standardized across laboratories, cost-effective, and amendable to broad application across specimen types including cytological preparations.
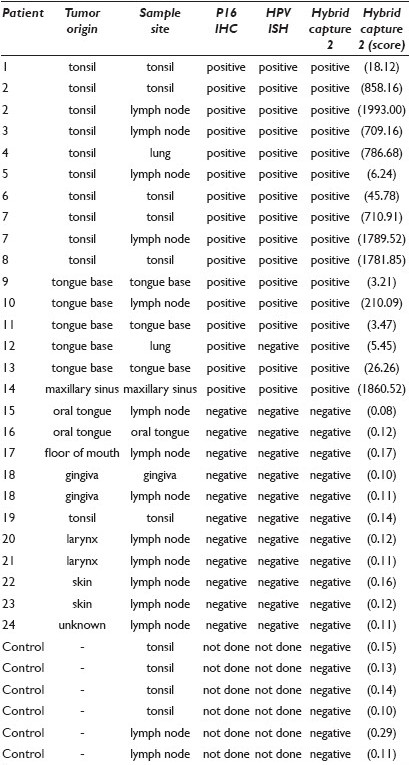
Materials and Methods: Cytological preparations (fine needle aspirates and brushes) were obtained from surgically resected HNSCCs and evaluated for the presence of high-risk HPV using the Hybrid Capture 2 assay. HPV analysis was also performed on the corresponding tissue sections using HPV in-situ hybridization and p16 immunohistochemistry. In cases where the immunohistochemical and in-situ hybridization results were discordant, HPV status was determined by real time PCR detection of E6 and E7 expression. HPV status in the tissue sections and corresponding cytological samples were compared. Twenty-four patients who had undergone resection of a primary and / or metastatic HNSCC were selected. During routine surgical pathology dissection of the specimens, the tumor was identified and aspirated or brushed. These FNA specimens were evaluated cytologically (Diff Quick stained air-dried smears) for the presence of tumor cells and overall sample cellularity. Four brushes from the non-neoplastic tonsils and two FNAs from the benign lymph nodes were used as HPV negative controls. All together, 27 cytological preparations from 24 patients were evaluated for high-risk HPV using the Hybrid Capture 2 assay. The HPV status was confirmed in the formalin-fixed and paraffin-embedded tissue sections of the resected HNSCCs. Immunohistochemical analysis targeted the expression of a biomarker of HPV E7 oncoprotein activity, the CDK-inhibitor p16. Tumor blocks were evaluated for the presence of HPV DNA by in-situ hybridization that captured HPV genotypes 16, 18, 33, 35, 45, 51, 52, 56, and 66.
Results: There was a strong agreement for the HPV status across the various methods of HPV analysis. All 13 HNSCCs that were p16 positive by immunohistochemistry and HPV positive by in-situ hybridization (p16+ / HPV+) were HPV positive by Hybrid Capture 2 assay analysis. Conversely, the 10 HNSCCs that were p16- / HPV- were negative by Hybrid Capture 2 assay analysis. The single discordant case (p16+ / HPV-) was found to be HPV positive using the Hybrid Capture 2 assay. Using real-time PCR amplification of the viral oncoprotein E7, the presence of HPV 16 in this case was confirmed at 1.02 copies of HPV 16 / genome equivalent. Based on the benchmark HPV testing of the tissue sections, 14 HNSCCs were classified as HPV positive and 10 as HPV negative. All the corresponding cytological preparations were correctly classified using the Hybrid Capture 2 assay.
Conclusions: The Hybrid Capture 2 strategy, already in widespread use for the detection of high-risk HPV in cervical brushes, is readily transferrable to HNSCCs. Consistent accuracy in cytological preparation suggests its potential application in FNAs from patients who present with lymph node metastases, and may eliminate the need to obtain a tissue, solely for the purpose of HPV testing.
82: Atypia of undetermined significance: Institutional experience with the Bethesda system
Matthew Olson, MD, Douglas Clark, MD, Yener Erozan, MD, Syed Ali, MD
Department of Pathology, The Johns Hopkins Hospital, Baltimore, Maryland
Introduction: Atypia of undetermined significance (AUS) is one of the least well-understood diagnostic categories within the bethesda system (TBS). As all the eight different scenarios lead to the categorization of AUS, and these range from sample preparation artifact to rare focal nuclear atypia, it follows that the likelihood of malignancy in these nodules would differ. This study is a correlation of the resection specimens from 95 patients with no worse than an AUS diagnosis from a fine needle aspirate (FNA) of the thyroid.
Materials and Methods: The frequencies of TBS categories were calculated from 3,956 thyroid FNAs, interpreted over a 26-month period at a major tertiary care center since the adoption of TBS for reporting thyroid cytopathology. The mmorphological criteria of TBS were applied strictly. The breakdown of TBS diagnoses is given in Figure 1. Resection and cyto–histo correlation was performed on 95 cases of AUS.
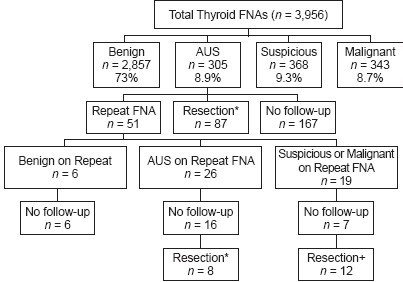
- The breakdown of the Bethesda System categories along with the frequencies of repeat FNA at our institution and the rates of diagnosis for the second FNA. *The 95 cases in our cyto–histo correlation were derived from the two categories with gray boxes. + Cases with a second FNA that were interpreted as malignant or suspicious for malignancy were not counted as AUS in the correlation with the cytopathology.
Results: The rate of false negative diagnoses in our series was 4.8% (11 / 237). Odds ratios and relative risks for this data are listed in Table 1. In thyroidectomies performed after the worst diagnosis of AUS (n = 95), 31 (33%) of them had stageable (not incidental microcarcinoma) carcinoma on resection (OR: 10.0, CI: 4.78 – 21.08). Our review disclosed two salient subcategories of AUS: Those with focal nuclear atypia, and those with focal microfollicular features. Of the subset of AUS with nuclear atypia (n = 36), 47% had stageable carcinoma on resection (OR: 18.6, CI: 7.6 – 45.2). When the AUS with nuclear atypia group was separated out, this group demonstrated a significantly higher risk of malignancy that the other forms of AUS (OR: 2.87, CI: 1.18 – 6.99). In contrast, the microfollicular features did not differ significantly from the other forms of AUS (OR: 1.61, CI: 0.57 – 4.54).

Conclusions: Although nuclear atypia and microfollicular features are both morphological subsets of AUS, in terms of clinical significance, nuclear atypia correlates more with the risk of stageable carcinoma on resection. These findings support the conclusion that AUS is a heterogeneous yet clinically valid diagnosis, with a significantly higher risk for stageable carcinoma on resection. Additionally, AUS with nuclear atypia is independently correlated with a higher risk for stageable carcinoma on resection.
83: Atypia of undetermined significance in thyroid fine needle aspiration predicts the absence of features associated with aggressive behavior for papillary thyroid carcinoma
Paul VanderLaan, MD, PhD, Jeffrey Krane, MD, PhD
Pathology, Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts
Introduction: The vast majority of malignancies identified by thyroid fine needle aspiration (FNA) are papillary thyroid carcinoma (PTC), a cancer with an excellent overall prognosis. We had previously noted a high percentage of follicular variants among the PTCs identified following an AUS diagnosis. Here, we set out to determine if other features of PTC, particularly those associated with a more aggressive clinical behavior, correlate with the preceding cytological diagnosis.
Materials and Methods: Thyroid FNAs performed at our hospital from January 2005 through May 2010 were correlated with subsequent histopathological findings. FNAs were evaluated by staff cytopathologists using a six-tiered Bethesda-like reporting system. The FNA diagnoses that were evaluated in this study were malignant (POS), suspicious for malignancy (SUS), and atypia of undetermined significance (AUS). Only the diagnosis for the targeted nodule was considered. Nodules diagnosed as PTCs were classified as being high-risk subtypes (tumors having tall cells, columnar, and / or diffuse sclerosing features), follicular variants, conventional variants, or other subtypes not in the high-risk subcategory. The following clinical parameters were also assessed for PTCs: Tumor size, the AJCC TNM stage, multifocality, lymphovascular invasion, extrathyroidal extension, and recurrence / metastasis after surgery.
Results: For this study period, 168 thyroid nodules were resected following a single or repeat diagnosis on FNA of AUS; 202 nodules for a SUS FNA, and 192 thyroid nodules for a POS FNA. Malignancy was identified in 56 (33%) of the AUS cases, including six minimally invasive follicular carcinomas (only one with lymphovascular invasion) and one lymphoma (following a diagnosis of atypical lymphoid cells). PTC was confirmed in 49 (29%) of the AUS FNAs, 163 (81%) of the SUS FNAs, and 183 (95%) of the POS FNAs. The mean size of the resected PTCs did not differ between the FNA-diagnosis groups (AUS: 2.0 ± 1.2 cm, SUS: 2.1 ± 1.4 cm, POS: 1.9 ± 1.1 cm), nor did the likelihood of a multifocal disease (AUS and SUS: 55%; POS: 63%). However, the PTCs following an AUS FNA were less likely to have properties associated with aggressive behavior. No aggressive variants of PTC were identified with the AUS category. AUS-associated PTCs were more likely to be a lower AJCC T stage, to be a lower AJCC N stage (all AUS-associated PTCs were N0) and to lack lymphovascular invasion or extrathyroidal extension [Table 1]. All T3 PTCs associated with AUS were > 4 cm, with one also having extrathyroidal extension. Only two PTCs had distant metastasis at the time of surgery, and 16 patients later went on to develop recurrence and / or distant lymph node metastasis after surgery; all these cases had a POS FNA diagnosis preceding surgery.
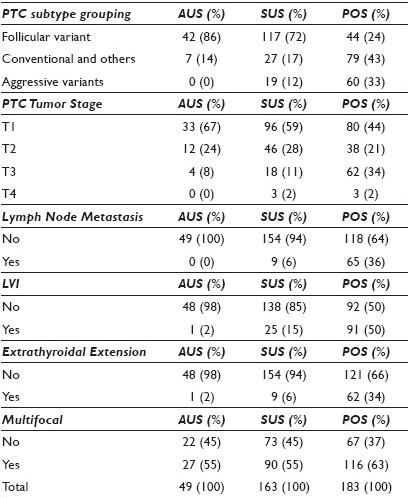
Conclusions: This study indicates that the probabilistic-based Bethesda system for reporting thyroid cytopathology not only conveys the risk that a thyroid nodule is malignant, but also predicts the presence of pathological risk factors associated with aggressive biological behavior when the malignancy is PTC. AUS diagnoses identify low-risk PTCs, most of which are follicular variants. These findings suggest that a more conservative clinical approach for nodules diagnosed repeatedly as AUS, particularly those of small size, may represent a reasonable alternative to immediate surgery.
84: Can cytomorphology further stratify thyroid fine needle aspirates diagnosed as follicular lesion of undetermined significance?
Ann Walts, MD, Catherine Bresee, MS, Shikha Bose, MD
Pathology and Laboratory Medicine, Cedars-Sinai Medical Center, Los Angeles, California
Introduction: Fine needle aspiration (FNA) provides a cost-effective method for the triage of thyroid nodules, but inconsistent terminology and low levels of diagnostic agreement have been problematic. The bethesda system for reporting thyroid cytopathology (TBS-T) was created to standardize the criteria and terminology for thyroid FNA reporting into six categories, each with an assigned ‘risk of malignancy’. Follicular lesion of undetermined significance (FLUS), with an assigned 5 – 10% risk of malignancy, is the most frequent abnormal diagnosis rendered in thyroid FNAs. TBS-T recommends that the FLUS not exceed 7% of thyroid FNA diagnoses; however, this percentage varies widely across cytopathologists and laboratories. In our laboratory, FLUS comprises of 10% of the thyroid FNA diagnoses. Stratification of FLUS could benefit patient management. This retrospective study of cases diagnosed as FLUS was designed to determine if cytomorphology could predict carcinoma (CA) in the subsequent thyroidectomy.
Materials and Methods: Eighty-three consecutive cases diagnosed as FLUS on FNA and subsequently resected were retrieved from our files. The patients ranged from 27 to 77 years in age; 76% were female. The final diagnostic groups (benign vs. malignant) were compared for age, gender, interval between FNA and resection, and the presence of cell sheets, microfollicles, nuclear grooves / irregular nuclear membranes (NG), nuclear overlap / crowding (NC), nuclear enlargement (NE), nuclear pseudoinclusions (NI), bland / compact chromatin, Hurthle change, lymphocytes, and colloid as described in the cytology reports. The confounding effects of subjective terms (e.g., rare, few, some, focal) were eliminated by scoring each feature on a binary scale (present or absent). Statistical analyses were performed using the SAS software.
Results: Histological diagnoses of the aspirated thyroid nodules (median 1.8 cm) included 58 benign, 21 CAs (10 follicular variants of papillary CA (FVPTC), five CAs with mixed papillary / follicular patterns, three classical papillary CAs, two minimally invasive follicular CAs, one anaplastic CA), and four neoplasms of undetermined malignant potential. For statistical analysis, these four cases were included in the malignant group. Comparison of the FNAs from the benign and malignant cases showed significant differences (P < 0.5) in the frequencies of the four features studied — NG, NC, NI, and Hurthle change — between the two groups [Table 1]. When each predictor was considered independently using unadjusted analysis with logistic regression, NG and NC emerged as significant predictors of CA. Ten (66.7%) of the 15 cases with NG and 15 (62.5%) of the 24 cases with NC were malignant on excision. The presence of NC showed a strong positive correlation with the presence of NG, NI, and NE (Spearman rank correlations). In a forward step-wise selected, adjusted, logistic regression analysis, an increased risk of malignancy on excision was only associated with NC. Thyroid malignancy was present in 17 (61%) of the 28 cases whose FNAs exhibited ≥ 1 of the three significant cytological features [Table 2].

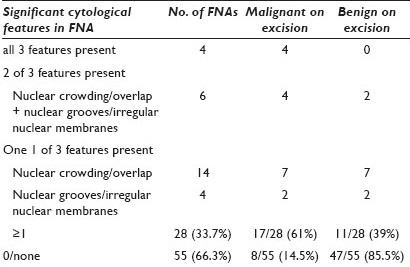
Conclusions: The follicular variant of papillary thyroid carcinoma (FVPTC) is the most frequent CA identified in thyroidectomies following an FNA diagnosis of FLUS.
-
The presence of NG, NI, and / or NC in FNAs diagnosed as FLUS was associated with malignancy in 61% of the subsequent thyroidectomies. These FNAS were best diagnosed as suspicious for malignancy to which TBS-T assigned the risk of malignancy as 50 – 75%.
-
Large prospective studies are needed to confirm our findings.
85: Web-based laboratory provider outreach tool to ease transition to the Bethesda system for reporting thyroid cytopathology
Scott Whitworth, MD
Department of Pathology, Walter Reed National Military Medical Center, Bethesda, Maryland
Introduction: The 2010 bethesda system for reporting thyroid cytopathology provides a framework for uniform interpretation of thyroid fine needle aspiration cytology. For some laboratories, adoption of this new reporting framework may require a significant adjustment in terminology and report format. This may create confusion for providers and uncertainty regarding treatment recommendations in some instances. The Bethesda System for reporting thyroid cytopathology allows flexibility in the reporting framework for each laboratory to tailor its interpretations and format, to meet the needs of its providers. This flexibility may lead to modified terminology and long explanatory commenting in individual aspiration reports. A prototype web application was developed to enhance the adoption of the bethesda system for reporting thyroid cytopathology, standardize interpretation commenting, and improve the laboratory-clinician outreach.
Materials and Methods: A web-based application was written in the Python programming language against the Django web-development framework, using open-source technology and modern programming practices, including source control and unit-testing. Application data was stored in SQLite. The application presented the providers with a list of diagnostic categories and specific diagnoses used by the laboratory. Pages for the selected diagnosis included laboratory-specific explanatory comments and recommendations for clinical management. External links included reference abstracts on Pubmed.gov, diagnosis-specific image sets in the online atlas of the bethesda system for reporting thyroid cytopathology, and management recommendations in the american thyroid association professional guidelines. the application is deployed on an inexpensive virtual private server using an open-source web server stack consisting of an Ubuntu linux operating system and Nginx web server.
Results: A functional demonstration is available at http//www.scottwhitworth.com/thyroid/. The source code is available under a free software license and is hosted on a popular code sharing and collaboration site where it is under active development. Current development efforts are focused on user-facing design and experience improvement. Application utilization and provider satisfaction studies are planned.
Conclusions: Adoption of the bethesda system for reporting thyroid cytopathology may cause a significant adjustment in former reporting terminology and create confusion for providers. This tool provides a low-cost solution for laboratory-clinician outreach, and reduces the need for lengthy explanatory comments in individual thyroid fine needle aspiration reports. The introduction of powerful web development frameworks for popular scripting languages and the open-source climate of today's internet, reduces the cost and expertise barriers to produce laboratory web tools.
86: Do smears contribute to the diagnosis of thyroid fine needle aspiration preparations?
Heather Wilgenbusch, CT(ASCP), MP(ASCP), Gail Mueller, MS, CT(ASCP), DLM, Nola Munasifi, MD, Margaret Neal, MD
Ketchum Wood and Burgert, Pathology Associates, Tallahassee, Florida
Introduction: Three types of cytological specimen preparations (two types of liquid-based preparations and prepared smears) are commonly used to diagnose thyroid fine needle aspiration (T-FNA). At present, there is lack of consensus as to which of these preparations is most influential in the diagnosis of FNAs or whether considering the three methods in conjunction might have a synergistic effect on the diagnosis. For example, the two liquid-based preparations (LBPs) provide an additional diagnostic tool with complementary morphological features. The standard procedure in our laboratory is to prepare one ThinPrep® (Hologic) and one SurePath® (BD) from the needle rinse in addition to reviewing two to eight smears (air-dried, Romanowsky stain and fixed, Papanicalou stain) provided by the clinician. The purpose of this study is to measure how closely the diagnoses based on LBPs reviewed alone correspond to our original diagnoses based on a combination of LBPs and smears.
Materials and Methods: Seven cytotechnologists and seven pathologists reviewed 272 archived liquid-based slides from 136 T-FNA cases received sequentially over a two-month period. These review diagnoses were based on liquid-based preparations alone and were compared to the original archived diagnoses, which were based on a review of liquid-based slides and clinician-prepared smears. The original diagnosis served as a reference point because it contained a composite of cytological material and more complete clinical information. The review diagnosis was blind to the original diagnosis and limited patient history was provided along with the ultrasound report, when available. The two LBPs were diagnosed separately, but were not blinded to each other. Diagnoses were based upon the bethesda system for reporting thyroid cytopathology. Comparison of the original diagnosis and review diagnosis was evaluated according to a scoring grid based on one- and two-step discrepancies.
Results: Comparison of the diagnoses revealed that 79.8% of the review diagnoses made using only LBPs corresponded exactly with the original diagnoses made on smears and LBPs, and an additional 17.8% of the diagnoses made on these LBPs reflected the original diagnosis within one step of the diagnostic category. All unsatisfactory cases in the original diagnoses were correctly identified, while 1.7% of the cases were two-step discrepancies based on the original diagnosis (six by cytotechnologists and three by pathologists) and 0.7% of the cases showed > 2-step discrepancies (four by cytotechnologists). A histological follow-up was available for only two cases.
Conclusions: LBPs reproduced the diagnoses of FNAs when compared with LBPs and submitted smears in 98% of the cases within one step in this study of 136 sequential T-FNAs. This study supports the previous findings that the use of liquid-based preparations alone provides sufficient material for the evaluation of FNAs. The inclusion of prepared smears added another dimension for review, with minor resultant differences in the interpretation, in 2% of our cases. LBPs offered advantages over smear preparations of a more standard preparation, ease of additional preparations for stains or molecular studies, and a clearer cellular detail, with no apparent disadvantage in diagnostic material, in this study.








